Rapidly progressive glomerulonephritis
| Rapidly progressive glomerulonephritis | |
|---|---|
| Other names | Crescentic glomerulonephritis[1] |
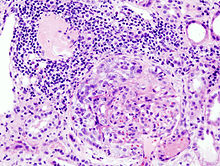 | |
| Histopathological image of crescentic glomerulonephritis in a patient with MPO-ANCA positive rapid progressive glomerulonephritis. Hematoxylin & eosin stain. | |
| Specialty | Nephrology |
| Symptoms | Hematuria[2] |
| Types | Type I, II and III[3] |
| Diagnostic method | Serum analysis[2] |
| Treatment | Corticosteroids |
Rapidly progressive glomerulonephritis (RPGN) is a
Signs and symptoms
Most types of RPGN are characterized by severe and rapid loss of kidney function with marked
Pathophysiology

It is thought that
Diagnosis
Impaired kidney function in an individual who has had the condition for fewer than three months is characteristic of RPGN. An
Classification

RPGN can be classified into three types, based upon the immunofluorescence patterns:[3]
Type I
Accounting for approximately 3
Type II
Characterized by deposition of
Type III
Also known as pauci-immune RPGN, type III RPGN accounts for 55% of RPGN and features neither immune complex deposition nor anti-GBM antibodies. Instead, the glomeruli are damaged in an undefined manner, perhaps through the activation of neutrophils in response to ANCA. Type III RPGN may be isolated to the glomerulus (primary, or idiopathic) or associated with a systemic disease (secondary). In most cases of the latter, the systemic disease is an ANCA-associated vasculitis such as granulomatosis with polyangiitis, microscopic polyangiitis or eosinophilic granulomatosis with polyangiitis.[2]
Treatment
Therapy consists of a combination of rituximab,
Epidemiology
The
References
- ^ RESERVED, INSERM US14-- ALL RIGHTS. "Orphanet: Rapidly progressive glomerulonephritis". www.orpha.net. Retrieved 31 July 2019.
{{cite web}}: CS1 maint: numeric names: authors list (link) - ^ ISBN 978-0-7216-0187-8.
- ^ ISBN 978-1-4200-8478-8.
- ^ a b TheFreeDictionary > rapidly progressive glomerulonephritis Citing: McGraw-Hill Concise Dictionary of Modern Medicine. 2002
- ^ a b c eMedicine > Glomerulonephritis, Crescentic Author: Malvinder S Parmar. Updated: Sep 25, 2008
- ^ "rapidly progressive glomerulonephritis" at Dorland's Medical Dictionary
- PMID 32132388.
- ^ "Rapidly Progressive Glomerulonephritis: Background, Pathophysiology, Epidemiology". 2018-04-05.
- PMID 4125698.
- PMID 21751663. Retrieved 31 October 2015.
- ^ https://www.msdmanuals.com/professional/multimedia/table/classification-of-rapidly-progressive-glomerulonephritis-based-on-immunofluorescence-microscopy
- ^ https://www.msdmanuals.com/professional/multimedia/table/classification-of-rapidly-progressive-glomerulonephritis-based-on-immunofluorescence-microscopy
- ^ PMID 25815169.
- ^ PMID 28842398.
- PMID 11007827.
Further reading
- Greenhall, George H. B.; Salama, Alan D. (2015-02-19). "What is new in the management of rapidly progressive glomerulonephritis?". Clinical Kidney Journal. 8 (2): 143–50. PMID 25815169.
