Rickettsia typhi
Rickettsia typhi is a small,
R. typhi was once one of the most prevalent causes of rickettsial diseases worldwide, but has since experienced a drop in case reports with the implementation of pest control programs.[8][9][10] The microorganism is concentrated in warmer climate and coastal ports where there is an abundance of rats and their fleas, which are the preferred hosts for the pathogen.[8][9] R. typhi is transmitted between competent flea and mammalian hosts through flea bites and contact with infected feces and tissues.[8][11]
There are several
| Rickettsia typhi | |
|---|---|
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Pseudomonadota |
| Class: | Alphaproteobacteria |
| Order: | Rickettsiales |
| Family: | Rickettsiaceae |
| Genus: | Rickettsia |
| Species group: | Typhus group |
| Species: | R. typhi
|
| Binomial name | |
| Rickettsia typhi (Wolbach and Todd, 1920) Philip, 1943
| |
History and taxonomy

In the early 20th century
Cellular morphology and motility
Rickettsia typhi is a small,
Virulence
Rickettsia typhi is a flea-borne disease organism and is widely distributed throughout the world.[18] There are two cycles in R. typhi transmission from animal reservoirs to human: a classic rat-flea-rat cycle, and a peridomestic cycle involving cats, dogs, opossums, sheep, and their fleas.[7]
Classic rat-flea-rat cycle
R. typhi circulates amongst rats (
Transmission of R. typhi from the rat flea is affected by contact with rickettsia-containing flea feces during or after blood feeding, as well as via flea bite.[14] The rickettsiae have no harmful effects on the fitness of either the vector or the rat, showing a true mutual relationship.[21] Infected fleas can maintain R. typhi for life, giving them potential for infecting large number of susceptible hosts.[21]
Peridomestic cycle
Thus far, there have not been many studies on the periodomestic animal cycle of transmission, with the majority that have been done focusing on cats.
It has been shown that R. typhi can be present in cats and the cat flea,
There is also some evidence that other domestic animals such as dogs and sheep,[25] as well as opossums,[23] could be involved in the R. typhi transmission cycle, but studies are currently limited.
Pathogenesis
Rickettsia spp. including R. typhi enter the skin and spread through the bloodstream to infect the endothelium lining the blood vessels. This leads to vascular inflammation, damage to vascular integrity, and compromised vascular permeability, which is collectively known as 'Rickettsial vasculitis' [7]
Disease
Murine typhus (endemic typhus) in humans
Rickettsia typhi is a causative agent of
Epidemiology

Geographical and temporal distribution
Rickettsia typhi is a small,
Historically, thousands of murine typhus cases were reported in the United States every year;[8][9][10][14] however, the disease experienced a sudden decline in incidence in the 1940s with the implementation of pest control programs to remove the flea and rodent reservoirs responsible for rickettsial transmission in urban dwellings.[8][14] Murine typhus infections in the present are more sporadic and infrequent, with fewer than 100 cases reported in the US annually.[9][14] Nevertheless, R. typhi is still regarded as a bacterium of considerable public health significance, and outbreaks are commonly reported in the Southern US, Southern Europe, Asia, Africa, and Australia.[8][9][10][14] It is estimated that R. typhi prevalence is actually higher than the measured value, since murine typhus is often underreported and misdiagnosed because of its non-specific and mild clinical presentation (fever, headache, generalized pain, and rashes).[9][10][14][25] Undiagnosed infections are predicted to outnumber reported cases by 4:1.[14] A recent study presented a clinical case of a patient that works in the Brazilian Amazon and presented an unspecific febrile illness probably caused by Rickettsia typhi since the patient presented specific antibodies to this bacteria. This shows that the R. typhi geographical distribution can be wider than expected.[31]
Host range and transmission

The R. typhi
The bacterium transmits from an infected rat (or other mammalian host) to a susceptible rat flea (or other arthropod vector) through a blood meal, and is then transmitted from an infected flea to another susceptible rat through direct contact with the infectious feces or tissues of the vector.[8][14][11] Transmission through contact with arthropod feces may be through an open wound, the respiratory tract (inhalation), or the conjunctivae of the mammalian host.[14] There is evidence that flea bite transmission is possible as well after the bacterium undergoes a certain incubation period in the arthropod vector.[14] Female fleas can also pass the infection onto offspring through transovarial transmission.[8][14] R. typhi appears to be in a truly commensal relationship with these insect and non-human hosts, as it only produces an asymptomatic infection that has no effect on host life span or reproductivity.[14] Because of its versatility in transmission, the R. typhi bacterium is very successful in perpetuating its numbers in endemic regions.[14]
Zoonotic potential
As with all rickettsiae species, R. typhi is a
Diagnosis and identification
The laboratory tests available for the diagnosis of Rickettsial species includes: shell vial assay, PCR-based detection, immunodetection, circulating endothelial cells, and serodiagnostic tests such as the Weil-Felix test, CF test, ELISA, microimmunofluorescence, immunoperoxidase, line blot and Western immunoblot tests.[6]
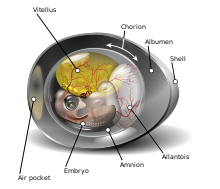
Traditionally, the diagnosis of Rickettsia was based on serology[33] However, serologic tests take about 15 days after the onset of symptoms for there to be diagnostically significant titers of R. tyhpi.[34] And so the diagnosis is often confirmed after the patient has either recovered or died.[6] R. typhi are not able to grow in axenic or sterile conditions, and must be grown in tissue, or embryo samples.[16] Even when stringent physiologic conditions are met, when grown in media that mimics the environment of host cytoplasm, pathogen activity cannot survive very long.[16] A common method for growing R. typhi is through the yolk sacs of embryonic eggs.[16]
Laboratory techniques such as real-time PCR and microimmunofluorescence can be used to identify Rickettsia down to the species level.[35][5] Microimmunofluorescence is a highly sensitive test that is often used in endemic areas to confirm infection by R. typhi.[10] The use of real-time PCR can allow for the detection and confirmation of R. typhi earlier than serological tests.[35] Membrane protein ompB and prsA gene fragments have been shown to be identifiable markers in qPCR for R. typhi.[36]
Differentiation from R. prowazekii
Bibliography
- ^ PMID 15317790.
- ^ PMID 21912565.
- ^ S2CID 24176171.
- PMID 29912688.
- ^ PMID 8027348.
- ^ PMID 9350721.
- ^ PMID 19327117.
- ^ ISBN 978-1-4377-2702-9, retrieved 2020-10-06
- ^ PMID 11231808.
- ^ PMID 8027348.
- ^ PMID 29769278.
- ^ S2CID 74156662.
- PMID 11231808.
- ^ PMID 2105686.
- PMID 29912688.
- ^ ISBN 9780123971692.
- S2CID 84913142.
- PMID 9284376.
- ^ PMID 705902.
- ^ PMID 18826827.
- ^ PMID 19036234.
- PMID 23940746.
- ^ PMID 20202415.
- PMID 8447530.
- ^ PMID 23290118.
- ^ PMID 18260783.
- ^ PMID 16893625.
- PMID 9346184.
- PMID 2499181.
- ^ ISBN 978-1-4557-4801-3, retrieved 2020-09-10
- PMID 32818424.
- S2CID 1675131.
- ^ "Rickettsia typhi (Murine typhus)- Infectious Disease and Antimicrobial Agents". www.antimicrobe.org. Retrieved 2020-09-23.
- PMID 1880866.
- ^ PMID 22098502.
- S2CID 1682815.
- PMID 23595041.
- ^ PMID 10882661.
