Anaplasma phagocytophilum
| Anaplasma phagocytophilum | |
|---|---|
| |
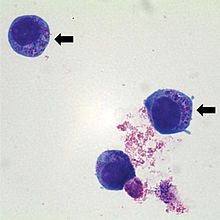
| Human Wright-Giemsa stain
| |
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Pseudomonadota |
| Class: | Alphaproteobacteria |
| Order: | Rickettsiales |
| Family: | Ehrlichiaceae |
| Genus: | Anaplasma |
| Species: | A. phagocytophilum
|
| Binomial name | |
| Anaplasma phagocytophilum (Foggie 1949) Dumler et al. 2001[1]
| |
| Synonyms | |
|
Rickettsia phagocytophila ovis | |
Anaplasma phagocytophilum (formerly Ehrlichia phagocytophilum)
A. phagocytophilum is a
Biology
A. phagocytophilum is a small, obligate, intracellular bacterium with a Gram-negative cell wall. It is 0.2–1.0 μm and lacks a lipopolysaccharide biosynthetic machinery. The bacterium first resides in an early endosome, where it acquires nutrients for binary fission and grows into small groups called morulae. This bacterium prefers to grow within myeloid or granulocytic cells.[4]
Hosts
Hosts include goat, cattle, horse and dog. Cattle infections had been suspected but were only first confirmed by Nieder et al. 2012.[5]
Role in human disease
A. phagocytophilum causes human granulocytic
Clinical signs in animals
The disease is multisystemic, but the most severe changes are
Bacterial mechanism
A. phagocytophilum binds to fucosylated and sialylated scaffold proteins on neutrophil and granulocyte surfaces. A
This bacterium has the ability to affect neutrophils by altering their function. It can survive the first encounter with the host cell by detoxifying superoxide produced by neutrophil phagocyte oxidase assembly. It also disrupts normal neutrophil function, such as endothelial cell adhesion, transmigration, motility, degranulation, respiratory burst, and phagocytosis.[4] It causes an increase in the secretion of IL-8, a chemoattractant that increases the phagocytosis of neutrophils. The purpose of this is to increase bacterial dissemination into the neutrophil.[6]
Laboratory diagnosis
These tests can be performed to determine an A. phagocytophilum infection:
- Indirect immunofluorescence assay is the principal test used to detect infection. The acute and convalescent phase serum samples can be evaluated to look for a four-fold change in antibody titer to A. phagocytophilum.
- Intracellular Inclusions (morulae) are visualized in granulocytes on Wright- or Giemsa- stained blood smears.
- Polymerase chain reaction assays are used to detect A. phagocytophilum DNA.[7]
Antibiotic therapy
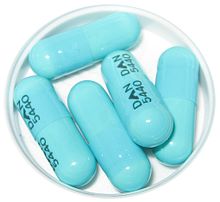
Patients with HGA undergo doxycycline therapy, 100 mg twice daily until the patient's fever subsides for at least 3 days. This drug has been the most beneficial to those patients infected with the bacteria. Some other tetracycline drugs are also effective. In general, patients with symptoms of HGA and unexplained fever after a tick exposure should receive empiric doxycycline therapy while their diagnostic tests are pending, especially if they experience leukopenia and/or thrombocytopenia.[7]
In animals, antibiotics such as
References
- ^ Page Anaplasma on lpsn.dsmz.de
- PMID 11760958.
- ^ a b c Tick-Borne Fever reviewed and published by WikiVet, accessed 12 October 2011.
- ^ PMID 16485466.
- PMID 26734888.
- S2CID 20043230.
- ^ a b "Human Anaplasmosis Information for Health Professionals: Diagnostic tests". Diseases. Minnesota Department of Health. Archived from the original on 2019-02-13. Retrieved 2011-04-27.
External links
- Anaplasma phagocytophilum HZ Genome Page
- Anaplasma+phagocytophilum at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- Zhang L, Liu Y, Ni D, et al. (November 2008). "Nosocomial transmission of human granulocytic anaplasmosis in China". JAMA. 300 (19): 2263–70. PMID 19017912.
