Rickettsia parkeri
| Rickettsia parkeri | |
|---|---|
| |
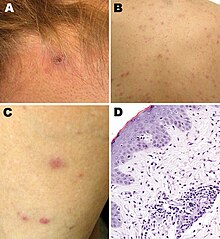
| Rickettsia parkeri rickettsiosis skin lesions: A - papulovesicular rash on back and leg; D - micrograph of biopsy specimen
| |
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Pseudomonadota |
| Class: | Alphaproteobacteria |
| Order: | Rickettsiales |
| Family: | Rickettsiaceae |
| Genus: | Rickettsia |
| Species group: | Spotted fever group
|
| Species: | R. parkeri
|
| Binomial name | |
| Rickettsia parkeri Lackman et al., 1965
| |
Rickettsia parkeri (abbreviated R. parkeri) is a
Biology
R. parkeri is classified in the spotted fever group of the genus Rickettsia.[1][2] Genetically, its close relatives include R. africae, R. sibirica, R. conorii, R. rickettsii, R. peacockii, and R. honei.[1]
The organism has been isolated from numerous species of ticks in the genus Amblyomma: A. americanum in the United States; A. aureolatum in Brazil; A. maculatum in Mexico, Peru, and the United States; A. nodosum in Brazil; A. ovale in Brazil and Mexico; A. parvitarsum in Argentina and Chile; A. tigrinum in Argentina, Bolivia, Brazil, and Uruguay; and A. triste in Argentina, Brazil, the United States, and Uruguay.[2][3][4][5] Different ticks may carry different strains of the organism. R. parkeri sensu stricto ("in the strict sense") is found in A. maculatum and A. triste; R. parkeri strain NOD, in A. nodosum; R. parkeri strain Parvitarsum, in A. parvitarsum; and R. parkeri strain Atlantic rainforest, in A. aureolatum and A. ovale.[2]
Human infections
The first report of a confirmed human case of infection with R. parkeri was published in 2004.
Epidemiology
Of all human cases documented in the medical literature, 87% were 18-64 years of age, and most cases were male.[8] Brazil, Argentina, and the United States accounted for the majority of cases in the medical literature.[8] In the United States, most of the 40 cases reported to the Centers for Disease Control and Prevention (CDC) as of 2016 became infected between the months of July and September.[13]: 5–6
Diagnosis
The CDC recommends polymerase chain reaction (PCR) of a biopsy or swab of an eschar, or PCR of a biopsy of a rash, for diagnosis of R. parkeri infection.[13]: 27 In addition, indirect immunofluorescence antibody (IFA) assays using paired acute and convalescent sera can be used.[13]: 27
Clinical manifestations
A 2008 study compared 12 R. parkeri cases with 208 Rocky Mountain spotted fever cases caused by R. rickettsii.[7] Although both R. parkeri and R. rickettsii caused fever, rash, myalgia, and headache, R. parkeri caused eschars and R. rickettsii did not.[7] Furthermore, the percentage of patients hospitalized was lower for R. parkeri than for R. rickettsii (33% vs 78%), and R. parkeri led to no deaths while R. rickettsii led to death in 7% of cases.[7]
A 2021 systematic review of 32 confirmed and 45 probable cases of human infection with R. parkeri determined that 94% of the confirmed cases had fever, 91% an eschar, 72% a rash, 56% headache, and 56% myalgia, with similar percentages among the probable cases.[8] The rash was most frequently described as papular or macular.[8] Among the confirmed and probable cases, the most common treatment was doxycycline, followed by tetracycline.[8] Although 9% of all the cases were hospitalized, there was a "100% rate of clinical recovery."[8]
History
In 1939, Ralph R. Parker, director of the
References
- ^ PMID 16901827.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - ^ PMID 29439989.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - PMID 19788817.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - PMID 30882330.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - PMID 31742525.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - ^ PMID 14999622.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - ^ PMID 18808353.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - ^ S2CID 234596034.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - S2CID 246701684.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - PMID 15799527.
- PMID 32748891.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - ^ PMID 21529406.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - ^ PMID 27172113.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - ^ PMID 18808353.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - PMID 14318051.)
{{cite journal}}: CS1 maint: multiple names: authors list (link
External links
- "Rickettsia parkeri rickettsiosis". Centers for Disease Control and Prevention. January 10, 2019.
