Posterior vitreous detachment
This article needs additional citations for verification. (July 2010) |
| Posterior vitreous detachment | |
|---|---|
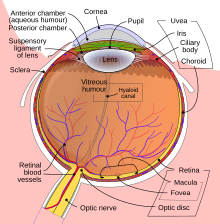 | |
| Schematic diagram of the human eye. | |
| Specialty | Ophthalmology |
A posterior vitreous detachment (PVD) is a condition of the eye in which the vitreous membrane separates from the retina.[1] It refers to the separation of the posterior hyaloid membrane from the retina anywhere posterior to the vitreous base (a 3–4 mm wide attachment to the ora serrata).
The condition is common for older adults; over 75% of those over the age of 65 develop it. Although less common among people in their 40s or 50s, the condition is not rare for those individuals. Some research has found that the condition is more common among women.[2][3]
Symptoms

When this occurs there is a characteristic pattern of symptoms:
- Flashes of light (photopsia)
- A sudden dramatic increase in the number of floaters
- A ring of floaters or hairs just to the temporal side of the central vision
As a posterior vitreous detachment proceeds, adherent vitreous membrane may pull on the retina. While there are no pain fibers in the retina, vitreous traction may stimulate the retina, with resultant flashes that can look like a perfect circle.[citation needed]
If a retinal vessel is torn, the leakage of blood into the vitreous cavity is often perceived as a "shower" of floaters. Retinal vessels may tear in association with a retinal tear, or occasionally without the retina being torn.[citation needed]
A Weiss ring can sometimes be seen with ophthalmoscopy as very strong indicator that vitreous detachment has occurred. This ring can remain free-floating for years after detachment. [citation needed]
Complications
The risk of retinal detachment is the greatest in the first 6 weeks following a vitreous detachment, but can occur over 3 months after the event.
The risk of retinal tears and detachment associated with vitreous detachment is higher in patients with myopic retinal degeneration,
Causes
The
Age and refractive error play a role in determining the onset of PVD in a healthy person. PVD is rare in
People with
PVD may also occur in cases of cataract surgery, within weeks or months of the surgery.[5]
The vitreous membrane is more firmly attached to the retina
Diagnosis
Posterior Vitreous Detachment is diagnosed via dilated eye examination. For some patients the vitreous gel is extremely clear and so it can be hard to see the PVD. In these cases, additional imaging such as Optical Coherence Tomography (OCT) or ocular ultrasound are used.[6]
Treatment
Therapy is not required or indicated in posterior vitreous detachment, unless there are associated
See also
- Vitreous membrane
- Central serous retinopathy
- Epiretinal membrane
- Vitrectomy
- Floater
References
- ^ Gauger E; Chin EK; Sohn EH (17 November 2014). "Vitreous Syneresis: An Impending Posterior Vitreous Detachment (PVD)". University of Iowa Health Care: Ophthalmology and Visual Sciences; See "Discussion" following "Clinical Course".
{{cite web}}: CS1 maint: postscript (link) - PMID 10163464.
- ^ "Posterior vitreous detachment". rnib.org.uk. 2023-02-28. Retrieved 3 November 2015.
- ^ Acta Ophthalmol. 2012 May;90(3):e179-84. doi: 10.1111/j.1755-3768.2011.02310.x. Epub 2011 Nov 22.Prevalence of early and late stages of physiologic PVD in emmetropic elderly population. Schwab C, Ivastinovic D, Borkenstein A, Lackner EM, Wedrich A, Velikay-Parel M.
- PMID 18776863.
- ^ Thompson, John. "Posterior Vitreous Detachment". American Society of Retinal Specialists. ASRS. Retrieved July 11, 2017.
- ^ a b "Posterior Vitreous Detachment". Cleveland Clinic. Retrieved 2008-12-24.
- PMID 8090453.
