Haemodynamic response

In
Vascular anatomy overview
In order to understand how blood is delivered to cranial tissues, it is important to understand the vascular anatomy of the space itself. Large cerebral arteries in the brain split into smaller
Mechanisms
Various cell types play a role in HR, including astrocytes, smooth muscle cells, endothelial cells of blood vessels, and pericytes. These cells control whether the vessels are constricted or dilated, which dictates the amount of oxygen and glucose that is able to reach the neuronal tissue.

Astrocytes
Astrocytes are unique in that they are intermediaries that lie between blood vessels and neurons. They are able to communicate with other astrocytes via
Constriction has been shown in vitro to occur when NE is placed in the synapse and is taken up by astrocyte receptors. NE uptake leads to an increase in intracellular astrocyte
Smooth muscle
Dilation occurs when
Pericytes
A principal function of pericytes is to interact with astrocytes, smooth muscle cells, and other intracranial cells to form the blood brain barrier and to modulate the size of blood vessels to ensure proper delivery and distribution of oxygen and nutrients to neuronal tissues. Pericytes have both cholinergic (α2) and adrenergic (β2) receptors. Stimulation of the latter leads to vessel relaxation, while stimulation of the cholinergic receptors leads to contraction.
Paracrine activity and oxygen availability have been shown to also modulate pericyte activity. The peptides
Complications
The haemodynamic response is rapid delivery of blood to active neuronal tissue. Complications in this response arise in acute coronary syndromes and
Acute coronary syndrome
Acute infections, such as
These effects result from
Pulmonary arterial hypertension
Pulmonary hypertension (PAH) is disease of small pulmonary arteries that is usually caused by more than one mechanism. This includes
Overall, pulmonary arterial tension and acute coronary syndromes are few of the many diseases that lead to hypoxia of neuronal tissue, which in turns deteriorates the haemodynamic response and leads to neuronal death. Prolonged hypoxia induces neuronal death via apoptosis. With a dysfunctional haemodynamic response, active neuronal tissue due to membrane depolarization lacks the necessary energy to propagate signals, as a result of blood flow hindrance. This affects many functions in the body, and may lead to severe symptoms.
Reduced haemodynamic response diseases
Alzheimer's disease
In this disease, there is a build of the amyloid beta protein in the brain. This ultimately leads to a reduction in the haemodynamic response and less blood flow in the brain. This reduced cerebral blood flow not only kills neuronal cells because of shortages in oxygen and glucose but it also reduces the brain's ability to remove amyloid beta. In a healthy brain, these protein fragments are broken down and eliminated. In Alzheimer's disease, the fragments accumulate to form hard, insoluble plaques which reduce blood flow. Two proteins are involved in this accumulation of amyloid beta: serum response factor or SRF and myocardin.[9] Together, these 2 proteins determine whether smooth muscle of blood vessels contract. SRF and myocardin are more active in the brains of people with Alzheimer's disease. When these proteins are active, they turn on SREBP2 which inhibits LRP-1. LRP-1 helps the brain remove amyloid beta. Therefore, when SRF and myocardin are active, there is a buildup in amyloid beta protein which ultimately leads to less blood flow in the brain because of contracted blood vessels.[10]
Ischemia
A decrease in circulation in the brain vasculature due to stroke or injury can lead to a condition known as ischemia. In general, decrease in blood flow to the brain can be a result of thrombosis causing a partial or full blockage of blood vessels, hypotension in systemic circulation (and consequently the brain), or cardiac arrest. This decrease in blood flow in the cerebral vascular system can result in a buildup of metabolic wastes generated by neurons and glial cells and a decrease in oxygen and glucose delivery to them. As a result, cellular energy failure, depolarization of neuronal and glial membranes, edema, and excess neurotransmitter and calcium ion release can occur.[11] This ultimately ends with cell death, as cells succumb to a lack of nutrients to power their metabolism and to a toxic brain environment, full of free radicals and excess ions that damage normal cell organelle function.
Clinical use
Changes in brain activity are closely coupled with changes in blood flow in those areas, and knowing this has proved useful in mapping brain functions in humans. The measurement of haemodynamic response, in a clinical setting, can be used to create images of the brain in which especially active and inactive regions are shown as distinct from one another. This can be a useful tool in diagnosing neural disease or in pre-surgical planning.
Functional magnetic resonance imaging
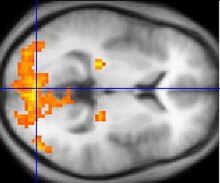
If fMRI can be used to detect the regular flow of blood in a healthy brain, it can also be used to detect the problems with a brain that has undergone degenerative diseases. Functional MRI, using haemodynamic response, can help assess the effects of stroke and other degenerative diseases such as Alzheimer's disease on brain function. Another way fMRI could be used is in the planning of surgery of the brain. Surgeons can use fMRI to detect blood flow of the most active areas of the brain and the areas involved in critical functions like thought, speech, movement, etc. In this way, brain procedures are less dangerous because there is a brain mapping that shows which areas are vital to a person's life. Haemodynamic response is vital to fMRI and clinical use because through the study of blood flow we are able to examine the anatomy of the brain and effectively plan out procedures of the brain and link together the causes of degenerative brain disease.[15]
Resting state fMRI enables the evaluation of the interaction of brain regions, when not performing a specific task.[16] This is also used to show the default mode network.
PET scan
PET scan or
Before a PET scan begins, the patient will be injected with a small dose of a radioactive medicine tagged to a
References
- PMID 28957666.
- S2CID 36555564.
- PMID 22927793.
- ^ PMID 16357084.
- S2CID 7117482.
- PMID 16212810.
- ^ PMID 23046969.
- PMID 15459304.
- ^ "Blood Flow In Alzheimer's Disease." ScienceDaily. ScienceDaily, 29 June 2009. Web. 04 Nov. 2012. https://www.sciencedaily.com/releases/2009/06/090624211135.htm
- ^ "Doc Blog." Cardiovascular System Proteins Play a Role in Alzheimer's. N.p., n.d. Web. 04 Nov. 2012. http://www.docblog.org/cardiovascular-system-proteins-play-a-role-in-alzheimers.html
- ^ Arcinlegas, David B., MD. "Hypoxic-Ischemic Brain Injury | Internationalbrain.org."Hypoxic-Ischemic Brain Injury | Internationalbrain.org. International Brain Injury Association, Mar. 2010. Web. <http://www.internationalbrain.org/?q=node/131>
- S2CID 8736954.
- ^ Barbe, Kurt, and Guy Nagels. "Extracting the Haemodynamic Response From Functional MRI Data." IEEE Xplore. http://ieeexplore.ieee.org/stamp/stamp.jsp?arnumber=06210369, n.d. Web. 03 Nov. 2012. <http://ieeexplore.ieee.org/stamp/stamp.jsp?arnumber=06210369>
- ^ Buckner, Randy L. "Event Related FMRI and the Haemodynamic Response." Human Brain Mapping. Wiley-Liss Inc., 1998. Web. 10 Oct. 2012
- ^ Attwell, David. "The Neural Basis of Functional Brain Imaging Signals." University College London, n.d. Web. <http://dx.dio.org/10.1016/s0166-2236(02)02264-6>
- S2CID 93823.
- ^ "Learn More About Brain Imaging Technologies." Learn More About Brain Imaging Technologies. N.p., n.d. Web. 03 Nov. 2012. <http://learn.genetics.utah.edu/content/addiction/drugs/brainimage.html Archived 2013-01-21 at the Wayback Machine>
- ^ Shibasaki, Hiroshi. "Human Brain Mapping: Hemodynamic Response and Electrophysiology." Elsevier. N.p., n.d. Web. <http://moodle.technion.ac.il/pluginfile.php/195507/mod_resource/content/0/week1/FunctionalBrainImaging.pdf>
