Pulmonary alveolus
| Pulmonary alveolus | |
|---|---|
 The alveoli | |
| Details | |
| System | Respiratory system |
| Location | Lung |
| Identifiers | |
| Latin | alveolus pulmonis |
| MeSH | D011650 |
| TH | H3.05.02.0.00026 |
| FMA | 7318 |
| Anatomical terminology | |
A pulmonary alveolus (pl.: alveoli, from Latin alveolus, "little cavity"), also known as an air sac or air space, is one of millions of hollow, distensible cup-shaped cavities in the
Alveoli are first located in the
Alveoli are particular to mammalian lungs. Different structures are involved in gas exchange in other vertebrates.[9]
Structure
The alveoli are first located in the respiratory bronchioles as scattered outpockets, extending from their lumens. The respiratory bronchioles run for considerable lengths and become increasingly alveolated with side branches of alveolar ducts that become deeply lined with alveoli. The ducts number between two and eleven from each bronchiole.[10] Each duct opens into five or six alveolar sacs into which clusters of alveoli open.
Each terminal respiratory unit is called an acinus and consists of the respiratory bronchioles, alveolar ducts, alveolar sacs, and alveoli. New alveoli continue to form until the age of eight years.[5]
A typical pair of
Microanatomy
An alveolus consists of an
In the alveolar walls there are interconnecting air passages between the alveoli known as the

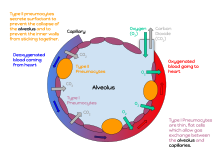
There are three major types of alveolar cell. Two types are pneumocytes or pneumonocytes known as type I and type II cells found in the alveolar wall, and a large phagocytic cell known as an alveolar macrophage that moves about in the lumens of the alveoli, and in the connective tissue between them. Type I cells, also called type I pneumocytes, or type I alveolar cells, are squamous, thin and flat and form the structure of the alveoli. Type II cells, also called type II pneumocytes or type II alveolar cells, release pulmonary surfactant to lower surface tension, and can also differentiate to replace damaged type I cells.[12][15]
Development
Development of the earliest structures that will contain alveoli begins on day 22 and is divided into five stages: embryonic, pseudoglandular, canalicular, saccular, and alveolar stage.[16] The alveolar stage begins approximately 36 weeks into development. Immature alveoli appear as bulges from the sacculi which invade the primary septa. As the sacculi develop, the protrusions in the primary septa become larger; new septations are longer and thinner and are known as secondary septa.[16] Secondary septa are responsible for the final division of the sacculi into alveoli. Majority of alveolar division occurs within the first 6 months but continue to develop until 3 years of age. To create a thinner diffusion barrier, the double-layer capillary network fuse into one network, each one closely associated with two alveoli as they develop.[16]
In the first three years of life, the enlargement of lungs is a consequence of the increasing number of alveoli; after this point, both the number and size of alveoli increases until the development of lungs finishes at approximately 8 years of age.[16]
Function
Type I cells


Type I cells are the larger of the two cell types; they are thin, flat epithelial lining cells (membranous pneumocytes), that form the structure of the alveoli.[3] They are squamous (giving more surface area to each cell) and have long cytoplasmic extensions that cover more than 95% of the alveolar surface.[12][17]
Type I cells are involved in the process of gas exchange between the alveoli and blood. These cells are extremely thin – sometimes only 25 nm – the electron microscope was needed to prove that all alveoli are lined with epithelium. This thin lining enables a fast diffusion of gas exchange between the air in the alveoli and the blood in the surrounding capillaries.
The nucleus of a type I cell occupies a large area of free cytoplasm and its
The cytoplasm in the thin portion contains pinocytotic vesicles which may play a role in the removal of small particulate contaminants from the outer surface. In addition to desmosomes, all type I alveolar cells have occluding junctions that prevent the leakage of tissue fluid into the alveolar air space.
The relatively low solubility (and hence rate of diffusion) of oxygen necessitates the large internal surface area (about 80 square m [96 square yards]) and very thin walls of the alveoli. Weaving between the capillaries and helping to support them is an extracellular matrix, a meshlike fabric of elastic and collagenous fibres. The collagen fibres, being more rigid, give the wall firmness, while the elastic fibres permit expansion and contraction of the walls during breathing.
Type I pneumocytes are unable to replicate and are susceptible to toxic insults. In the event of damage, type II cells can proliferate and differentiate into type I cells to compensate.[18]
Type II cells
Type II cells are cuboidal and much smaller than type I cells.
Type II cells start to develop at about 26 weeks of gestation, secreting small amounts of surfactant. However, adequate amounts of surfactant are not secreted until about 35 weeks of gestation – this is the main reason for increased rates of infant respiratory distress syndrome, which drastically reduces at ages above 35 weeks gestation.
Type II cells are also capable of cellular division, giving rise to more type I and II alveolar cells when the lung tissue is damaged.[21]
The importance of the type 2 lung alveolar cells in the development of severe respiratory symptoms of COVID-19 and potential mechanisms on how these cells are protected by the SSRIs fluvoxamine and fluoxetine was summarized in a review in April 2022.[23]
Alveolar macrophages
The alveolar macrophages reside on the internal luminal surfaces of the alveoli, the alveolar ducts, and the bronchioles. They are mobile scavengers that serve to engulf foreign particles in the lungs, such as dust, bacteria, carbon particles, and blood cells from injuries.[24] They are also called pulmonary macrophages, and dust cells.
Clinical significance
Diseases
Surfactant
Insufficient surfactant in the alveoli is one of the causes that can contribute to atelectasis (collapse of part or all of the lung). Without pulmonary surfactant, atelectasis is a certainty.[25] The severe condition of acute respiratory distress syndrome (ARDS) is caused by a deficiency or dysfunction of surfactant.[26] Insufficient surfactant in the lungs of preterm infants causes infant respiratory distress syndrome (IRDS). The lecithin–sphingomyelin ratio is a measure of fetal amniotic fluid to indicate lung maturity or immaturity.[27] A low ratio indicates a risk factor for IRDS. Lecithin and sphingomyelin are two of the glycolipids of pulmonary surfactant.
Impaired surfactant regulation can cause an accumulation of surfactant proteins to build up in the alveoli in a condition called pulmonary alveolar proteinosis. This results in impaired gas exchange.[28]
Inflammation
- Diffuse alveolar damage can be a cause of acute respiratory distress syndrome(ARDS) a severe inflammatory disease of the lung.[31]: 187
- In photochemical smogfor example, as well as substances to which a person is allergic.
- abundance of mucusis produced by the lungs. The production of mucus occurs naturally when the lung tissue is exposed to irritants. In chronic bronchitis, the air passages into the alveoli, the respiratory bronchioles, become clogged with mucus. This causes increased coughing in order to remove the mucus, and is often a result of extended periods of exposure to cigarette smoke.
- Hypersensitivity pneumonitis
Structural

Almost any type of lung tumor or lung cancer can compress the alveoli and reduce gas exchange capacity. In some cases the tumor will fill the alveoli.[32]
- Cavitary pneumoniais a process in which the alveoli are destroyed and produce a cavity. As the alveoli are destroyed, the surface area for gas exchange to occur becomes reduced. Further changes in blood flow can lead to decline in lung function.
- Emphysema is another disease of the lungs, whereby the elastin in the walls of the alveoli is broken down by an imbalance between the production of neutrophil elastase (elevated by cigarette smoke) and alpha-1 antitrypsin (the activity varies due to genetics or reaction of a critical methionine residue with toxins including cigarette smoke). The resulting loss of elasticity in the lungs leads to prolonged times for exhalation, which occurs through passive recoil of the expanded lung. This leads to a smaller volume of gas exchanged per breath.
- Pulmonary alveolar microlithiasis is a rare lung disorder of small stone formation in the alveoli.
Fluid
A pulmonary contusion is a bruise of the lung tissue caused by trauma.[33] Damaged capillaries from a contusion can cause blood and other fluids to accumulate in the tissue of the lung, impairing gas exchange.
Pulmonary edema is the buildup of fluid in the parenchyma and alveoli. An edema is usually caused by left ventricular heart failure, or by damage to the lung or its vasculature.
Because of the high expression of
Additional images
-
Blood circulation around alveoli
-
Diagrammatic view of lung showing magnified inner structures including alveolar sacs at 10) and lobules at 9)
See also
References
- ^ "Pulmonary Gas Exchange - MeSH - NCBI". www.ncbi.nlm.nih.gov. Retrieved 30 December 2022.
- ^ "Alveoli". www.cancer.gov. 2 February 2011. Retrieved 22 July 2021.
- ^ PMID 30390118.
- ^ Jones, Jeremy. "Lung parenchyma | Radiology Reference Article | Radiopaedia.org". Radiopaedia. Retrieved 15 August 2021.
- ^ ISBN 978-1-4963-4721-3.
- PMID 1141138.
- ^ Hogan CM (2011). "Respiration". In McGinley M, Cleveland CJ (eds.). Encyclopedia of Earth. Washington, D.C.: National council for Science and the Environment.
- ^ Paxton S, Peckham M, Knibbs A (2003). "Functions of the Respiratory Portion". The Leeds Histology Guide. Faculty of Biological Sciences, University of Leeds.
- PMID 12869615.
- ^ ISBN 0-07-105448-0.
- PMID 14512270.
- ^ ISBN 978-0-323-04582-7.
- ^ "Bronchi, Bronchial Tree & Lungs". SEER Training Modules. U.S. Department of Health and Human Services National Institutes of Health National Cancer Institute.
- ISBN 978-1-4160-4574-8.
- PMID 30020685. Retrieved 12 September 2021.
- ^ PMID 31335092.
- ISBN 978-0-323-52371-4.
- ^ ISBN 978-0-7020-7705-0.
- ^ Ross MH, Pawlina W (2011). Histology, A Text and Atlas (Sixth ed.).
- PMID 11686863.
- ^ "Lung – Regeneration – Nonneoplastic Lesion Atlas". National Toxicology Program. National Institute of Environmental Health Sciences, National Institutes of Health, U.S. Department of Health and Human Services. Retrieved 2018-05-18.
- PMID 9850098.
- PMID 35409171.
- ^ "The trachea and the stem bronchi". Encyclopædia Britannica. Encyclopædia Britannica, Inc.
- ISBN 978-0-07-322804-4.
- PMID 33242393.
- PMID 18773379.
- S2CID 27932336.
- ^ "Pneumonia – Symptoms and causes". Mayo Clinic. Retrieved 2019-06-10.
- ^ "Pneumonia Symptoms and Diagnosis". American Lung Association. Retrieved 2019-06-10.
- ISBN 978-0-7020-3085-7.
- ISBN 0-07-105448-0.
- ^ "Pulmonary Contusion – Injuries and Poisoning". Merck Manuals Consumer Version. Retrieved 2019-06-10.
- PMID 20599443.
- PMID 32094336.
External links
- Pulmonary+Alveoli at the U.S. National Library of Medicine Medical Subject Headings (MeSH)


