Histopathology
This article needs additional citations for verification. (June 2021) |

Histopathology (compound of three
Collection of tissues
Histopathological examination of tissues starts with
Preparation for histology
The tissue is then prepared for viewing under a microscope using either chemical fixation or frozen section.
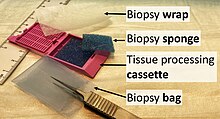
If a large sample is provided e.g. from a surgical procedure then a pathologist looks at the tissue sample and selects the part most likely to yield a useful and accurate diagnosis - this part is removed for examination in a process commonly known as grossing or cut up. Larger samples are cut to correctly situate their anatomical structures in the cassette. Certain specimens (especially biopsies) can undergo agar pre-embedding to assure correct tissue orientation in cassette & then in the block & then on the diagnostic microscopy slide. This is then placed into a plastic cassette for most of the rest of the process.[citation needed]
Chemical fixation
In addition to formalin, other chemical fixatives have been used. But, with the advent of immunohistochemistry (IHC) staining and diagnostic molecular pathology testing on these specimen samples, formalin has become the standard chemical fixative in human diagnostic histopathology. Fixation times for very small specimens are shorter, and standards exist in human diagnostic histopathology.
Processing
Water is removed from the sample in successive stages by the use of increasing concentrations of alcohol.[1] Xylene is used in the last dehydration phase instead of alcohol - this is because the wax used in the next stage is soluble in xylene where it is not in alcohol allowing wax to permeate (infiltrate) the specimen.[1] This process is generally automated and done overnight. The wax infiltrated specimen is then transferred to an individual specimen embedding (usually metal) container. Finally, molten wax is introduced around the specimen in the container and cooled to solidification so as to embed it in the wax block.[1] This process is needed to provide a properly oriented sample sturdy enough for obtaining a thin microtome section(s) for the slide.
Once the wax embedded block is finished, sections will be cut from it and usually placed to float on a waterbath surface which spreads the section out. This is usually done by hand and is a skilled job (histotechnologist) with the lab personnel making choices about which parts of the specimen microtome wax ribbon to place on slides. A number of slides will usually be prepared from different levels throughout the block. After this the thin section mounted slide is stained and a protective cover slip is mounted on it. For common stains, an automatic process is normally used; but rarely used stains are often done by hand.[1]
Frozen section processing

An initial evaluation of a suspected lymphoma is to make a "touch prep" wherein a glass slide is lightly pressed against excised lymphoid tissue, and subsequently stained (usually
Staining of processed histology slides
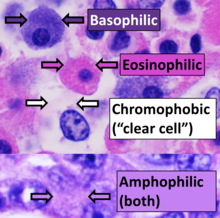
This can be done to slides processed by the chemical fixation or frozen section slides. To see the tissue under a microscope, the sections are stained with one or more
The most commonly used stain in histology is a combination of
Recently, antibodies have been used to stain particular proteins, lipids and carbohydrates. Called immunohistochemistry, this technique has greatly increased the ability to specifically identify categories of cells under a microscope. Other advanced techniques include in situ hybridization to identify specific DNA or RNA molecules. These antibody staining methods often require the use of frozen section histology. These procedures above are also carried out in the laboratory under scrutiny and precision by a trained specialist medical laboratory scientist (a histoscientist). Digital cameras are increasingly used to capture histopathological images.
Interpretation
The histological slides are examined under a microscope by a
Following are examples of general features of suspicious findings that can be appreciated from low to high magnification on histopathology:
-
Orientation (lowest magnification): In this case oriented by the skin surface (green). A lesion is seen (red) and its demarcation can be discerned (diffuse in this case)
-
Architectural pattern of any suspicious cells, in this case nests of cells, as well as components of the intervening stroma.
-
Cellular arrangement, including crowding andmitosescan also be appreciated at this level.
-
Subcellular features (may need highest magnification)
Architectural patterns
Major histopathologic architectural patterns include:
-
Nests: islands of cells of similar type.
-
Trabecular, elongated (rod-shaped) groups of cells.
-
Papillary: Protuberances of epithelioid cells around fibrovascular cores.
-
Micropapillary: Papillary tufts without fibrovascular cores
-
Fascicular: Generally the same cell type throughout, but some form band-like groups that are aligned in the same direction.
-
Woven or storiform: Elongated cells or nuclei wherein small bundles are aligned in an otherwise haphazard pattern.
-
Solid: More or less the same cell type throughout, with no spaces between, and no other particular pattern.
-
Cribriform: Solid with multiple clear spaces.
-
Whorled: Multiple concentric objects, or spiral-shaped
-
Cartwheel pattern: Center points that radiate cells or connective tissue outward
Nuclear patterns
Major nuclear patterns include:
-
Monomorphic when having relatively similar sizes and shapes.
-
nucleus to cytoplasm ratio. These features generally indicate malignancy.
-
Fine chromatin when inconspicuous (essentially only nucleoli seen in the nuclei), versus coarse chromatin.
-
Sometimes "euchromatic" nuclei are used for visual appearance, but this strictly refers to the molecular structure of DNA.
In myocardial infarction
After a
See also
- Anatomical pathology
- Molecular pathology
- Frozen section procedure
- Medical technologist
- Laser capture microdissection
- List of pathologists
References
- ^ a b c d "Basic guide to histological staining and tissue preparation". Archived from the original on July 6, 2016.
- ^ "Perl - Red Blood Cell - Staining". Scribd.
- ISBN 978-1-4160-2973-1. 8th edition.
External links
- Virtual Histology Course - University of Zurich (German, English version in preparation)
- Histopathology of the uterine cervix - digital atlas (IARC Screening Group)
- Histopathology Virtual Slidebox - University of Iowa




















