Ductal carcinoma in situ
This article needs to be updated. The reason given is: almost every source in this article is around fifteen years old. (June 2022) |
| Breast cancer in situ | |
|---|---|
| Other names | Intraductal carcinoma |
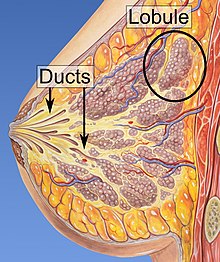 | |
| Ducts of the mammary gland, the location of ductal carcinoma | |
| Specialty | Oncology |

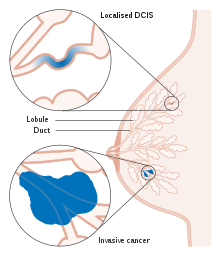
Ductal carcinoma in situ (DCIS), also known as intraductal carcinoma, is a pre-cancerous or non-invasive cancerous lesion of the
In DCIS, abnormal cells are found in the lining of one or more
DCIS has been classified according to the architectural pattern of the cells (solid, cribriform, papillary, and micropapillary),
About 20–30% of those who do not receive treatment develop breast cancer.[10][11] DCIS is the most common type of pre-cancer in women. There is some disagreement on its status as cancer; some bodies include DCIS when calculating breast cancer statistics, while others do not.[12][13]
Terminology
Ductal carcinoma in situ (DCIS) literally means groups of "cancerous"
For statistical purposes, DCIS is sometimes counted as a "cancer", but this is not always the case.[13][17] When classified as a cancer, it is referred to as a "non-invasive" or "pre-invasive" form.[14][18] It is described by the National Cancer Institute as a "noninvasive condition".[13]
Signs and symptoms

Most of the women who develop DCIS do not experience any symptoms. The majority of cases (80-85%) are detected through screening mammography. The first signs and symptoms may appear if the cancer advances. Because of the lack of early symptoms, DCIS is most often detected at
In a few cases, DCIS may cause:
- A lump or thickening in or near the breast or under the arm
- A change in the size or shape of the breast
- Nipple discharge or nipple tenderness; the nipple may also be inverted, or pulled back into the breast
- Ridges or pitting of the breast; the skin may look like the skin of an orange
- A change in the way the skin of the breast, swelling, redness or scaliness.[20]
Causes
The specific causes of DCIS are still unknown. The risk factors for developing this condition are similar to those for invasive breast cancer.[21]
Some women are however more prone than others to developing DCIS. Women considered at higher risks are those who have a
Long-term use of estrogen-progestin hormone replacement therapy (HRT) for more than five years after menopause, genetic mutations (BRCA1 or BRCA2 genes), atypical
Diagnosis
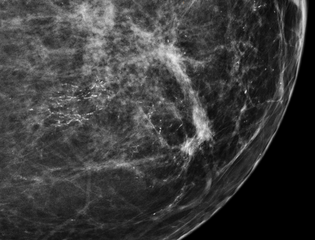
80% of cases in the United States are detected by mammography screening.[23] More definitive diagnosis is made by breast biopsy for histopathology.
-
Mammogrammicrocalcifications in ductal carcinoma in situ
-
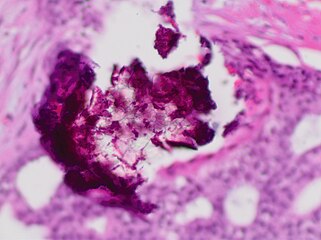
Histopathology of dystrophicmicrocalcificationsin DCIS, H&E stain.
-
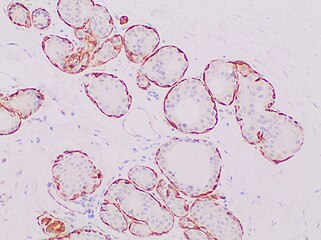
Histopathologic architectural patterns of DCIS.[24]
-
DCIS with microinvasion, defined as focus of invasive cancer measuring up to 1.0 mm in size.[26]
-
invasive ductal carcinoma.
-
Ductal carcinoma in situ with comedo necrosis spanning 30% of its diameter, which is generally regarded as the minimal size to classify it as comedo.[27]
Treatment
There are different opinions on the best treatment of DCIS.
While surgery reduces the risk of subsequent cancer, many people never develop cancer even without treatment and the associated side effects.[30] There is no evidence comparing surgery with watchful waiting and some feel watchful waiting may be a reasonable option in certain cases.[30]
Radiation therapy
Use of
Mastectomy
There is no evidence that mastectomy decreases the risk of death over a lumpectomy.[37] Mastectomy, however, may decrease the rate of the DCIS or invasive cancer occurring in the same location.[7][37]
Mastectomies remain a common recommendation in those with persistent microscopic involvement of margins after local excision or with a diagnosis of DCIS and evidence of suspicious, diffuse microcalcifications.[38]
Sentinel node biopsy
Some institutions that have encountered high rates of recurrent invasive cancers after mastectomy for DCIS have endorsed routine
Prognosis
With treatment, the prognosis is excellent, with greater than 97% long-term survival. If untreated, DCIS progresses to invasive cancer in roughly one-third of cases, usually in the same breast and quadrant as the earlier DCIS.[43] About 2% of women who are diagnosed with this condition and treated died within 10 years.[44] Biomarkers can identify which women who were initially diagnosed with DCIS are at high or low risk of subsequent invasive cancer.[45][46]
Epidemiology

DCIS is often detected with mammographies but can rarely be felt. With the increasing use of screening mammography, noninvasive cancers are more frequently diagnosed and now constitute 15% to 20% of all breast cancers.[38]
Cases of DCIS have increased five-fold between 1983 and 2003 in the United States due to the introduction of screening mammography.[44] In 2009 about 62,000 cases were diagnosed.[44]
References
- PMID 24415964.
- ISBN 978-0-387-98348-6.
- ^ DePolo, Jamie (13 October 2023). "Breast Cancer Stages: Stage 0 breast cancer". Breastcancer.org.
- PMID 18270336.
- ISBN 978-0-387-21997-4.
- PMID 31880271.
- ^ PMID 32461218.
- ^ PMID 20629475.
- PMID 34537861.
- ISBN 978-0-7817-9516-6.
- PMID 20956824.
- ^ "Breast Cancer Treatment (PDQ®)". NCI. 11 April 2014. Retrieved 19 June 2014.
- ^ a b c d e "Breast Cancer Treatment (PDQ®)". NCI. January 1980. Retrieved 19 June 2014.
- ^ PMID 20956817.
- ISBN 978-1-4419-6505-9.
- ISBN 9780470757796.
- ISBN 978-0-387-31056-5.
- ISBN 978-0-387-75246-4.
- ^ "Breast Cancer". Retrieved 28 June 2010.
- ^ "Signs and Symptoms". Retrieved 28 June 2010.
- ^ "After the mammogram". Archived from the original on 7 April 2010. Retrieved 28 June 2010.
- ^ "Intraductal Carcinoma of the Breast". Archived from the original on 11 June 2010. Retrieved 28 June 2010.
- ^ "Ductal Carcinoma In Situ". cancer.gov. 9 January 2015. Retrieved 5 March 2015.
- PMID 34734332.
- "This article is licensed under a Creative Commons Attribution 4.0 International License" - PMID 33363702.
- PMID 35464581.(PDF). College of American Pathologists.
- "This is an open access article distributed under the terms of the Creative Commons Attribution License CC BY 4.0."
Source for microinvasion: "Protocol for the Examination of Resection Specimens from Patients with Ductal Carcinoma In Situ (DCIS) of the Breast, Version: 4.4.0.0. Protocol Posting Date: June 2021" - PMID 30980039.
- PMID 26697227.
- ^ "Ductal Carcinoma In Situ: Treatment Options for Patients With DCIS". National Cancer Institute at NIH. National Institutes of Health. 11 July 2014.
- ^ PMID 24600734.
- PMID 21145284.
- Johns Hopkins Medicine
- ^ PMID 24259251.
- PMID 20071685.
- PMID 20956824.
- ^ "NIH DCIS Consensus Conference Statement". National Institutes of Health. September 2009. Archived from the original on 13 August 2011. Retrieved 19 June 2014.
- ^ PMID 20629475.
They found women undergoing mastectomy were less likely than women undergoing lumpectomy plus radiation to experience local DCIS or invasive recurrence. Women undergoing BCS alone were also more likely to experience a local recurrence than women treated with mastectomy. We found no study showing a mortality reduction associated with mastectomy over breast conserving surgery with or without radiation
- ^ a b "Intraductal carcinoma". Archived from the original on 10 April 2016. Retrieved 28 June 2010.
- S2CID 1924867.
- PMID 32337481.
- PMID 31388937.
- PMID 17300928.
- ISBN 978-0-323-35317-5.
- ^ PMID 20956818.
- PMID 20427430.
- PMID 19502809.

![Histopathologic architectural patterns of DCIS.[24]](http://upload.wikimedia.org/wikipedia/commons/thumb/5/58/Histopathologic_architectural_patterns_of_DCIS.png/288px-Histopathologic_architectural_patterns_of_DCIS.png)
![Histopathology of high-grade DCIS. H&E stain. RBC = red blood cell.[25]](http://upload.wikimedia.org/wikipedia/commons/thumb/3/3f/Histopathology_of_high-grade_DCIS.png/202px-Histopathology_of_high-grade_DCIS.png)
![DCIS with microinvasion, defined as focus of invasive cancer measuring up to 1.0 mm in size.[26]](http://upload.wikimedia.org/wikipedia/commons/thumb/d/d9/Histopathology_of_microinvasive_ductal_carcinoma_in_situ.png/289px-Histopathology_of_microinvasive_ductal_carcinoma_in_situ.png)
![Ductal carcinoma in situ with comedo necrosis spanning 30% of its diameter, which is generally regarded as the minimal size to classify it as comedo.[27]](http://upload.wikimedia.org/wikipedia/commons/thumb/4/41/Histopathology_of_ductal_carcinoma_in_situ_with_comedo_necrosis.jpg/321px-Histopathology_of_ductal_carcinoma_in_situ_with_comedo_necrosis.jpg)