Vortioxetine
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /vɔːrtiˈɒksətiːn/ vor-tee-OK-sə-teen |
| Trade names | Trintellix, Brintellix, others |
| Other names | Lu AA21004, Vortioxetine hydrobromide (JAN JP), Vortioxetine hydrobromide (USAN US) |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a614003 |
| License data |
|
| Pregnancy category | |
| Routes of administration | By mouth |
| Drug class | Selective serotonin reuptake inhibitor (SSRI)[3] |
| ATC code | |
| Legal status | |
| Legal status | |
oxidation[12] | |
| Elimination half-life | 66 hours[12] |
| Excretion | 59% in urine, 26% in feces[12] |
| Identifiers | |
| |
JSmol) | |
| |
| |
| (verify) | |
Vortioxetine, sold under the brand names Trintellix and Brintellix among others, , is an
Common
It was approved for medical use in the United States in 2013.[14][19] In 2020, it was the 243rd most commonly prescribed medication in the United States, with more than 1 million prescriptions.[20][21]
Medical uses
Vortioxetine is used as a treatment for
Vortioxetine is also used

Contraindications
Vortioxetine is contraindicated in those taking monoamine oxidase inhibitors (MAOIs) due to the possibility of serotonin syndrome.[10]
Adverse effects
| Side effect | Placebo | Vortioxetine | Duloxetine | |||
|---|---|---|---|---|---|---|
| 5 mg/day | 10 mg/day | 15 mg/day | 20 mg/day | 60 mg/day | ||
| Any | 62% | 66% | 67% | 70% | 73% | 77% |
| Nausea | 9% | 21% | 26% | 32% | 32% | 36% |
| Vomiting | 1% | 3% | 5% | 6% | 6% | 4% |
| Diarrhea | 6% | 7% | 7% | 10% | 7% | ? |
| Constipation | 3% | 3% | 5% | 6% | 6% | 10% |
Dry mouth
|
6% | 7% | 7% | 6% | 8% | ? |
| Flatulence | 1% | 1% | 3% | 2% | 1% | ? |
| Dizziness | 6% | 6% | 6% | 8% | 9% | ? |
Abnormal dreams
|
1% | <1% | <1% | 2% | 3% | ? |
Itching
|
1% | 1% | 2% | 3% | 3% | ? |
| Notes: Vortioxetine and | ||||||
The most common side effects reported with vortioxetine are nausea, vomiting, constipation, and sexual dysfunction, among others.[10] With the exceptions of nausea and sexual dysfunction, these side effects were reported by less than or equal to 10% of study participants given vortioxetine.[10][38] Significant percentages of placebo-treated participants also report these side effects.[10][38] Discontinuation of treatment due to adverse effects in clinical trials was 8% with vortioxetine versus 3% with placebo.[38]
| Quantification method | Group | Placebo | Vortioxetine | Duloxetine | |||
|---|---|---|---|---|---|---|---|
| 5 mg/day | 10 mg/day | 15 mg/day | 20 mg/day | 60 mg/day | |||
| Measured by ASEX
|
Men | 14% | 16% | 20% | 19% | 29% | 26% |
| Women | 20% | 22% | 23% | 33% | 34% | 28% | |
| Spontaneously reported | Men | 2% | 3% | 4% | 4% | 5% | ? |
| Women | <1% | <1% | 1% | <1% | 2% | ? | |
| Notes: Vortioxetine and duloxetine (an SNRI) were directly compared in randomized clinical trials. | |||||||
Significant changes in
However reports have come in from users regarding weight gain/loss since the approval of Vortioxetine.Based on preliminary clinical studies, vortioxetine may cause less emotional blunting than SSRIs and SNRIs.[40][41]
If vortioxetine is used in combination with other serotonergic drugs like MAOIs or SSRIs, this may result in serotonin syndrome.[10]
Interactions
Vortioxetine is metabolized primarily by the cytochrome P450 enzyme CYP2D6.[12] Inhibitors and inducers of CYP2D6 may modify the pharmacokinetics of vortioxetine and necessitate dosage adjustments.[12]
Bupropion, a strong CYP2D6 inhibitor, has been found to increase peak levels of vortioxetine by 2.1-fold and total vortioxetine levels by 2.3-fold (bupropion dosed at 300 mg/day and vortioxetine dosed at 10 mg/day).[12] The incidence of side effects with vortioxetine, like nausea, headache, vomiting, and insomnia, was correspondingly increased with the combination.[12] Other strong CYP2D6 inhibitors, like fluoxetine, paroxetine, and quinidine, may have similar influences on the pharmacokinetics of vortioxetine, and it is recommended that the dosage of vortioxetine be reduced by half when it is administered in combination with such medications.[12][10] Lesser interactions have additionally been identified for vortioxetine with the cytochrome P450 inhibitors ketoconazole and fluconazole.[12]
Rifampicin, a strong and broad cytochrome P450 inducer (though notably not of CYP2D6), has been found to decrease peak levels of vortioxetine by 51% and total levels of vortioxetine by 72% (rifampicin dosed at 600 mg/day and vortioxetine at 20 mg/day).[12] Similar influences on vortioxetine pharmacokinetics may also occur with other strong cytochrome P450 inducers like carbamazepine and phenytoin.[12] As such, it is recommended that increasing vortioxetine dosage be considered when it is given in combination with strong cytochrome P450 inducers.[12] The maximum recommended dose should not exceed three times the original vortioxetine dose.[12][10]
Vortioxetine and its metabolites show no meaningful interactions with a variety of assessed cytochrome P450 enzymes and transporters (e.g., P-glycoprotein) and hence vortioxetine is not expected to importantly influence the pharmacokinetics of other medications.[10][12]
The combination of vortioxetine with MAOIs, including other MAOIs like
Pharmacology
Pharmacodynamics
| Target | Affinity | Functional activity | Action | |
|---|---|---|---|---|
| Ki (nM) | IC50 / EC50 (nM) | IA (%) | ||
| SERT | 1.6 | 5.4 | – | Inhibition |
| NET | 113 | – | – | Inhibition |
| 5-HT1A | 15 | 200 | 96 | Agonist |
| 5-HT1B | 33 | 120 | 55 | Partial agonist |
| 5-HT1D | 54 | 370 | – | Antagonist |
| 5-HT2C | 180 | – | – | – |
| 5-HT3A | 3.7 | 12 | – | Antagonist |
| 5-HT7 | 19 | 450 | – | Antagonist |
β1-adr.
|
46 | – | – | – |
| Note: No significant activities at 70 other molecular targets (>1,000 nM) (including, e.g., the DAT). Sources: [42][43] | ||||
Vortioxetine increases
It has been claimed that the
Vortioxetine at 5 mg/day may produce antidepressant effects and result in SERT occupancy as low as 50%.[12][45][48] This is in apparent contrast to SSRIs and SNRIs, which appear to require a minimum of 70 to 80% occupancy for antidepressant efficacy.[12][45][49] These findings are suggestive that the antidepressant effects of vortioxetine may be mediated by serotonin receptor interactions in addition to serotonin reuptake inhibition.[12][45] A study found no significant occupancy of the 5-HT1A receptor with vortioxetine at 30 mg/day for 9 days, which suggests that at least this specific serotonin receptor may not be involved in the clinical pharmacology of vortioxetine.[45][13][47] However, methodological concerns were noted that may limit the interpretability of this result.[45][47][13] Occupancy of other serotonin receptors like 5-HT3 and 5-HT7 by vortioxetine in humans does not seem to have been studied.[18][45] In relation to the preceding, the contribution of serotonin receptor interactions to the antidepressant effects of vortioxetine is unknown and remains to be established.[12][10][18][17] Uncertainties remain about whether vortioxetine is indeed a clinically multimodal antidepressant or whether it is effectively "[just] another selective serotonin reuptake inhibitor".[17][18]
Antagonism of the 5-HT3 receptor has been found to enhance the increase in brain serotonin levels produced by serotonin reuptake inhibition in animal studies.[45][13] Whether or not the 5-HT3 receptor antagonism of vortioxetine likewise does this in humans or contributes to its clinical antidepressant efficacy is unclear.[17][18] SSRIs and 5-HT1A receptor agonists often produce nausea as a side effect, whereas 5-HT3 receptor antagonists like ondansetron are antiemetics and have been found to be effective in treating SSRI-induced nausea.[45] It was thought that the 5-HT3 receptor antagonism of vortioxetine would reduce the incidence of nausea relative to SSRIs.[45] However, clinical trials found significant and dose-dependent rates of nausea with vortioxetine that appeared to be comparable to those found with the SNRI duloxetine.[10][18]
Pharmacokinetics


Vortioxetine is well-
The apparent volume of distribution of vortioxetine is large and ranges from 2,500 to 3,400 L after single or multiple doses of 5 to 20 mg vortioxetine, with extensive extravascular distribution.[12][38] The plasma protein binding of vortioxetine is approximately 98 or 99%, with about 1.25 ± 0.48% free or unbound.[12][10][13]
Vortioxetine is extensively
The estimated total
Pharmacogenomics
Chemistry
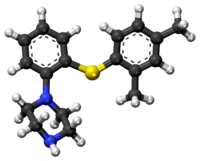
Vortioxetine (1-[2-(2,4-dimethylphenylsulfanyl)phenyl]piperazine) is a bis-aryl-sulfanyl amine as well as
History

Vortioxetine was discovered by scientists at Lundbeck who reported the rationale and synthesis for the drug (then called Lu AA21004) in a 2011 paper.[43][45]
In 2007, the compound was in Phase II clinical trials, and Lundbeck and Takeda entered into a partnership in which Takeda paid Lundbeck $40 million up-front, with promises of up to $345 million in milestone payments, and Takeda agreed to pay most of the remaining cost of developing the drug. The companies agreed to co-promote the drug in the US and Japan, and that Lundbeck would receive a royalty on all such sales. The deal included another drug candidate, tedatioxetine (Lu AA24530), and could be expanded to include two other Lundbeck compounds.[53]
Vortioxetine was approved by the U.S. Food and Drug Administration (FDA) for the treatment of major depressive disorder (MDD) in adults in September 2013,[54] and it was approved in the European Union later that year.[55]
Society and culture
It is made by the pharmaceutical companies Lundbeck and Takeda.[10]
Names
Vortioxetine was previously sold under the brand name Brintellix in the United States, but in May 2016, the US Food and Drug Administration (FDA) approved a name change to Trintellix in order to avoid confusion with the blood-thinning medication Brilinta (ticagrelor).[56] Other brand names include Vantaxa, Torvox, Voxigain, Trivoxetin, Trintellix etc.
Research
Vortioxetine was under development for the treatment of
References
- ^ "Brintellix (vortioxetine (as hydrobromide)) Product Information" (PDF). Therapeutic Goods Administration.
- ^ "Updates to the Prescribing Medicines in Pregnancy database". Therapeutic Goods Administration (TGA). Australian Government. 12 May 2022. Retrieved 13 May 2022.
- ^ a b "Vortioxetine Tablet - Uses, Side Effects, and More". WebMD. Retrieved 13 April 2024.
- FDA. Retrieved 22 October 2023.
- ^ "Product Information Brintellix" (PDF). Therapeutic Goods Administration (TGA). Australian Government.
- ^ "AusPAR: Vortioxetine hydrobromide". Therapeutic Goods Administration (TGA). Australian Government.
- ^ "Prescription medicines: registration of new chemical entities in Australia, 2014". Therapeutic Goods Administration (TGA). 21 June 2022. Retrieved 10 April 2023.
- ^ Anvisa (31 March 2023). "RDC Nº 784 - Listas de Substâncias Entorpecentes, Psicotrópicas, Precursoras e Outras sob Controle Especial" [Collegiate Board Resolution No. 784 - Lists of Narcotic, Psychotropic, Precursor, and Other Substances under Special Control] (in Brazilian Portuguese). Diário Oficial da União (published 4 April 2023). Archived from the original on 3 August 2023. Retrieved 16 August 2023.
- ^ "Brintellix tablets 5, 10 and 20mg - Summary of Product Characteristics (SmPC)". (emc). 11 April 2022. Retrieved 19 December 2022.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa "Trintellix- vortioxetine tablet, film coated". DailyMed. 26 July 2019. Retrieved 16 November 2020.
- ^ "Brintellix EPAR". European Medicines Agency (EMA). 17 September 2018. Retrieved 15 January 2021.
- ^ PMID 29189941.
- ^ ISBN 9781118788523.
- ^ a b c d e f g h i j k "Vortioxetine Hydrobromide Monograph for Professionals". Drugs.com. American Society of Health-System Pharmacists. Retrieved 18 March 2019.
- ISBN 9780857113382.
- ^ "Vortioxetine". go.drugbank.com. Retrieved 2 July 2021.
- ^ S2CID 21642202.
- ^ PMID 25562777.
- S2CID 5987668.
- ^ "The Top 300 of 2020". ClinCalc. Retrieved 7 October 2022.
- ^ "Vortioxetine - Drug Usage Statistics". ClinCalc. Retrieved 7 October 2022.
- S2CID 195192772.
- PMID 29477251.
- S2CID 43104089.
- S2CID 40432194.
The authors suggest that vortioxetine is currently a good second-line antidepressant option and shows promise, pending additional long-term data, to become a first-line antidepressant option.
- S2CID 21501578.
- PMID 26316764.
- PMID 28677828.
- PMID 35356713.
- PMID 25851751.
- PMID 27143896.
- PMID 31784448.
- S2CID 11855728.
- PMID 34038400.
- PMID 33343351.
- ^ PMID 26035185.
- ^ PMID 25575488.
- ^ S2CID 9721842.
- PMID 29344340.
- PMID 33516560.
- S2CID 4572360.
- ^ S2CID 54253895.
- ^ PMID 21486038.
- ^ "Lundbeck's "Serotonin Modulator and Stimulator" Lu AA21004: How Novel? How Good? - GLG News". Archived from the original on 24 July 2011.
- ^ PMID 25016186.
- PMID 26174134.
- ^ S2CID 44631551.
- S2CID 17263858.
- S2CID 30529325.
- PMID 28941196.
- ^ PMID 31094901.
- ^ "Australian Public Assessment Report for vortioxetine hydrobromide" (PDF). p. 11. Archived (PDF) from the original on 1 August 2017. Retrieved 5 May 2018.
- ^ Beaulieu D (5 September 2007). "Lundbeck, Takeda enter strategic alliance for mood disorder, anxiety drugs". First Word Pharma. Archived from the original on 10 October 2016.
- ^ "FDA approves new drug to treat major depressive disorder". U.S. Food and Drug Administration Press Announcement. Archived from the original on 3 October 2013.
- ^ "Brintellix". European Medicines Agency. Archived from the original on 26 January 2016. Retrieved 19 January 2016.
- ^ "Safety Alerts for Human Medical Products - Brintellix (vortioxetine): Drug Safety Communication - Brand Name Change to Trintellix, to Avoid Confusion With Antiplatelet Drug Brilinta (ticagrelor". U.S. Food and Drug Administration (FDA). Archived from the original on 5 May 2016. Retrieved 2 May 2016.
- S2CID 4768865.
- S2CID 73498106.
- ^ a b c "Vortioxetine - Lundbeck". AdisInsight. Springer Nature Switzerland AG.
- S2CID 37489812.
- S2CID 241004816.
- PMID 31780961.
