X-ray

X-ray (or much less commonly, X-radiation) is a high-energy electromagnetic radiation. In many languages, it is referred to as Röntgen radiation, after the German scientist Wilhelm Conrad Röntgen, who discovered it in 1895[1] and named it X-radiation to signify an unknown type of radiation.[2]
X-ray
X-rays can penetrate many solid substances such as construction materials and living tissue, so X-ray
History
Pre-Röntgen observations and research
Before their discovery in
The earliest experimenter thought to have (unknowingly) produced X-rays was
When Stanford University physics professor Fernando Sanford created his "electric photography", he also unknowingly generated and detected X-rays. From 1886 to 1888, he studied in the Hermann von Helmholtz laboratory in Berlin, where he became familiar with the cathode rays generated in vacuum tubes when a voltage was applied across separate electrodes, as previously studied by Heinrich Hertz and Philipp Lenard. His letter of 6 January 1893 (describing his discovery as "electric photography") to the Physical Review was duly published and an article entitled Without Lens or Light, Photographs Taken With Plate and Object in Darkness appeared in the San Francisco Examiner.[7]
Starting in 1888, Philipp Lenard conducted experiments to see whether cathode rays could pass out of the Crookes tube into the air. He built a Crookes tube with a "window" at the end made of thin aluminium, facing the cathode so the cathode rays would strike it (later called a "Lenard tube"). He found that something came through, that would expose photographic plates and cause fluorescence. He measured the penetrating power of these rays through various materials. It has been suggested that at least some of these "Lenard rays" were actually X-rays.[8]
In 1889, Ivan Puluj, a lecturer in experimental physics at the Prague Polytechnic who since 1877 had been constructing various designs of gas-filled tubes to investigate their properties, published a paper on how sealed photographic plates became dark when exposed to the emanations from the tubes.[9]
Helmholtz formulated mathematical equations for X-rays. He postulated a dispersion theory before Röntgen made his discovery and announcement. He based it on the
In 1894, Nikola Tesla noticed damaged film in his lab that seemed to be associated with Crookes tube experiments and began investigating this invisible, radiant energy.[11][12] After Röntgen identified the X-ray, Tesla began making X-ray images of his own using high voltages and tubes of his own design,[13] as well as Crookes tubes.
Discovery by Röntgen

On
There are conflicting accounts of his discovery because Röntgen had his

Röntgen discovered their medical use when he made a picture of his wife's hand on a photographic plate formed due to X-rays. The photograph of his wife's hand was the first photograph of a human body part using X-rays. When she saw the picture, she said "I have seen my death."[24]
The discovery of X-rays generated significant interest. Röntgen's biographer Otto Glasser estimated that, in 1896 alone, as many as 49 essays and 1044 articles about the new rays were published.[25] This was probably a conservative estimate, if one considers that nearly every paper around the world extensively reported about the new discovery, with a magazine such as Science dedicating as many as 23 articles to it in that year alone.[26] Sensationalist reactions to the new discovery included publications linking the new kind of rays to occult and paranormal theories, such as telepathy.[27][28]
Advances in radiology

Röntgen immediately noticed X-rays could have medical applications. Along with his 28 December Physical-Medical Society submission, he sent a letter to physicians he knew around Europe (1 January 1896).[29] News (and the creation of "shadowgrams") spread rapidly with Scottish electrical engineer Alan Archibald Campbell-Swinton being the first after Röntgen to create an X-ray (of a hand). Through February, there were 46 experimenters taking up the technique in North America alone.[29]
The first use of X-rays under clinical conditions was by John Hall-Edwards in Birmingham, England on 11 January 1896, when he radiographed a needle stuck in the hand of an associate. On 14 February 1896, Hall-Edwards was also the first to use X-rays in a surgical operation.[30]
In early 1896, several weeks after Röntgen's discovery,
The first medical X-ray made in the United States was obtained using a discharge tube of Pului's design. In January 1896, on reading of Röntgen's discovery, Frank Austin of

Many experimenters, including Röntgen himself in his original experiments, came up with methods to view X-ray images "live" using some form of luminescent screen.
In 1901,
Hazards discovered
With the widespread experimentation with X‑rays after their discovery in
In August 1896, HD. Hawks, a graduate of Columbia College, suffered severe hand and chest burns from an X-ray demonstration. It was reported in Electrical Review and led to many other reports of problems associated with X-rays being sent in to the publication.[41] Many experimenters including Elihu Thomson at Edison's lab, William J. Morton, and Nikola Tesla also reported burns. Elihu Thomson deliberately exposed a finger to an X-ray tube over a period of time and suffered pain, swelling, and blistering.[42] Other effects were sometimes blamed for the damage including ultraviolet rays and (according to Tesla) ozone.[11] Many physicians claimed there were no effects from X-ray exposure at all.[42] On 3 August 1905, in San Francisco, California, Elizabeth Fleischman, an American X-ray pioneer, died from complications as a result of her work with X-rays.[43][44][45]
Hall-Edwards developed a cancer (then called X-ray dermatitis) sufficiently advanced by 1904 to cause him to write papers and give public addresses on the dangers of X-rays. His left arm had to be amputated at the elbow in 1908,
20th century and beyond
The many applications of X-rays immediately generated enormous interest. Workshops began making specialized versions of Crookes tubes for generating X-rays and these first-generation cold cathode or Crookes X-ray tubes were used until about 1920.
A typical early 20th-century medical X-ray system consisted of a Ruhmkorff coil connected to a cold cathode Crookes X-ray tube. A spark gap was typically connected to the high voltage side in parallel to the tube and used for diagnostic purposes.[48] The spark gap allowed detecting the polarity of the sparks, measuring voltage by the length of the sparks thus determining the "hardness" of the vacuum of the tube, and it provided a load in the event the X-ray tube was disconnected. To detect the hardness of the tube, the spark gap was initially opened to the widest setting. While the coil was operating, the operator reduced the gap until sparks began to appear. A tube in which the spark gap began to spark at around 6.4 centimeters (2.5 in) was considered soft (low vacuum) and suitable for thin body parts such as hands and arms. A 13-centimeter (5 in) spark indicated the tube was suitable for shoulders and knees. An 18-to-23-centimeter (7 to 9 in) spark would indicate a higher vacuum suitable for imaging the abdomen of larger individuals. Since the spark gap was connected in parallel to the tube, the spark gap had to be opened until the sparking ceased to operate the tube for imaging. Exposure time for photographic plates was around half a minute for a hand to a couple of minutes for a thorax. The plates may have a small addition of fluorescent salt to reduce exposure times.[48]
Crookes tubes were unreliable. They had to contain a small quantity of gas (invariably air) as a current will not flow in such a tube if they are fully evacuated. However, as time passed, the X-rays caused the glass to absorb the gas, causing the tube to generate "harder" X-rays until it soon stopped operating. Larger and more frequently used tubes were provided with devices for restoring the air, known as "softeners". These often took the form of a small side tube that contained a small piece of mica, a mineral that traps relatively large quantities of air within its structure. A small electrical heater heated the mica, causing it to release a small amount of air, thus restoring the tube's efficiency. However, the mica had a limited life, and the restoration process was difficult to control.
In
In about 1906, the physicist
In
In 1913, Henry Moseley performed crystallography experiments with X-rays emanating from various metals and formulated Moseley's law which relates the frequency of the X-rays to the atomic number of the metal.
The Coolidge X-ray tube was invented the same year by William D. Coolidge. It made possible the continuous emissions of X-rays. Modern X-ray tubes are based on this design, often employing the use of rotating targets which allow for significantly higher heat dissipation than static targets, further allowing higher quantity X-ray output for use in high-powered applications such as rotational CT scanners.

The use of X-rays for medical purposes (which developed into the field of
Medical science also used the motion picture to study human physiology. In 1913, a motion picture was made in Detroit showing a hard-boiled egg inside a human stomach. This early X-ray movie was recorded at a rate of one still image every four seconds.[51] Dr Lewis Gregory Cole of New York was a pioneer of the technique, which he called "serial radiography".[52][53] In 1918, X-rays were used in association with motion picture cameras to capture the human skeleton in motion.[54][55][56] In 1920, it was used to record the movements of tongue and teeth in the study of languages by the Institute of Phonetics in England.[57]
In 1914, Marie Curie developed radiological cars to support soldiers injured in World War I. The cars would allow for rapid X-ray imaging of wounded soldiers so battlefield surgeons could quickly and more accurately operate.[58]
From the early 1920s through to the 1950s, X-ray machines were developed to assist in the fitting of shoes[59] and were sold to commercial shoe stores.[60][61][62] Concerns regarding the impact of frequent or poorly controlled use were expressed in the 1950s,[63][64] leading to the practice's eventual end that decade.[65]
The X-ray microscope was developed during the 1950s.
The Chandra X-ray Observatory, launched on 23 July 1999, has been allowing the exploration of the very violent processes in the universe that produce X-rays. Unlike visible light, which gives a relatively stable view of the universe, the X-ray universe is unstable. It features stars being torn apart by black holes, galactic collisions, and novae, and neutron stars that build up layers of plasma that then explode into space.

An
Phase-contrast X-ray imaging refers to a variety of techniques that use phase information of an X-ray beam to form the image. Due to its good sensitivity to density differences, it is especially useful for imaging soft tissues. It has become an important method for visualizing cellular and histological structures in a wide range of biological and medical studies. There are several technologies being used for X-ray phase-contrast imaging, all using different principles to convert phase variations in the X-rays emerging from an object into intensity variations.[66][67] These include propagation-based phase contrast,[68] Talbot interferometry,[67] refraction-enhanced imaging,[69] and X-ray interferometry.[70] These methods provide higher contrast compared to normal absorption-based X-ray imaging, making it possible to distinguish from each other details that have almost similar density. A disadvantage is that these methods require more sophisticated equipment, such as synchrotron or microfocus X-ray sources, X-ray optics, and high resolution X-ray detectors.
Energy ranges

Soft and hard X-rays
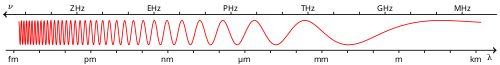
X-rays with high
Gamma rays
There is no consensus for a definition distinguishing between X-rays and
Occasionally, one term or the other is used in specific contexts due to historical precedent, based on measurement (detection) technique, or based on their intended use rather than their wavelength or source. Thus, gamma-rays generated for medical and industrial uses, for exampleProperties

X-ray
Hard X-rays can traverse relatively thick objects without being much
X-rays have much shorter wavelengths than visible light, which makes it possible to probe structures much smaller than can be seen using a normal
Interaction with matter
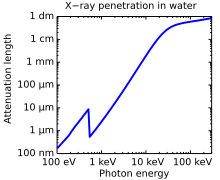
X-rays interact with matter in three main ways, through photoabsorption, Compton scattering, and Rayleigh scattering. The strength of these interactions depends on the energy of the X-rays and the elemental composition of the material, but not much on chemical properties, since the X-ray photon energy is much higher than chemical binding energies. Photoabsorption or photoelectric absorption is the dominant interaction mechanism in the soft X-ray regime and for the lower hard X-ray energies. At higher energies, Compton scattering dominates.
Photoelectric absorption
The probability of a photoelectric absorption per unit mass is approximately proportional to Z3/E3, where Z is the
A photoabsorbed photon transfers all its energy to the electron with which it interacts, thus ionizing the atom to which the electron was bound and producing a photoelectron that is likely to ionize more atoms in its path. An outer electron will fill the vacant electron position and produce either a characteristic X-ray or an
Compton scattering
Compton scattering is the predominant interaction between X-rays and soft tissue in medical imaging.
Rayleigh scattering
Rayleigh scattering is the dominant elastic scattering mechanism in the X-ray regime.[81] Inelastic forward scattering gives rise to the refractive index, which for X-rays is only slightly below 1.[82]
Production
Whenever charged particles (electrons or ions) of sufficient energy hit a material, X-rays are produced.
Production by electrons
| Anode material |
Atomic number |
Photon energy [keV] | Wavelength [nm] | ||
|---|---|---|---|---|---|
Kα1 |
Kβ1 | Kα1 | Kβ1 | ||
| W | 74 | 59.3 | 67.2 | 0.0209 | 0.0184 |
| Mo | 42 | 17.5 | 19.6 | 0.0709 | 0.0632 |
| Cu | 29 | 8.05 | 8.91 | 0.154 | 0.139 |
| Ag | 47 | 22.2 | 24.9 | 0.0559 | 0.0497 |
| Ga | 31 | 9.25 | 10.26 | 0.134 | 0.121 |
| In | 49 | 24.2 | 27.3 | 0.0512 | 0.0455 |
X-rays can be generated by an X-ray tube, a vacuum tube that uses a high voltage to accelerate the electrons released by a hot cathode to a high velocity. The high velocity electrons collide with a metal target, the anode, creating the X-rays.[85] In medical X-ray tubes the target is usually tungsten or a more crack-resistant alloy of rhenium (5%) and tungsten (95%), but sometimes molybdenum for more specialized applications, such as when softer X-rays are needed as in mammography. In crystallography, a copper target is most common, with cobalt often being used when fluorescence from iron content in the sample might otherwise present a problem.
The maximum energy of the produced X-ray photon is limited by the energy of the incident electron, which is equal to the voltage on the tube times the electron charge, so an 80 kV tube cannot create X-rays with an energy greater than 80 keV. When the electrons hit the target, X-rays are created by two different atomic processes:
- Characteristic X-ray emission (X-ray electroluminescence): If the electron has enough energy, it can knock an orbital electron out of the inner electron shell of the target atom. After that, electrons from higher energy levels fill the vacancies, and X-ray photons are emitted. This process produces an emission spectrum of X-rays at a few discrete frequencies, sometimes referred to as spectral lines. Usually, these are transitions from the upper shells to the K shell (called K lines), to the L shell (called L lines) and so on. If the transition is from 2p to 1s, it is called Kα, while if it is from 3p to 1s it is Kβ. The frequencies of these lines depend on the material of the target and are therefore called characteristic lines. The Kα line usually has greater intensity than the Kβ one and is more desirable in diffraction experiments. Thus the Kβ line is filtered out by a filter. The filter is usually made of a metal having one proton less than the anode material (e.g. Ni filter for Cu anode or Nb filter for Mo anode).
- continuous spectrum. The frequency of Bremsstrahlung is limited by the energy of incident electrons.
So, the resulting output of a tube consists of a continuous Bremsstrahlung spectrum falling off to zero at the tube voltage, plus several spikes at the characteristic lines. The voltages used in diagnostic X-ray tubes range from roughly 20 kV to 150 kV and thus the highest energies of the X-ray photons range from roughly 20 keV to 150 keV.[86]
Both of these X-ray production processes are inefficient, with only about one percent of the electrical energy used by the tube converted into X-rays, and thus most of the electric power consumed by the tube is released as waste heat. When producing a usable flux of X-rays, the X-ray tube must be designed to dissipate the excess heat.
A specialized source of X-rays which is becoming widely used in research is
Short nanosecond bursts of X-rays peaking at 15 keV in energy may be reliably produced by peeling pressure-sensitive adhesive tape from its backing in a moderate vacuum. This is likely to be the result of recombination of electrical charges produced by triboelectric charging. The intensity of X-ray triboluminescence is sufficient for it to be used as a source for X-ray imaging.[88]
Production by fast positive ions
X-rays can also be produced by fast protons or other positive ions. The proton-induced X-ray emission or particle-induced X-ray emission is widely used as an analytical procedure. For high energies, the production cross section is proportional to Z12Z2−4, where Z1 refers to the atomic number of the ion, Z2 refers to that of the target atom.[89] An overview of these cross sections is given in the same reference.
Production in lightning and laboratory discharges
X-rays are also produced in lightning accompanying terrestrial gamma-ray flashes. The underlying mechanism is the acceleration of electrons in lightning related electric fields and the subsequent production of photons through Bremsstrahlung.[90] This produces photons with energies of some few keV and several tens of MeV.[91] In laboratory discharges with a gap size of approximately 1 meter length and a peak voltage of 1 MV, X-rays with a characteristic energy of 160 keV are observed.[92] A possible explanation is the encounter of two streamers and the production of high-energy run-away electrons;[93] however, microscopic simulations have shown that the duration of electric field enhancement between two streamers is too short to produce a significant number of run-away electrons.[94] Recently, it has been proposed that air perturbations in the vicinity of streamers can facilitate the production of run-away electrons and hence of X-rays from discharges.[95][96]
Detectors
X-ray detectors vary in shape and function depending on their purpose. Imaging detectors such as those used for
Medical uses
This section needs additional citations for verification. (November 2017) |


Since Röntgen's discovery that X-rays can identify bone structures, X-rays have been used for medical imaging.[98] The first medical use was less than a month after his paper on the subject.[34] Up to 2010, five billion medical imaging examinations had been conducted worldwide.[99] Radiation exposure from medical imaging in 2006 made up about 50% of total ionizing radiation exposure in the United States.[100]
Projectional radiographs

Projectional radiography is the practice of producing two-dimensional images using X-ray radiation. Bones contain a high concentration of calcium, which, due to its relatively high atomic number, absorbs X-rays efficiently. This reduces the amount of X-rays reaching the detector in the shadow of the bones, making them clearly visible on the radiograph. The lungs and trapped gas also show up clearly because of lower absorption compared to tissue, while differences between tissue types are harder to see.[101]
Projectional radiographs are useful in the detection of
In medical diagnostic applications, the low energy (soft) X-rays are unwanted, since they are totally absorbed by the body, increasing the radiation dose without contributing to the image. Hence, a thin metal sheet, often of aluminium, called an X-ray filter, is usually placed over the window of the X-ray tube, absorbing the low energy part in the spectrum. This is called hardening the beam since it shifts the center of the spectrum towards higher energy (or harder) X-rays.
To generate an image of the
Computed tomography
Fluoroscopy
Radiotherapy
The use of X-rays as a treatment is known as
Adverse effects
X-rays are a form of
Experimental and epidemiological data currently do not support the proposition that there is a threshold dose of radiation below which there is no increased risk of cancer.[113] However, this is under increasing doubt.[114] Cancer risk can start at the exposure of 1100 mGy.[115] It is estimated that the additional radiation from diagnostic X-rays will increase the average person's cumulative risk of getting cancer by age 75 by 0.6–3.0%.[116] The amount of absorbed radiation depends upon the type of X-ray test and the body part involved.[112] CT and fluoroscopy entail higher doses of radiation than do plain X-rays.
To place the increased risk in perspective, a plain chest X-ray will expose a person to the same amount from background radiation that people are exposed to (depending upon location) every day over 10 days, while exposure from a dental X-ray is approximately equivalent to 1 day of environmental background radiation.[117] Each such X-ray would add less than 1 per 1,000,000 to the lifetime cancer risk. An abdominal or chest CT would be the equivalent to 2–3 years of background radiation to the whole body, or 4–5 years to the abdomen or chest, increasing the lifetime cancer risk between 1 per 1,000 to 1 per 10,000.[117] This is compared to the roughly 40% chance of a US citizen developing cancer during their lifetime.[118] For instance, the effective dose to the torso from a CT scan of the chest is about 5 mSv, and the absorbed dose is about 14 mGy.[119] A head CT scan (1.5 mSv, 64 mGy)[120] that is performed once with and once without contrast agent, would be equivalent to 40 years of background radiation to the head. Accurate estimation of effective doses due to CT is difficult with the estimation uncertainty range of about ±19% to ±32% for adult head scans depending upon the method used.[121]
The risk of radiation is greater to a fetus, so in pregnant patients, the benefits of the investigation (X-ray) should be balanced with the potential hazards to the fetus.[122][123] If there is 1 scan in 9 months, it can be harmful to the fetus.[124] Therefore, women who are pregnant get ultrasounds as their diagnostic imaging because this does not use radiation.[124] If there is too much radiation exposure there could be harmful effects on the fetus or the reproductive organs of the mother.[124] In the US, there are an estimated 62 million CT scans performed annually, including more than 4 million on children.[112] Avoiding unnecessary X-rays (especially CT scans) reduces radiation dose and any associated cancer risk.[125]
Medical X-rays are a significant source of human-made radiation exposure. In 1987, they accounted for 58% of exposure from human-made sources in the United States. Since human-made sources accounted for only 18% of the total radiation exposure, most of which came from natural sources (82%), medical X-rays only accounted for 10% of total American radiation exposure; medical procedures as a whole (including

Dosage due to dental X-rays varies significantly depending on the procedure and the technology (film or digital). Depending on the procedure and the technology, a single dental X-ray of a human results in an exposure of 0.5 to 4 mrem. A full mouth series of X-rays may result in an exposure of up to 6 (digital) to 18 (film) mrem, for a yearly average of up to 40 mrem.[127][128][129][130][131][132][133]
Financial incentives have been shown to have a significant impact on X-ray use with doctors who are paid a separate fee for each X-ray providing more X-rays.[134]
Early photon tomography or EPT[135] (as of 2015) along with other techniques[136] are being researched as potential alternatives to X-rays for imaging applications.
Other uses
Other notable uses of X-rays include:

- X-ray astronomy, which is an observational branch of astronomy, which deals with the study of X-ray emission from celestial objects.
- X-ray microscopic analysis, which uses electromagnetic radiation in the soft X-ray band to produce images of very small objects.
- X-ray fluorescence, a technique in which X-rays are generated within a specimen and detected. The outgoing energy of the X-ray can be used to identify the composition of the sample.
- Industrial radiography uses X-rays for inspection of industrial parts, particularly welds.
- pentimenti alterations in the course of painting or by later restorers, and sometimes previous paintings on the support. Many pigments such as lead whiteshow well in radiographs.
- X-ray spectromicroscopy has been used to analyse the reactions of pigments in paintings. For example, in analysing colour degradation in the paintings of van Gogh.[138]

- Authentication and quality control of packaged items.
- Industrial CT(computed tomography), a process that uses X-ray equipment to produce three-dimensional representations of components both externally and internally. This is accomplished through computer processing of projection images of the scanned object in many directions.
- Airport security luggage scanners use X-rays for inspecting the interior of luggage for security threats before loading on aircraft.
- Border control truck scanners and domestic police departments use X-rays for inspecting the interior of trucks.

- X-ray art and fine art photography, artistic use of X-rays, for example the works by Stane Jagodič
- X-ray hair removal, a method popular in the 1920s but now banned by the FDA.[140]
- Shoe-fitting fluoroscopes were popularized in the 1920s, banned in the US in the 1960s, in the UK in the 1970s, and later in continental Europe.
- Roentgen stereophotogrammetry is used to track movement of bones based on the implantation of markers
- X-ray photoelectron spectroscopy is a chemical analysis technique relying on the photoelectric effect, usually employed in surface science.
- H-bomb).
Visibility
While generally considered invisible to the human eye, in special circumstances X-rays can be visible. Brandes, in an experiment a short time after Röntgen's landmark 1895 paper, reported after dark adaptation and placing his eye close to an X-ray tube, seeing a faint "blue-gray" glow which seemed to originate within the eye itself.[141] Upon hearing this, Röntgen reviewed his record books and found he too had seen the effect. When placing an X-ray tube on the opposite side of a wooden door Röntgen had noted the same blue glow, seeming to emanate from the eye itself, but thought his observations to be spurious because he only saw the effect when he used one type of tube. Later he realized that the tube which had created the effect was the only one powerful enough to make the glow plainly visible and the experiment was thereafter readily repeatable. The knowledge that X-rays are actually faintly visible to the dark-adapted naked eye has largely been forgotten today; this is probably due to the desire not to repeat what would now be seen as a recklessly dangerous and potentially harmful experiment with ionizing radiation. It is not known what exact mechanism in the eye produces the visibility: it could be due to conventional detection (excitation of rhodopsin molecules in the retina), direct excitation of retinal nerve cells, or secondary detection via, for instance, X-ray induction of phosphorescence in the eyeball with conventional retinal detection of the secondarily produced visible light.
Though X-rays are otherwise invisible, it is possible to see the ionization of the air molecules if the intensity of the X-ray beam is high enough. The beamline from the wiggler at the European Synchrotron Radiation Facility[142] is one example of such high intensity.[143]
Units of measure and exposure
The measure of X-rays ionizing ability is called the exposure:
- The SI unit of ionizing radiationexposure, and it is the amount of radiation required to create one coulomb of charge of each polarity in one kilogram of matter.
- The electrostatic unitof charge of each polarity in one cubic centimeter of dry air. 1 roentgen = 2.58×10−4 C/kg.
However, the effect of ionizing radiation on matter (especially living tissue) is more closely related to the amount of energy deposited into them rather than the charge generated. This measure of energy absorbed is called the absorbed dose:
- The gray (Gy), which has units of (joules/kilogram), is the SI unit of absorbed dose, and it is the amount of radiation required to deposit one joule of energy in one kilogram of any kind of matter.
- The radis the (obsolete) corresponding traditional unit, equal to 10 millijoules of energy deposited per kilogram. 100 rad = 1 gray.
The equivalent dose is the measure of the biological effect of radiation on human tissue. For X-rays it is equal to the absorbed dose.
- The rad, or, in other words, 10 millijoules of energy deposited per kilogram. 100 rem = 1 Sv.
- The sievert (Sv) is the SI unit of equivalent dose, and also of effective dose. For X-rays the "equivalent dose" is numerically equal to a Gray (Gy). 1 Sv = 1 Gy. For the "effective dose" of X-rays, it is usually not equal to the Gray (Gy).
| Quantity | Unit | Symbol | Derivation | Year | SI equivalent |
|---|---|---|---|---|---|
| Activity (A) | becquerel | Bq | s−1 | 1974 | SI unit |
| curie | Ci | 3.7 × 1010 s−1 | 1953 | 3.7×1010 Bq | |
| rutherford | Rd | 106 s−1 | 1946 | 1,000,000 Bq | |
| Exposure (X) | coulomb per kilogram | C/kg | C⋅kg−1 of air | 1974 | SI unit |
| röntgen | R | esu / 0.001293 g of air | 1928 | 2.58 × 10−4 C/kg | |
| Absorbed dose (D) | gray | Gy | J⋅kg−1 | 1974 | SI unit |
| erg per gram | erg/g | erg⋅g−1 | 1950 | 1.0 × 10−4 Gy | |
rad
|
rad | 100 erg⋅g−1 | 1953 | 0.010 Gy | |
| Equivalent dose (H) | sievert | Sv | J⋅kg−1 × WR | 1977 | SI unit |
| röntgen equivalent man | rem | 100 erg⋅g−1 × WR | 1971 | 0.010 Sv | |
| Effective dose (E) | sievert | Sv | J⋅kg−1 × WR × WT | 1977 | SI unit |
| röntgen equivalent man | rem | 100 erg⋅g−1 × WR × WT | 1971 | 0.010 Sv |
See also
 Medical portal
Medical portal Physics portal
Physics portal- Backscatter X-ray
- Detective quantum efficiency
- High-energy X-rays
- Macintyre's X-Ray Film – 1896 documentary radiography film
- N ray
- Neutron radiation
- NuSTAR
- Radiographer
- Reflection (physics)
- Resonant inelastic X-ray scattering (RIXS)
- Small-angle X-ray scattering (SAXS)
- The X-Rays – 1897 British short silent comedy film
- X-ray absorption spectroscopy
- X-ray marker
- X-ray nanoprobe
- X-ray reflectivity
- X-ray vision
- X-ray welding
References
- ^ "X-Rays". Science Mission Directorate. NASA.
- ISBN 0-674-83339-2.
- ^ Caldwell, Wallace E.; Merrill, Edward H. (1964). History of the World. Vol. 1. United States: The Greystone Press. p. 394.
- .
- .
- .
- ^ Wyman T (Spring 2005). "Fernando Sanford and the Discovery of X-rays". "Imprint", from the Associates of the Stanford University Libraries: 5–15.
- ^ Thomson JJ (1903). The Discharge of Electricity through Gasses. US: Charles Scribner's Sons. pp. 182–186.
- PMID 9212769. Archived from the originalon 28 May 2008. Retrieved 6 April 2008.
- ^ Wiedmann's Annalen, Vol. XLVIII.
- ^ PMID 18635636.
- ISBN 978-1-61820-149-2.
- ^ Tesla's technical publications indicate that he invented and developed a single-electrode X-ray tube. Morton, William James and Hammer, Edwin W. (1896) American Technical Book Co., p. 68. U.S. patent 514,170, "Incandescent Electric Light". U.S. patent 454,622 "System of Electric Lighting". These differed from other X-ray tubes in having no target electrode and worked with the output of a Tesla coil.
- doi:10.1038/053274b0. see also pp. 268 and 276 of the same issue.
- S2CID 44719943.
Rats have been trained to respond to signals consisting of very low doses of chi-ray directed to the head.
- PMID 8475784.
- PMID 8044245.
- ^ Karlsson EB (9 February 2000). "The Nobel Prizes in Physics 1901–2000". Stockholm: The Nobel Foundation. Retrieved 24 November 2011.
- ^ Peters P (1995). "W. C. Roentgen and the discovery of x-rays". Textbook of Radiology. Medcyclopedia.com, GE Healthcare. Archived from the original on 11 May 2008. Retrieved 5 May 2008.
- ISBN 978-0930405229.
- ^ Arthur C (8 November 2010). "Google doodle celebrates 115 years of X-rays". The Guardian. Guardian US. Retrieved 5 February 2019.
- ISBN 978-0-8135-2358-3.
- ^ Sample S (27 March 2007). "X-Rays". The Electromagnetic Spectrum. NASA. Retrieved 3 December 2007.
- ^ Markel H (20 December 2012). "'I Have Seen My Death': How the World Discovered the X-Ray". PBS NewsHour. PBS. Retrieved 23 March 2019.
- ^ Glasser O (1958). Dr. W. C. Ro ̈ntgen. Springfield: Thomas.
- S2CID 142518799.
- hdl:2318/1770480.
- S2CID 35604474.
- ^ PMID 2685937.
- ^ "Major John Hall-Edwards". Birmingham City Council. Archived from the original on 28 September 2012. Retrieved 17 May 2012.
- ISBN 9781600212802.
- ^ "Green, James (Zoological Artist), Sciagraphs of British batrachians and reptiles, 1897". Yale Centre for British Art. Retrieved 24 November 2021.
- S2CID 4054184.
- ^ PMID 7998549.
- ISBN 3631581203
- ^ "Visible Proofs: Forensic Views of the Body: Galleries: Cases: Could X-rays Have Saved President William McKinley?". NLM.NIH.gov. Retrieved 24 January 2022.
- PMID 17779817.
- ISBN 978-1589809468.
- ^ Ce4Rt (March 2014). Understanding Ionizing Radiation and Protection. p. 174.
{{cite book}}: CS1 maint: numeric names: authors list (link) - ISBN 978-0930405229.
- PMID 21239576.
- ^ a b "ISU Health Physics Radinf – First 50 Years". Sites.Google.com. Retrieved 24 January 2022.
- ^ California, San Francisco Area Funeral Home Records, 1835–1979. Database with images. FamilySearch. Jacob Fleischman in the entry for Elizabeth Aschheim. 3 August 1905. Citing funeral home J.S. Godeau, San Francisco, San Francisco, California. Record book Vol. 06, p. 1–400, 1904–1906. San Francisco Public Library. San Francisco History and Archive Center.
- ^ Editor. (5 August 1905). Aschheim. Obituaries. San Francisco Examiner. San Francisco, California.
- ^ Editor. (5 August 1905). Obituary Notice. Elizabeth Fleischmann. San Francisco Chronicle. Page 10.
- ^ "Major John Hall-Edwards". Birmingham City Council. Archived from the original on 28 September 2012. Retrieved 23 April 2010.
- ^ "JOHN HALL-EDWARDS". Engole the Elven for Knowledge. 15 June 2018. Retrieved 27 October 2023.
- ^ a b Schall K (1905). Electro-medical Instruments and their Management. Bemrose & Sons Ltd. Printers. pp. 96, 107.
- . Retrieved 25 March 2022.
- ^ Birmingham City Council: Major John Hall-Edwards Archived 28 September 2012 at the Wayback Machine
- ^ "X-ray movies show hard boiled egg fighting digestive organs (1913)". The News-Palladium. 4 April 1913. p. 2. Retrieved 26 November 2020.
- ^ "X-ray moving pictures latest (1913)". Chicago Tribune. 22 June 1913. p. 32. Retrieved 26 November 2020.
- ^ "Homeopaths to show movies of body's organs at work (1915)". The Central New Jersey Home News. 10 May 1915. p. 6. Retrieved 26 November 2020.
- ^ "How X-Ray Movies Are Taken (1918)". Davis County Clipper. 15 March 1918. p. 2. Retrieved 26 November 2020.
- ^ "X-ray movies (1919)". Tampa Bay Times. 12 January 1919. p. 16. Retrieved 26 November 2020.
- ^ "X-ray movies perfected. Will show motions of bones and joints of human body. (1918)". The Sun. 7 January 1918. p. 7. Retrieved 26 November 2020.
- ^ "Talk is cheap? X-ray used by Institute of Phonetics (1920)". New Castle Herald. 2 January 1920. p. 13. Retrieved 26 November 2020.
- ^ Jorgensen TJ (10 October 2017). "Marie Curie and her X-ray vehicles' contribution to World War I battlefield medicine". The Conversation. Retrieved 23 February 2018.
- ^ "X-Rays for Fitting Boots". Warwick Daily News (Qld.: 1919–1954). 25 August 1921. p. 4. Retrieved 27 November 2020.
- ^ "T. C. BEIRNE'S X-RAY SHOE FITTING". Telegraph (Brisbane, Qld. : 1872–1947). 17 July 1925. p. 8. Retrieved 5 November 2017.
- ^ "THE PEDOSCOPE". Sunday Times (Perth, WA : 1902–1954). 15 July 1928. p. 5. Retrieved 5 November 2017.
- ^ "X-RAY SHOE FITTINGS". Biz (Fairfield, NSW : 1928–1972). 27 July 1955. p. 10. Retrieved 5 November 2017.
- ^ "SHOE X-RAY DANGERS". Brisbane Telegraph (Qld. : 1948–1954). 28 February 1951. p. 7. Retrieved 5 November 2017.
- ^ "X-ray shoe sets in S.A. 'controlled'". News (Adelaide, SA : 1923–1954). 27 April 1951. p. 12. Retrieved 5 November 2017.
- ^ "Ban On Shoe X-ray Machines Resented". Canberra Times (ACT : 1926–1995). 26 June 1957. p. 4. Retrieved 5 November 2017.
- S2CID 121322301.
- ^ .
- S2CID 4273199.
- S2CID 4287341.
- S2CID 23523144.
- ISBN 978-0-521-65214-8. Archived from the originalon 11 November 2012. Retrieved 4 November 2012.
- ^ "Physics.nist.gov". Physics.nist.gov. Retrieved 8 November 2011.
- ^ ISBN 978-0-7503-0591-4.
- ISBN 978-0-201-02116-5.
- ISBN 978-0-12-436603-9.
- ISBN 978-3-540-25312-9.
- ^ Hodgman, Charles, ed. (1961). CRC Handbook of Chemistry and Physics, 44th Ed. US: Chemical Rubber Co. p. 2850.
- ^ Government of Canada, Canadian Centre for Occupational Health and Safety (9 May 2019). "Radiation – Quantities and Units of Ionizing Radiation: OSH Answers". CCOHS.ca. Retrieved 9 May 2019.
- ISBN 978-0-683-30118-2.
- ISBN 978-0-683-30118-2.
- doi:10.1016/S0969-806X(00)00290-5. Archived from the originalon 12 December 2011. Retrieved 8 November 2012.
- ISBN 978-0-521-65214-8. Archived from the originalon 11 November 2012. Retrieved 4 November 2012.
- ^ "X-ray Transition Energies Database". NIST Physical Measurement Laboratory. 9 December 2011. Retrieved 19 February 2016.
- ^ "X-Ray Data Booklet Table 1-3" (PDF). Center for X-ray Optics and Advanced Light Source, Lawrence Berkeley National Laboratory. 1 October 2009. Archived from the original (PDF) on 23 April 2009. Retrieved 19 February 2016.
- ISBN 978-0-443-07027-3.
- ISBN 978-0-683-30118-2.
- ISBN 90-5199-248-3.
- S2CID 4372536. Retrieved 2 February 2013.
- .
- S2CID 10679475.
- .
- S2CID 43609721.
- .
- PMID 28503005.
- .
- PMID 30034044.
- PMID 31030653.
- PMID 17629432.
- ^ PMID 20933639.
Of the 5 billion imaging investigations performed worldwide...
- ^ a b "Medical Radiation Exposure Of The U.S. Population Greatly Increased Since The Early 1980s". ScienceDaily. Retrieved 24 January 2022.
- ISSN 0033-8419.
- ^ Van Haver A, Kolk S, DeBoodt S, Valkering K, Verdonk P (2018). "Accuracy of total knee implant position assessment based on postoperative X-rays, registered to pre-operative CT-based 3D models". Orthopaedic Proceedings. 99-B (Supp 4).
- ISBN 978-1-85233-617-2.
- ^ PMID 34662062, retrieved 20 April 2024
- ^ ISSN 1084-208X.
- S2CID 18082594.
- S2CID 7672187.
- ^ "11th Report on Carcinogens". Ntp.niehs.nih.gov. Archived from the original on 9 December 2010. Retrieved 8 November 2010.
- PMID 18440940.
- S2CID 17264651.
- PMID 17963274.
- ^ S2CID 2760372.
- S2CID 13301920.
- S2CID 4419048. Archived from the original(PDF) on 12 September 2011.
- PMID 31217755.
- S2CID 8516754.
- ^ a b "Radiation Dose in X-Ray and CT Exams". RadiologyInfo.org. Radiological Society of North America (RSNA) and American College of Radiology (ACR). Retrieved 24 January 2022.
- ^ "National Cancer Institute: Surveillance Epidemiology and End Results (SEER) data". Seer.cancer.gov. 30 June 2010. Retrieved 8 November 2011.
- .
- ^ Shrimpton, P.C; Miller, H.C; Lewis, M.A; Dunn, M. Doses from Computed Tomography (CT) examinations in the UK – 2003 Review Archived 22 September 2011 at the Wayback Machine
- PMID 18777910.
- PMID 13358242.
- ^ "Pregnant Women and Radiation Exposure". eMedicine Live online medical consultation. Medscape. 28 December 2008. Archived from the original on 23 January 2009. Retrieved 16 January 2009.
- ^ PMID 19047611.
- PMID 15671393.
- ISBN 978-0-309-09156-5., data credited to NCRP (US National Committee on Radiation Protection) 1987
- ^ "ANS / Public Information / Resources / Radiation Dose Calculator". Archived from the original on 16 May 2012. Retrieved 16 May 2012.
- ^ "HOW DANGEROUS IS RADIATION?". PhyAst.Pitt.edu. Retrieved 24 January 2022.
- ^ Muller, Richard. Physics for Future Presidents, Princeton University Press, 2010
- ^ X-Rays Archived 15 March 2007 at the Wayback Machine. Doctorspiller.com (9 May 2007). Retrieved on 2011-05-05.
- ^ X-Ray Safety Archived 4 April 2007 at the Wayback Machine. Dentalgentlecare.com (6 February 2008). Retrieved on 2011-05-05.
- ^ "Dental X-Rays". Idaho State University. Archived from the original on 7 November 2012. Retrieved 7 November 2012.
- ^ D.O.E. – About Radiation Archived 27 April 2012 at the Wayback Machine
- PMID 29408150.
- ^ "Using lasers instead of x-rays". Open University. 24 February 2011. Retrieved 28 July 2021.
- ^ Dent S (12 February 2015). "Scientists achieve X-ray vision with safe, visible light". Engadget. Retrieved 28 July 2021.
- ISBN 978-3-540-25317-4.
- PMID 21314202.
- ^ Ahi K, Anwar M (May 2016). "Advanced terahertz techniques for quality control and counterfeit detection". In Anwar MF, Crowe TW, Manzur T (eds.). Terahertz Physics, Devices, and Systems X: Advanced Applications in Industry and Defense. Vol. 9856. Society of Photographic Instrumentation Engineers. pp. 31–44.
- ISBN 978-1401815554.
- ^ Frame P. "Wilhelm Röntgen and the Invisible Light". Tales from the Atomic Age. Oak Ridge Associated Universities. Retrieved 11 October 2021.
- ^ European Synchrotron Radiation Facility ID11
- ISBN 978-0-471-49858-2.
External links
- "On a New Kind of Rays". Nature. 53 (1369): 274–276. January 1896. doi:10.1038/053274b0.
- "Ion X-Ray tubes". The Cathode Ray Tube site.
- "Index of Early Bremsstrahlung Articles". Shade Tree Physics. 12 April 2010.
- Samuel JJ (20 October 2013). "La découverte des rayons X par Röntgen". Bibnum Education (in French). Röntgen's discovery of X-rays (PDF; English translation)
- Oakley, P. A., Navid Ehsani, N., & Harrison, D. E. (2020). 5 Reasons Why Scoliosis X-Rays Are Not Harmful. Dose-Response. https://doi.org/10.1177/1559325820957797
- "X-ray Crystallography". A web for learning how X-rays can "see" inside the crystals.