Spanish flu research
| Influenza A virus subtype H1N1 | |
|---|---|
| |
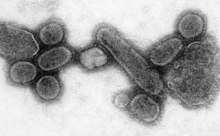
| An electron micrograph of the virus that caused the 1918 flu.
| |
| Virus classification | |
| (unranked): | Virus |
| Realm: | Riboviria |
| Kingdom: | Orthornavirae |
| Phylum: | Negarnaviricota
|
| Class: | Insthoviricetes |
| Order: | Articulavirales |
| Family: | Orthomyxoviridae |
| Genus: | Alphainfluenzavirus |
| Species: | |
| Serotype: | Influenza A virus subtype H1N1
|
| Sampled strains | |
| |
Spanish flu research concerns studies regarding the causes and characteristics of the
Origin of virus
There are two prevailing theories usually postulated.[citation needed] One theory by Alfred W. Crosby is that the virus strain originated at Fort Riley, Kansas, by two genetic mechanisms – genetic drift and antigenic shift – in viruses in poultry and swine which the fort bred for local consumption. Though initial data from a recent reconstruction of the virus suggested that it jumped directly from birds to humans, without traveling through swine,[a] this has since been cast into doubt. One researcher published in 2004 argued that the disease was found in Haskell County, Kansas, as early as January 1918.[2] A similar and even more deadly virus had been seen earlier at British camps in France and at Aldershot.[3]
Earlier investigative work published in 2000 by a team led by British virologist, John Oxford[4] of St Bartholomew's Hospital and the Royal London Hospital, suggested that a principal British troop staging camp in Étaples, France, was at the center of the 1918 flu pandemic or at least a significant precursor virus to it. There had been a mysterious respiratory infection at the military base during the winter of 1915–1916.[5]
Discovery of viral genomes


In 1995, Jeffery Taubenberger of the US Armed Forces Institute of Pathology (AFIP), wondered if it might be possible to recover the virus of 1918 flu pandemic from the dried and fixed tissue of victims. He and his colleagues, tested 10 slides of tissue sample and 2 came out positive. Taubenberger, Ann H. Reid and Thomas G. Fanning were able to amplify short segments of the viral nucleic acid using polymerase chain reaction (PCR).[6] The results were published in the journal Science in March 1997.[7]
On August 20, 1997, Johan Hultin recovered samples of the 1918 influenza from the frozen corpse of a Native Alaskan woman buried for nearly eight decades in permafrost near Brevig Mission, Alaska.[8] He brought the samples to a team in Rockville, Maryland led by Jeffery Taubenberger of the US Armed Forces Institute of Pathology (AFIP). Brevig Mission lost approximately 85% of its population to the 1918 flu in November 1918. One of the four recovered samples contained viable genetic material of the virus. This sample provided scientists a first-hand opportunity to study the virus, which was inactivated with guanidinium thiocyanate before transport. This sample and others found in AFIP archives allowed researchers to completely analyze the critical gene structures of the 1918 virus.
- "We have now identified three cases: The
The archived autopsy samples had been taken from WWI Army privates Roscoe Vaughan and James Downs.[11]
The 6 February 2004 edition of responsible for the flu outbreak of 1918. They did this by piecing together DNA from a lung sample from an Inuit woman buried in the Alaskan tundra and a number of preserved samples from American soldiers of the First World War. The teams had analyzed the structure of the gene and discovered how subtle alterations to the shape of a protein molecule had allowed it to move from birds to humans with such devastating effects.
On 5 October 2005, Tumpey and other researchers at the
Characteristics of virus
In July 2004, researchers led by H. Deng of the
In December 2008, research by Yoshihiro Kawaoka of
Research of viral pathogenesis
Recent research of Taubenberger et al. has suggested that the 1918 virus, like H5N1, could have arisen directly from an avian influenza virus.[13] However, researchers at University of Virginia and Australian National University have suggested that there may be an alternative interpretation of the data used in the Taubenberger et al. paper.[19][20] Taubenberger et al. responded to these letters and defended their original interpretation.[21]
Other research by Tumpey and colleagues who reconstructed the
The sequences of the polymerase proteins (PA, PB1, and PB2) of the 1918 virus and subsequent human viruses differ by only 10 amino acids from the avian influenza viruses. Viruses with 7 of the 10 amino acids in the human influenza locations have already been identified in currently circulating
Another important factor is the change of the HA protein to a binding preference for alpha-2,6
Blood plasma as an effective treatment
In the event of another pandemic, US military researchers have proposed reusing a treatment from the deadly pandemic of 1918 in order to blunt the effects of the flu: Some military doctors injected severely afflicted patients with blood or blood plasma from people who had recovered from the flu. Data collected during that time indicates that the blood-injection treatment reduced mortality rates by as much as 50 percent.[23]
Navy researchers have launched a test to see if the 1918 treatment will work against deadly Asian bird flu. Results thus far have been inconclusive.
In the worldwide
See also
- Influenza research
- Mark Sykes – exhumation of a British flu victim in the United Kingdom
- Yoshihiro Kawaoka – engineered and recreated a virus to study how it works and how the flu naturally mutates
- Kirsty Duncan - led unsuccessful expedition to find flu virus in permafrost at Longyearbyen, Svalbard, Norway
Footnotes
- Spanish Flu' in 1918 appears to be entirely derived from an avian source." (Belshe, 2005)[1]
- ^ Johan Hultin first attempted to recover samples from Brevig in 1951, but was unsuccessful. In 1997, by then a seventy-two-year-old retired pathologist, Hultin decided that science had advanced enough to make another attempt worthwhile. Taubenberger had already recovered RNA of limited quality from samples of two servicemen who had died in the pandemic, and Hultin wrote offering his services to try to get better quality samples from Brevig permafrost. Taubenberger accepted, and Hultin went alone to Brevig in August 1997, and recovered the sample from the Alaskan woman, which Taubenberger and his team then analysed.[10]
References
- ^ Harder, Timm C.; Werner, Ortrud (2006). "Chapter Two: Avian Influenza" (free on-line book). Influenza Report (Report).
a medical textbook that provides a comprehensive overview of epidemic and pandemic influenza.
- PMID 14733617.
- ^ Valentine, Vikki (20 February 2006). "Origins of the 1918 pandemic: The case for France". NPR. National Public Radio (NPR). 5222069.
- ^ "Dr. John Oxford". EU Research Profile. Archived from the original on 26 December 2008.
- ^ Connor, Steve (8 January 2000). "Flu epidemic traced to Great War transit camp". The Independent. UK. Archived from the original on 8 August 2009. Retrieved 26 March 2020.
An investigation into the global epidemic of influenza in 1918, which killed an estimated 40 million people, has shown it almost certainly started in an army camp in France in the middle of the First World War.
- ISSN 0190-8286. Retrieved 2020-07-25.
- S2CID 8976173.
- ^ Brown, David (10 October 2005). "Resurrecting 1918 flu virus took many turns". Washington Post.
- ^ "Lethal secrets of 1918 flu virus". BBC News.
- ISBN 978-0-374-15706-7.
- ^ "Closing in on a killer: Scientists unlock clues to the Spanish influenza virus". National Museum of Health and Medicine. Archived from the original on 2 May 2020. Retrieved 23 March 2020.
- PMID 16208326.
- ^ S2CID 4405787.
- ^ S2CID 14773861.
- PMID 16306617.
- PMID 16226289.
- PMID 15235128.
- ^ "Researchers unlock secrets of 1918 flu pandemic". Reuters. 29 December 2008.
- S2CID 4422599.
- S2CID 4382489.
- S2CID 4308033.
- S2CID 4431644.
- ^ "Influenza (main)". history.navy.mil.
- ^ "Experts: Use 1918 Methods to Fight Pandemic". NPR.org. Retrieved 2021-03-03.
- ^ "[no title cited]". National Public Radio (NPR). 5731688.
- ^ "The Threat of Pandemic Influenza: Are we ready?" (free online book). www.ncbi.nlm.nih.gov. Workshop Summary. National Institutes of Health. 2005. p. 62.
