Aldosterone
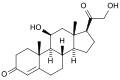
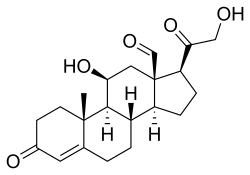 Skeletal formula of the fictitious aldehyde form[1]
| |
 | |
| Names | |
|---|---|
| IUPAC name
11β,21-Dihydroxy-3,20-dioxopregn-4-en-18-al
| |
| Systematic IUPAC name
(1S,3aS,3bS,9aR,9bS,10S,11aR)-10-Hydroxy-1-(hydroxyacetyl)-9a-methyl-7-oxo-1,2,3,3a,3b,4,5,7,8,9,9a,9b,10,11-tetradecahydro-11aH-cyclopenta[a]phenanthrene-11a-carbaldehyde | |
| Other names
Aldocorten; Aldocortin; Electrocortin; Reichstein X; 18-Aldocorticosterone; 18-Oxocorticosterone
| |
| Identifiers | |
3D model (
JSmol ) |
|
| ChEBI | |
| ChEMBL | |
| ChemSpider | |
| DrugBank | |
ECHA InfoCard
|
100.000.128 |
IUPHAR/BPS |
|
| KEGG | |
| MeSH | Aldosterone |
PubChem CID
|
|
| UNII | |
CompTox Dashboard (EPA)
|
|
| |
| |
| Properties | |
| C21H28O5 | |
| Molar mass | 360.450 g·mol−1 |
| Pharmacology | |
| H02AA01 (WHO) | |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa).
| |
Aldosterone is the main mineralocorticoid
Aldosterone is part of the
Another example is spironolactone, a potassium-sparing diuretic of the steroidal spirolactone group, which interferes with the aldosterone receptor (among others) leading to lower blood pressure by the mechanism described above.
Aldosterone was first isolated by Sylvia Tait (Simpson) and Jim Tait in 1953; in collaboration with Tadeusz Reichstein.[10][11][12]
Biosynthesis
This section needs additional citations for verification. (December 2023) |
The
Aldosterone and
Aldosterone synthase is normally absent in other sections of the adrenal gland.[14]
Stimulation
Aldosterone synthesis is stimulated by several factors:
- increase in the plasma concentration of angiotensin III, a metabolite of angiotensin II
- increase in angiotensin I, which is in turn regulated by renin, a hormone secreted in the kidneys.
- Serum potassium concentrations are the most potent stimulator of aldosterone secretion.
- the ACTH stimulation test, which is sometimes used to stimulate the production of aldosterone along with cortisol to determine whether primary or secondary adrenal insufficiency is present. However, ACTH has only a minor role in regulating aldosterone production; with hypopituitarism there is no atrophy of the zona glomerulosa.
- plasma acidosis
- the stretch receptors located in the atriaof the heart. If decreased blood pressure is detected, the adrenal gland is stimulated by these stretch receptors to release aldosterone, which increases sodium reabsorption from the urine, sweat, and the gut. This causes increased osmolarity in the extracellular fluid, which will eventually return blood pressure toward normal.
- adrenoglomerulotropin, a lipid factor, obtained from pineal extracts. It selectively stimulates secretion of aldosterone.[15]
The secretion of aldosterone has a diurnal rhythm.[16]
Biological function
Aldosterone is the primary of several endogenous members of the class of mineralocorticoids in humans. Deoxycorticosterone is another important member of this class. Aldosterone tends to promote Na+ and water retention, and lower plasma K+ concentration by the following mechanisms:
- Acting on the nuclear Na+/K+ pumps, which pumps three sodium ions out of the cell, into the interstitial fluid and two potassium ions into the cell from the interstitial fluid. This creates a concentration gradient which results in reabsorption of sodium (Na+) ions and water (which follows sodium) into the blood, and secreting potassium (K+) ions into the urine (lumen of collecting duct).
- Aldosterone upregulates epithelial sodium channels (ENaCs) in the collecting ductand the colon, increasing apical membrane permeability for Na+ and thus absorption.
- Cl− is reabsorbed in conjunction with sodium cations to maintain the system's electrochemical balance.
- Aldosterone stimulates the secretion of K+ into the tubular lumen.[17]
- Aldosterone stimulates Na+ and water reabsorption from the gut, salivary and sweat glands in exchange for K+.
- Aldosterone stimulates secretion of H+ via the H+/ATPase in the intercalated cellsof the cortical collecting tubules
- Aldosterone upregulates expression of NCC in the distal convoluted tubule chronically and its activity acutely.[18]
Aldosterone is responsible for the reabsorption of about 2% of filtered sodium in the kidneys, which is nearly equal to the entire sodium content in human blood under normal glomerular filtration rates.[19]
Aldosterone, probably acting through mineralocorticoid receptors, may positively influence neurogenesis in the dentate gyrus.[20]
Mineralocorticoid receptors
The MR is stimulated by both aldosterone and cortisol, but a mechanism protects the body from excess aldosterone receptor stimulation by glucocorticoids (such as cortisol), which happen to be present at much higher concentrations than mineralocorticoids in the healthy individual. The mechanism consists of an enzyme called
Control of aldosterone release from the adrenal cortex

Major regulators
The role of the renin–angiotensin system
Angiotensin is involved in regulating aldosterone and is the core regulation.[22] Angiotensin II acts synergistically with potassium, and the potassium feedback is virtually inoperative when no angiotensin II is present.[23] A small portion of the regulation resulting from angiotensin II must take place indirectly from decreased blood flow through the liver due to constriction of capillaries.[24] When the blood flow decreases so does the destruction of aldosterone by liver enzymes.
Although sustained production of aldosterone requires persistent
The plasma concentration of potassium
The amount of plasma renin secreted is an indirect function of the serum potassium[27][28] as probably determined by sensors in the carotid artery.[29][30]
Adrenocorticotropic hormone
Adrenocorticotropic hormone (ACTH), a pituitary peptide, also has some stimulating effect on aldosterone, probably by stimulating the formation of deoxycorticosterone, a precursor of aldosterone.[31] Aldosterone is increased by blood loss,[32] pregnancy,[33] and possibly by further circumstances such as physical exertion, endotoxin shock, and burns.[34][35]
Miscellaneous regulators
The role of sympathetic nerves
The aldosterone production is also affected to one extent or another by nervous control, which integrates the inverse of carotid artery pressure,[29] pain, posture,[33] and probably emotion (anxiety, fear, and hostility)[36] (including surgical stress).[37] Anxiety increases aldosterone,[36] which must have evolved because of the time delay involved in migration of aldosterone into the cell nucleus.[38] Thus, there is an advantage to an animal's anticipating a future need from interaction with a predator, since too high a serum content of potassium has very adverse effects on nervous transmission.
The role of baroreceptors
Pressure-sensitive baroreceptors are found in the vessel walls of nearly all large arteries in the thorax and neck, but are particularly plentiful in the sinuses of the carotid arteries and in the arch of the aorta. These specialized receptors are sensitive to changes in mean arterial pressure. An increase in sensed pressure results in an increased rate of firing by the baroreceptors and a negative feedback response, lowering systemic arterial pressure. Aldosterone release causes sodium and water retention, which causes increased blood volume, and a subsequent increase in blood pressure, which is sensed by the baroreceptors.[39] To maintain normal homeostasis these receptors also detect low blood pressure or low blood volume, causing aldosterone to be released. This results in sodium retention in the kidney, leading to water retention and increased blood volume.[40]
The plasma concentration of sodium
Aldosterone levels vary as an inverse function of sodium intake as sensed via osmotic pressure.[41] The slope of the response of aldosterone to serum potassium is almost independent of sodium intake.[42] Aldosterone is increased at low sodium intakes, but the rate of increase of plasma aldosterone as potassium rises in the serum is not much lower at high sodium intakes than it is at low. Thus, potassium is strongly regulated at all sodium intakes by aldosterone when the supply of potassium is adequate, which it usually is in "primitive" diets.
Aldosterone feedback
Feedback by aldosterone concentration itself is of a nonmorphological character (that is, other than changes in the cells' number or structure) and is poor, so the electrolyte feedbacks predominate, short term.[34]
Associated clinical conditions
Hyperaldosteronism is abnormally increased levels of aldosterone, while hypoaldosteronism is abnormally decreased levels of aldosterone.
A measurement of aldosterone in blood may be termed a plasma aldosterone concentration (PAC), which may be compared to plasma renin activity (PRA) as an aldosterone-to-renin ratio.
Hyperaldosteronism
Depending on cause and other factors, hyperaldosteronism can be treated by surgery and/or medically, such as by
The ratio of renin to aldosterone is an effective screening test to screen for primary hyperaldosteronism related to
Hypoaldosteronism
An ACTH stimulation test for aldosterone can help in determining the cause of hypoaldosteronism, with a low aldosterone response indicating a primary hypoaldosteronism of the adrenals, while a large response indicating a secondary hypoaldosteronism. The most common cause of this condition (and related symptoms) is Addison's disease; it is typically treated by fludrocortisone, which has a much longer persistence (1 day) in the bloodstream.
Additional images
-
Corticosteroid biosynthetic pathway in rat
References
- PMID 35479823.
- ^ "CSD Entry: ALDAHA10". Cambridge Structural Database: Access Structures. Cambridge Crystallographic Data Centre. 1972. Retrieved 2022-09-03.
- PMID 5040851.
- PMID 26668301.
- OCLC 777127809.
- ^ PMID 25905305.
- ^ a b Marieb Human Anatomy & Physiology 9th edition, chapter:16, page:629, question number:14
- PMID 26217336.
- ^ "Pharmacokinetics of Corticosteroids". 2003. Retrieved 15 June 2016.
- PMID 16002531.
- S2CID 5738857.
- PMID 12788829.
- ISSN 2002-4436.
- OCLC 1076268769.)
{{cite book}}: CS1 maint: location missing publisher (link - PMID 13821632.
- PMID 14660513.
- PMID 10760062.
- PMID 23739593.
- OCLC 43702042.
- S2CID 24099239.
- ISBN 1-4160-2328-3.
- PMID 4342886.
- PMID 6286729.
- PMID 844145.
- ^ PMID 22546854.
- S2CID 23622821.
- PMID 513492.
- PMID 222934.
- ^ a b Gann DS Mills IH Bartter 1960 On the hemodynamic parameter mediating increase in aldosterone secretion in the dog. Fed. Proceedings 19; 605–610.
- PMID 13896654.
- PMID 4336939.
- ^ Ruch TC Fulton JF 1960 Medical Physiology and Biophysics. W.B. Saunders and Co., Phijl & London. On p1099.
- ^ PMID 13590935.
- ^ OCLC 186705.
- PMID 13375573. on 529
- ^ PMID 13449153.
- PMID 14934025.
- ^ Sharp GUG Leaf A 1966 in; Recent Progress in Hormone Research. (Pincus G, ed.
- ^ Copstead, E. C. & Banasik, J. L. (2010.) Pathophysiology. (4th ed.). St. Louis, Mo: Saunders Elsevier.
- ^ Marieb, E. N. (2004) Human anatomy and physiology (6th ed) San Francisco: Pearson Benjamin Cummings.
- PMID 3971930.
- PMID 5054456.
- PMID 13299331.
- PMID 10957926.
- PMID 23199617.
- ^ a b Hoffman R (October 19, 2018). "What is the role of aldosterone-to-renin ratio (ARR) in the diagnosis of hyperaldosteronism?". www.medscape.com. Retrieved 18 May 2019.