Nissen fundoplication
| Nissen fundoplication | |
|---|---|
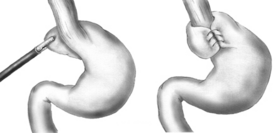 Diagram of a Nissen fundoplication. | |
| Other names | Laparoscopic Nissen fundoplication |
| ICD-9-CM | 44.66, 44.67 |
A Nissen fundoplication, or laparoscopic Nissen fundoplication when performed via
History
Dr. Rudolph Nissen (1896–1981) first performed the procedure in 1955 and published the results of two cases in a 1956 Swiss Medical Weekly.[2] In 1961 he published a more detailed overview of the procedure.[3] Nissen originally called the surgery "gastroplication". The procedure has borne his name since it gained popularity in the 1970s.[4]
Indications
The most common indication for a fundoplication is GERD that has failed lifestyle modification and medical management.
Technique

In a fundoplication, the
In a Nissen fundoplication, also called a complete fundoplication, the fundus is wrapped the entire 360 degrees around the esophagus. In contrast, surgery for achalasia is generally accompanied by either a Dor or Toupet partial fundoplication, which is less likely than a Nissen wrap to aggravate the dysphagia that characterizes achalasia. In a Dor (anterior) fundoplication, the fundus is laid over the top of the esophagus; while in a Toupet (posterior) fundoplication, the fundus is wrapped around the back of the esophagus.[citation needed]
The procedure can be performed with open surgery but is now routinely performed
This procedure can also be completed robotically. Outcomes comparing laparoscopic fundoplication to robotic fundoplication show similar clinical outcomes, but robotic fundoplication is more likely to have an increased length of operative time and financial cost.[11]
Mechanism of relief
Whenever the stomach contracts, it also closes off the esophagus instead of squeezing stomach acids into it. This prevents the reflux of gastric acid (in GERD). Although antacids and PPI drug therapy can reduce the effects of reflux acid, successful surgical treatment has the advantage of eliminating drug side-effects and damaging effects from other components of reflux such as bile or gastric contents.[1] The Nissen fundoplication reduces reflux by reinforcing the LES by increasing LES pressure and increasing the LES length.[6]
Effectiveness
Nissen (complete) fundoplication is generally considered to be safe and effective, with a mortality rate of less than 1% and many of the most common post-operative complications minimized or eliminated by the partial fundoplication procedures now more commonly used. Studies have shown that after 10 years, 89.5% of patients are still symptom-free. When compared to stand alone medical therapy with PPIs, Nissen fundoplication has been found to be superior in reducing acid reflux as well as the symptoms associated with reflux.[12] Fundoplication was found to be better at increasing LES pressure than PPI therapy, whilst having similar risk for adverse events.[13] In patients with non-acid reflux, a hiatal hernia, or respiratory symptoms, surgical intervention was found to be more effective at controlling symptoms than PPIs alone.[7]
Complications
Complications include "gas bloat syndrome", dysphagia (trouble swallowing), dumping syndrome, excessive scarring, vagus nerve injury and, rarely, achalasia.[14] The fundoplication can also come undone over time in about 5–10% of cases, leading to recurrence of symptoms. If the symptoms warrant a repeat surgery, the surgeon may use Marlex or another form of artificial mesh to strengthen the connection.[15] Postoperative ileus, which is common after abdominal surgery, is possible.
In "gas bloat syndrome", fundoplication can alter the mechanical ability of the stomach to eliminate swallowed air by
Acute
Vomiting is sometimes impossible or, if not, very painful after a fundoplication, with the likelihood of this complication typically decreasing in the months after surgery. In some cases, the purpose of this operation is to correct excessive vomiting. Initially, vomiting is impossible; however, small amounts of vomit may be produced after the wrap settles over time, and in extreme cases such as
See also
References
- ^ doi:10.1038/gimo56 (inactive 31 January 2024).)
{{cite journal}}: CS1 maint: DOI inactive as of January 2024 (link - NAID 10008497300.
- S2CID 29470586.
- PMID 15622007.
- PMID 25339814.
- ^ S2CID 278325.
- ^ PMID 26629969.
- S2CID 242477061.
- S2CID 150096013.
- PMID 9600280.
- S2CID 23663135.
- PMID 29305934.
- S2CID 231746674.
- PMID 10695014.
- PMID 10323431.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - ^ a b Booth, M.I. (2003). "Treatments: What Is the Current Rate of Gas-Bloat Syndrome Following Open and Laparoscopic Antireflux Surgery?". In Giuli, R.; Siewert, J.R; Couturier, D.; Scarpignato, C. (eds.). Barrett's Esophagus. Vol. 6. OESO, UNESCO.
- S2CID 20831084.
- ^ PMID 8931410.
- ^ PMID 29899438.
- PMID 23267868.
- S2CID 6795623.
