Chloroprocaine
 | |
| Clinical data | |
|---|---|
| Trade names | Nesacaine, Iheezo, others |
| AHFS/Drugs.com | Micromedex Detailed Consumer Information |
| ATC code | |
| Legal status | |
| Legal status | |
| Identifiers | |
| |
JSmol) | |
| |
| |
| | |
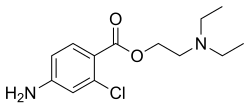
Chloroprocaine (trade name Nesacaine, Nesacaine-MPF) (often in the hydrochloride salt form as the aforementioned trade names) is a local anesthetic given by injection during surgical procedures and labor and delivery. Chloroprocaine vasodilates; this is in contrast to cocaine which vasoconstricts. Chloroprocaine is an ester anesthetic.[3]
Medical uses
Chloroprocaine is used for
It is also indicated for
It is also used for
Chloroprocaine is also indicated for ocular surface anesthesia.[2]
Subarachnoid block
Chloroprocaine was developed to meet the need for a short-acting spinal anaesthetic that is reliable and has a favourable safety profile to support the growing need for day-case surgery. Licensed in Europe for surgical procedures up to 40 minutes, chloroprocaine is an ester-type local anaesthetic with the shortest duration of action of all the established local anaesthetics. It has a significantly shorter duration of action than lidocaine and is significantly less toxic. Chloroprocaine has a motor block lasting for 40 minutes, a rapid onset time of 3–5 minutes (9.6 min ± 7.3 min at 40 mg dose; 7.9 min ± 6.0 min at 50 mg dose) and a time to ambulation of 90 minutes without complications, especially lacking transient neurologic symptomatology.
These data are based upon a retrospective review of 672 patients suitable for spinal anaesthesia in surgical procedures less than 60 minutes' duration using 30–40 mg chloroprocaine. The results showed good surgical anaesthesia, a fast onset time, and postoperative mobilization after 90 minutes without complications.[6]
The use of chloroprocaine in the
In recent years, several studies have been published on the safe use of intrathecal chloroprocaine when appropriate dosage is used and with preservative-free preparations.[16][10]
It is currently approved for intrathecal use in the United States [17] and in Europe.[18]
Obstetrics
Amide-linked local anesthetic agents, such as
The in vitro half-life of chloroprocaine is 21 seconds for maternal and 43 seconds for fetal blood. In patients who are homozygous atypical for plasma cholinesterase, chloroprocaine typically exists for two minutes in circulation.[20][21]
Synthesis

The hydrochloride salt of 4-amino-2-chlorobenzoyl chloride is made by the reaction of 2-chloro-4-aminobenzoic acid with thionyl chloride.
References
- ^ "Nesacaine- chloroprocaine hydrochloride injection, solution Nesacaine MPF- chloroprocaine hydrochloride injection, solution". DailyMed. 1 September 2022. Retrieved 21 January 2023.
- ^ a b "Iheezo- chloroprocaine hydrochloride ophthalmic gel gel". DailyMed. 27 September 2022. Retrieved 21 January 2023.
- ^ "Chloroprocaine". Drug Bank. Archived from the original on 2018-09-20. Retrieved 2009-10-21.
- ^ Sintetica Limited (9 March 2017). "Ampres 10 mg/ml solution for injection". EMC. Archived from the original on 19 August 2019. Retrieved 2 December 2018.
- ^ a b c Physicians' Desk Reference. "chloroprocaine hydrochloride". USA: PDR.net. Archived from the original on 2019-08-19. Retrieved 2018-12-02.
- ^ Palas T (2009). "Ampres (chloroprocaine) Summary of Product Characteristics". Perimed. 3 (2): 31–34.
Cloroprocaina in chirurgia ambulatoriale: uno studio osservazionale
- PMID 15673892.
- PMID 7189987.
- S2CID 205430566.
- ^ S2CID 42930157.
- S2CID 31870857.
- doi:10.1136/rapm-00115550-198409030-00004 (inactive 31 January 2024).)
{{cite journal}}: CS1 maint: DOI inactive as of January 2024 (link - PMID 1443708.
- S2CID 9604835.
- PMID 2346671.
- S2CID 525005.
- ^ "Clorotekal: Chloroprocaine Hydrochloride". Drugs@FDA: FDA-Approved Drugs. Archived from the original on 2020-10-19. Retrieved 2018-05-29.
- ^ "Rediscovered Local Holds Promise for Spinal Anesthesia". Anesthesiology News. McMahon Publishing. 5 June 2013. Archived from the original on 29 September 2022. Retrieved 20 September 2013.
- PMID 3970100.
- ISBN 978-0-323-02357-3.
- ISBN 978-0-683-30665-1.
- ISBN 978-0-444-52166-8.
External links
- "Chloroprocaine". Drug Information Portal. U.S. National Library of Medicine.
- "Chloroprocaine hydrochloride". Drug Information Portal. U.S. National Library of Medicine.
