Inflammation
This article needs more primary sources. (March 2021) |  |
| Inflammation | |
|---|---|
autoimmune disorder |
Inflammation (from
Inflammation is a generic response, and therefore is considered a mechanism of innate immunity, whereas adaptive immunity is specific to each pathogen.[3]
Inflammation is a protective response involving
.Inflammation can be classified as acute or chronic. Acute inflammation is the initial response of the body to harmful stimuli, and is achieved by the increased movement of
Inflammation has also been classified as Type 1 and Type 2 based on the type of
The term inflammation is not a synonym for infection. Infection describes the interaction between the action of microbial invasion and the reaction of the body's inflammatory response—the two components are considered together in discussion of infection, and the word is used to imply a microbial invasive cause for the observed inflammatory reaction. Inflammation, on the other hand, describes just the body's immunovascular response, regardless of cause. But, because of the two are often correlated, words ending in the suffix -itis (which means inflammation) are sometimes informally described as referring to infection: for example, the word urethritis strictly means only "urethral inflammation", but clinical health care providers usually discuss urethritis as a urethral infection because urethral microbial invasion is the most common cause of urethritis.
However, the inflammation–infection distinction is crucial in situations in
Causes
- Burns[6]
- Frostbite
- Physical injury, blunt or penetrating[7]
- Foreign bodies, including splinters, dirt and debris
- Trauma[6]
- Ionizing radiation
Biological:
- Infection by pathogens[6]
- Immune reactions due to hypersensitivity
- Stress
Chemical:[6]
Psychological:
- Excitement[8]
Types
|
|
| Acute | Chronic | |
|---|---|---|
| Causative agent | Bacterial pathogens, injured tissues | Persistent acute inflammation due to non-degradable pathogens, viral infection, persistent foreign bodies, or autoimmune reactions |
| Major cells involved | neutrophils (primarily), basophils (inflammatory response), and eosinophils (response to helminth worms and parasites), mononuclear cells (monocytes, macrophages) | Mononuclear cells (monocytes, macrophages, lymphocytes, plasma cells), fibroblasts |
| Primary mediators | Vasoactive amines, eicosanoids | IFN-γ and other cytokines, growth factors, reactive oxygen species, hydrolytic enzymes |
| Onset | Immediate | Delayed |
| Duration | Few days | Up to many months, or years |
| Outcomes | Resolution, abscess formation, chronic inflammation | Tissue destruction, fibrosis, necrosis |
Acute
Acute inflammation is a short-term process, usually appearing within a few minutes or hours and begins to cease upon the removal of the injurious stimulus.[9] It involves a coordinated and systemic mobilization response locally of various immune, endocrine and neurological mediators of acute inflammation. In a normal healthy response, it becomes activated, clears the pathogen and begins a repair process and then ceases.[10]
Acute inflammation occurs immediately upon injury, lasting only a few days.[11] Cytokines and chemokines promote the migration of neutrophils and macrophages to the site of inflammation.[11] Pathogens, allergens, toxins, burns, and frostbite are some of the typical causes of acute inflammation.[11] Toll-like receptors (TLRs) recognize microbial pathogens.[11] Acute inflammation can be a defensive mechanism to protect tissues against injury.[11] Inflammation lasting 2–6 weeks is designated subacute inflammation.[11][12]
Cardinal signs
| English | Latin |
|---|---|
| Redness | Rubor
|
| Swelling | Tumor
|
| Heat | Calor |
| Pain | Dolor |
| Loss of function | Functio laesa[b] |
Inflammation is characterized by five
(the traditional names of which come from Latin):- Dolor (pain)
- Calor (heat)
- Rubor(redness)
- Tumor (swelling)
- Functio laesa (loss of function)[17]
The first four (classical signs) were described by Celsus (c. 30 BC–38 AD).[18]
Loss of function
The fifth sign, loss of function, is believed to have been added later by
Acute process
This section needs more primary sources. (April 2023) |  |


The process of acute inflammation is initiated by resident immune cells already present in the involved tissue, mainly resident
At the onset of an infection, burn, or other injuries, these cells undergo activation (one of the PRRs recognize a PAMP or DAMP) and release inflammatory mediators responsible for the clinical signs of inflammation. Vasodilation and its resulting increased blood flow causes the redness (rubor) and increased heat (calor). Increased permeability of the blood vessels results in an exudation (leakage) of
In addition to cell-derived mediators, several acellular biochemical cascade systems—consisting of preformed plasma proteins—act in parallel to initiate and propagate the inflammatory response. These include the
Acute inflammation may be regarded as the first line of defense against injury. Acute inflammatory response requires constant stimulation to be sustained. Inflammatory mediators are short-lived and are quickly degraded in the tissue. Hence, acute inflammation begins to cease once the stimulus has been removed.[9]
Chronic
Chronic inflammation is inflammation that lasts for months or years.
Cardinal signs
Common signs and symptoms that develop during chronic inflammation are:[12]
- Body pain, arthralgia, myalgia
- Chronic fatigue and insomnia
- Depression, anxiety and mood disorders
- Gastrointestinal complications such as constipation, diarrhea, and acid reflux
- Weight gain or loss
- Frequent infections
Vascular component
This section needs more primary sources. (March 2021) |  |
Vasodilation and increased permeability
As defined, acute inflammation is an immunovascular response to inflammatory stimuli, which can include infection or trauma.
Upon contact with PAMPs, tissue
Acute inflammation is characterized by marked vascular changes, including
Plasma cascade systems
- The MAC.
- The kinin systemgenerates proteins capable of sustaining vasodilation and other physical inflammatory effects.
- The coagulation systemor clotting cascade, which forms a protective protein mesh over sites of injury.
- The fibrinolysis system, which acts in opposition to the coagulation system, to counterbalance clotting and generate several other inflammatory mediators.
Plasma-derived mediators
* non-exhaustive list
| Name | Produced by | Description |
|---|---|---|
| Bradykinin | Kinin system |
A vasoactive protein that is able to induce vasodilation, increase vascular permeability, cause smooth muscle contraction, and induce pain. |
C3 |
Complement system | Cleaves to produce C3a and C3b. C3a stimulates histamine release by mast cells, thereby producing vasodilation. C3b is able to bind to bacterial cell walls and act as an opsonin, which marks the invader as a target for phagocytosis. |
| C5a | Complement system | Stimulates histamine release by mast cells, thereby producing vasodilation. It is also able to act as a chemoattractant to direct cells via chemotaxis to the site of inflammation.
|
| Factor XII (Hageman Factor) | Liver | A protein that circulates inactively, until activated by collagen, platelets, or exposed basement membranes via conformational change. When activated, it in turn is able to activate three plasma systems involved in inflammation: the kinin system, fibrinolysis system, and coagulation system. |
Membrane attack complex |
Complement system | A complex of the complement proteins . The combination and activation of this range of complement proteins forms the membrane attack complex, which is able to insert into bacterial cell walls and causes cell lysis with ensuing bacterial death. |
| Plasmin | Fibrinolysis system |
Able to break down fibrin clots, cleave complement protein C3, and activate Factor XII. |
| Thrombin | Coagulation system |
Cleaves the soluble plasma protein blood clot. Thrombin can also bind to cells via the PAR1 receptor to trigger several other inflammatory responses, such as production of chemokines and nitric oxide .
|
Cellular component
The cellular component involves
Leukocyte extravasation

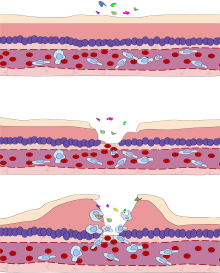
Various
- Leukocyte margination and endothelial adhesion: The white blood cells within the vessels which are generally centrally located move peripherally towards the walls of the vessels.G protein-coupled receptorsthat activates integrins on the leukocyte surface for firm adhesion. Such activation increases the affinity of bound integrin receptors for ICAM-1 and VCAM-1 on the endothelial cell surface, firmly binding the leukocytes to the endothelium.
- Migration across the endothelium, known as transmigration, via the process of diapedesis: Chemokine gradients stimulate the adhered leukocytes to move between adjacent endothelial cells. The endothelial cells retract and the leukocytes pass through the basement membrane into the surrounding tissue using adhesion molecules such as ICAM-1.[29]
- Movement of leukocytes within the tissue via chemoattractants, for example, C3a or C5, and cause the leukocytes to move along a chemotactic gradient towards the source of inflammation.
Phagocytosis
Extravasated neutrophils in the cellular phase come into contact with microbes at the inflamed tissue.
Upon endocytic PRR binding,
Phagocytic efficacy can be enhanced by
Cell-derived mediators
* non-exhaustive list
| Name | Type | Source | Description |
|---|---|---|---|
| Lysosome granules | Enzymes | Granulocytes | These cells contain a large variety of enzymes that perform a number of functions. Granules can be classified as either azurophilic depending upon the contents, and are able to break down a number of substances, some of which may be plasma-derived proteins that allow these enzymes to act as inflammatory mediators.
|
| GM-CSF | Glycoprotein | Macrophages, monocytes, T-cells, B-cells, and tissue-resident cells | Elevated GM-CSF has been shown to contribute to inflammation in COVID-19 .
|
| Histamine | Monoamine |
Mast cells and basophils | Stored in preformed granules, histamine is released in response to a number of stimuli. It causes venous permeability, and a wide variety of organ-specific effects.
|
| IFN-γ | Cytokine | T-cells, NK cells | Antiviral, immunoregulatory, and anti-tumour properties. This interferon was originally called macrophage-activating factor, and is especially important in the maintenance of chronic inflammation. |
| IL-6 | Cytokine and Myokine | Macrophages, osteoblasts, adipocytes, and smooth muscle cells (cytokine) Skeletal muscle cells (myokine) | Pro-inflammatory cytokine secreted by macrophages in response to pathogen-associated molecular patterns (PAMPs); pro-inflammatory cytokine secreted by adipocytes, especially in obesity; anti-inflammatory myokine secreted by skeletal muscle cells in response to exercise. |
| IL-8 | Chemokine | Primarily macrophages | Activation and chemoattraction of neutrophils, with a weak effect on monocytes and eosinophils. |
| Leukotriene B4 | Eicosanoid | Leukocytes , cancer cells |
Able to mediate leukocyte adhesion and activation, allowing them to bind to the endothelium and migrate across it. In neutrophils, it is also a potent chemoattractant, and is able to induce the formation of reactive oxygen species and the release of lysosomal enzymes by these cells. |
LTD4 |
Eicosanoid | macrophages |
These three Cysteine-containing leukotrienes contract lung airways, increase micro-vascular permeability, stimulate mucus secretion, and promote eosinophil-based inflammation in the lung, skin, nose, eye, and other tissues. |
5-oxo-eicosatetraenoic acid |
Eicosanoid | Leukocytes , cancer cells |
Potent stimulator of neutrophil chemotaxis, lysosome enzyme release, and reactive oxygen species formation; monocyte chemotaxis; and with even greater potency eosinophil chemotaxis, lysosome enzyme release, and reactive oxygen species formation. |
5-HETE |
Eicosanoid | Leukocytes |
Metabolic precursor to 5-Oxo-eicosatetraenoic acid, it is a less potent stimulator of neutrophil chemotaxis, lysosome enzyme release, and reactive oxygen species formation; monocyte chemotaxis; and eosinophil chemotaxis, lysosome enzyme release, and reactive oxygen species formation. |
| Prostaglandins | Eicosanoid | Mast cells | A group of lipids that can cause vasodilation, fever, and pain. |
| Nitric oxide | Soluble gas | Macrophages, endothelial cells, some neurons | Potent vasodilator, relaxes smooth muscle, reduces platelet aggregation, aids in leukocyte recruitment, direct antimicrobial activity in high concentrations. |
IL-1 |
Cytokines | Primarily macrophages | Both affect a wide variety of cells to induce many similar inflammatory reactions: fever, production of cytokines, endothelial gene regulation, chemotaxis, leukocyte adherence, activation of fibroblasts. Responsible for the systemic effects of inflammation, such as loss of appetite and increased heart rate. TNF-α inhibits osteoblast differentiation. |
| Tryptase | Enzymes | Mast Cells | This serine protease is believed to be exclusively stored in mast cells and secreted, along with histamine, during mast cell activation.[30][31][32] |
Morphologic patterns
Specific patterns of acute and chronic inflammation are seen during particular situations that arise in the body, such as when inflammation occurs on an
- Granulomatous inflammation: Characterised by the formation of granulomas, they are the result of a limited but diverse number of diseases, which include among others tuberculosis, leprosy, sarcoidosis, and syphilis.
- Fibrinous inflammation: Inflammation resulting in a large increase in vascular permeability allows pseudomembranous colitis), pseudomembranous tubes can be formed.
- Purulent inflammation: Inflammation resulting in large amount of staphylococci is characteristic of this kind of inflammation. Large, localised collections of pus enclosed by surrounding tissues are called abscesses.
- Serous inflammation: Characterised by the copious effusion of non-viscous serous fluid, commonly produced by mesothelial cells of serous membranes, but may be derived from blood plasma. Skin blistersexemplify this pattern of inflammation.
- Ulcerative inflammation: Inflammation occurring near an epithelium can result in the necrotic loss of tissue from the surface, exposing lower layers. The subsequent excavation in the epithelium is known as an ulcer.
Disorders


Inflammatory abnormalities are a large group of disorders that underlie a vast variety of human diseases. The immune system is often involved with inflammatory disorders, as demonstrated in both
Examples of disorders associated with inflammation include:
- Acne vulgaris
- Asthma
- Autoimmune diseases
- Autoinflammatory diseases
- Celiac disease
- Chronic prostatitis
- Colitis
- Diverticulitis
- Familial Mediterranean Fever
- Glomerulonephritis
- Hidradenitis suppurativa
- Hypersensitivities
- Inflammatory bowel diseases
- Interstitial cystitis
- Lichen planus
- Mast Cell Activation Syndrome
- Mastocytosis
- Otitis
- Pelvic inflammatory disease
- Peripheral ulcerative keratitis
- Pneumonia
- Reperfusion injury
- Rheumatic fever
- Rheumatoid arthritis
- Rhinitis
- Sarcoidosis
- Transplant rejection
- Vasculitis
Atherosclerosis
Atherosclerosis, formerly considered a bland lipid storage disease, actually involves an ongoing inflammatory response. Recent advances in basic science have established a fundamental role for inflammation in mediating all stages of atherosclerosis from initiation through progression and, ultimately, the thrombotic complications from it. These new findings provide important links between risk factors and the mechanisms of
Allergy
An allergic reaction, formally known as
Myopathies
Leukocyte defects
Due to the central role of leukocytes in the development and propagation of inflammation, defects in leukocyte functionality often result in a decreased capacity for inflammatory defense with subsequent vulnerability to infection.
Pharmacological
Certain drugs or exogenous chemical compounds are known to affect inflammation.
Cancer
Inflammation orchestrates the
According to a review of 2009, recent data suggests that cancer-related inflammation (CRI) may lead to accumulation of random genetic alterations in cancer cells.[41]
Role in cancer
In 1863, Rudolf Virchow hypothesized that the origin of cancer was at sites of chronic inflammation.[38][42] As of 2012, chronic inflammation was estimated to contribute to approximately 15% to 25% of human cancers.[42][43]
Mediators and DNA damage in cancer
An inflammatory mediator is a messenger that acts on blood vessels and/or cells to promote an inflammatory response.
Inflammation also causes DNA damages due to the induction of reactive oxygen species (ROS) by various intracellular inflammatory mediators.[38][45][42] In addition, leukocytes and other phagocytic cells attracted to the site of inflammation induce DNA damages in proliferating cells through their generation of ROS and reactive nitrogen species (RNS). ROS and RNS are normally produced by these cells to fight infection.[38] ROS, alone, cause more than 20 types of DNA damage.[46] Oxidative DNA damages cause both mutations[47] and epigenetic alterations.[48][42][49] RNS also cause mutagenic DNA damages.[50]
A normal cell may undergo carcinogenesis to become a cancer cell if it is frequently subjected to DNA damage during long periods of chronic inflammation. DNA damages may cause genetic mutations due to inaccurate repair. In addition, mistakes in the DNA repair process may cause epigenetic alterations.[42][45][49] Mutations and epigenetic alterations that are replicated and provide a selective advantage during somatic cell proliferation may be carcinogenic.
Genome-wide analyses of human cancer tissues reveal that a single typical cancer cell may possess roughly 100 mutations in coding regions, 10–20 of which are "driver mutations" that contribute to cancer development.[42] However, chronic inflammation also causes epigenetic changes such as DNA methylations, that are often more common than mutations. Typically, several hundreds to thousands of genes are methylated in a cancer cell (see DNA methylation in cancer). Sites of oxidative damage in chromatin can recruit complexes that contain DNA methyltransferases (DNMTs), a histone deacetylase (SIRT1), and a histone methyltransferase (EZH2), and thus induce DNA methylation.[42][51][52] DNA methylation of a CpG island in a promoter region may cause silencing of its downstream gene (see CpG site and regulation of transcription in cancer). DNA repair genes, in particular, are frequently inactivated by methylation in various cancers (see hypermethylation of DNA repair genes in cancer). A 2018 report[53] evaluated the relative importance of mutations and epigenetic alterations in progression to two different types of cancer. This report showed that epigenetic alterations were much more important than mutations in generating gastric cancers (associated with inflammation).[54] However, mutations and epigenetic alterations were of roughly equal importance in generating esophageal squamous cell cancers (associated with tobacco chemicals and acetaldehyde, a product of alcohol metabolism).
HIV and AIDS
It has long been recognized that infection with
Delineating how CD4 T cells are depleted and how chronic inflammation and immune activation are induced lies at the heart of understanding HIV pathogenesis—one of the top priorities for HIV research by the Office of AIDS Research, National Institutes of Health. Recent studies demonstrated that caspase-1-mediated pyroptosis, a highly inflammatory form of programmed cell death, drives CD4 T-cell depletion and inflammation by HIV.[63][64][65] These are the two signature events that propel HIV disease progression to AIDS. Pyroptosis appears to create a pathogenic vicious cycle in which dying CD4 T cells and other immune cells (including macrophages and neutrophils) release inflammatory signals that recruit more cells into the infected lymphoid tissues to die. The feed-forward nature of this inflammatory response produces chronic inflammation and tissue injury.[66] Identifying pyroptosis as the predominant mechanism that causes CD4 T-cell depletion and chronic inflammation, provides novel therapeutic opportunities, namely caspase-1 which controls the pyroptotic pathway. In this regard, pyroptosis of CD4 T cells and secretion of pro-inflammatory cytokines such as IL-1β and IL-18 can be blocked in HIV-infected human lymphoid tissues by addition of the caspase-1 inhibitor VX-765,[63] which has already proven to be safe and well tolerated in phase II human clinical trials.[67] These findings could propel development of an entirely new class of "anti-AIDS" therapies that act by targeting the host rather than the virus. Such agents would almost certainly be used in combination with ART. By promoting "tolerance" of the virus instead of suppressing its replication, VX-765 or related drugs may mimic the evolutionary solutions occurring in multiple monkey hosts (e.g. the sooty mangabey) infected with species-specific lentiviruses that have led to a lack of disease, no decline in CD4 T-cell counts, and no chronic inflammation.
Resolution
The inflammatory response must be actively terminated when no longer needed to prevent unnecessary "bystander" damage to tissues.[9] Failure to do so results in chronic inflammation, and cellular destruction. Resolution of inflammation occurs by different mechanisms in different tissues. Mechanisms that serve to terminate inflammation include:[9][68]
- Short inflammatory mediatorsin vivo.
- Production and release of
- Production and release of interleukin 10 (IL-10)[72]
- Production of anti-inflammatory
- Downregulation of pro-inflammatory molecules, such as leukotrienes.
- Upregulation of anti-inflammatory molecules such as the tumor necrosis factor receptor(TNFR)
- Apoptosis of pro-inflammatory cells[75]
- Desensitization of receptors.
- Increased survival of cells in regions of inflammation due to their interaction with the extracellular matrix (ECM)[76][77]
- Downregulation of receptor activity by high concentrations of ligands
- Cleavage of matrix metalloproteinases (MMPs) might lead to production of anti-inflammatory factors.[78]
Acute inflammation normally resolves by mechanisms that have remained somewhat elusive. Emerging evidence now suggests that an active, coordinated program of resolution initiates in the first few hours after an inflammatory response begins. After entering tissues,
cytokines such as transforming growth factor-β1. The anti-inflammatory program ends with the departure of macrophages through the lymphatics.[79]
Connection to depression
There is evidence for a link between inflammation and depression.[80] Inflammatory processes can be triggered by negative cognitions or their consequences, such as stress, violence, or deprivation. Thus, negative cognitions can cause inflammation that can, in turn, lead to depression.[81][82][dubious – discuss] In addition, there is increasing evidence that inflammation can cause depression because of the increase of cytokines, setting the brain into a "sickness mode".[83]
Classical symptoms of being physically sick, such as lethargy, show a large overlap in behaviors that characterize depression. Levels of cytokines tend to increase sharply during the depressive episodes of people with bipolar disorder and drop off during remission.[84] Furthermore, it has been shown in clinical trials that anti-inflammatory medicines taken in addition to antidepressants not only significantly improves symptoms but also increases the proportion of subjects positively responding to treatment.[85] Inflammations that lead to serious depression could be caused by common infections such as those caused by a virus, bacteria or even parasites.[86]
Connection to delirium
There is evidence for a link between inflammation and delirium based on the results of a recent longitudinal study investigating CRP in COVID-19 patients.[87]
Systemic effects
An
When inflammation overwhelms the host,
Acute-phase proteins
Inflammation also is characterized by high systemic levels of
- Fever
- Increased blood pressure
- Decreased sweating
- Malaise
- Loss of appetite
- Somnolence
Leukocyte numbers
Inflammation often affects the numbers of leukocytes present in the body:
- Leukopenia can be induced by certain infections and diseases, including viral infection, Rickettsia infection, some protozoa, tuberculosis, and some cancers.[9]
Interleukins and obesity
With the discovery of interleukins (IL), the concept of systemic inflammation developed. Although the processes involved are identical to tissue inflammation, systemic inflammation is not confined to a particular tissue but involves the endothelium and other organ systems.
Chronic inflammation is widely observed in obesity.[89][90] Obese people commonly have many elevated markers of inflammation, including:[91][92]
Low-grade chronic inflammation is characterized by a two- to threefold increase in the systemic concentrations of cytokines such as TNF-α, IL-6, and CRP.[95] Waist circumference correlates significantly with systemic inflammatory response.[96]
Loss of white adipose tissue reduces levels of inflammation markers.[89] As of 2017 the association of systemic inflammation with insulin resistance and type 2 diabetes, and with atherosclerosis was under preliminary research, although rigorous clinical trials had not been conducted to confirm such relationships.[97]
Outcomes
The outcome in a particular circumstance will be determined by the tissue in which the injury has occurred—and the injurious agent that is causing it. Here are the possible outcomes to inflammation:[9]
- Resolution
The complete restoration of the inflamed tissue back to a normal status. Inflammatory measures such as vasodilation, chemical production, and leukocyte infiltration cease, and damaged parenchymal cells regenerate. Such is usually the outcome when limited or short-lived inflammation has occurred. - scarring occurs in these areas of damage, forming a scar composed primarily of collagen. The scar will not contain any specialized structures, such as parenchymalcells, hence functional impairment may occur.
- Abscess formation
A cavity is formed containing pus, an opaque liquid containing dead white blood cells and bacteria with general debris from destroyed cells. - Chronic inflammation
In acute inflammation, if the injurious agent persists then chronic inflammation will ensue. This process, marked by inflammation lasting many days, months or even years, may lead to the formation of a chronic wound. Chronic inflammation is characterised by the dominating presence of macrophages in the injured tissue. These cells are powerful defensive agents of the body, but the toxins they release—including reactive oxygen species—are injurious to the organism's own tissues as well as invading agents. As a consequence, chronic inflammation is almost always accompanied by tissue destruction.
Examples
Inflammation is usually indicated by adding the suffix "
-
Acute appendicitis
-
Acute dermatitis
-
Acute infective meningitis
-
Acute tonsillitis
See also
Notes
- ^ All these signs may be observed in specific instances, but no single sign must, as a matter of course, be present.[13]
These are the original, or cardinal signs of inflammation.[13]
- ^ Functio laesa is an antiquated notion, as it is not unique to inflammation and is a characteristic of many disease states.[14]
References
- PMID 17223962.
- S2CID 3571245.
- ISBN 978-1-4160-4688-2.
- ^ "Inflammation and Your Health". Cedars-Sinai.
- from the original on 12 July 2021. Retrieved 1 July 2021.
- ^ ISBN 978-1-4160-4574-8.
- from the original on 21 January 2021. Retrieved 1 July 2017.
- S2CID 19823098.
- ^ ISBN 978-0-7216-7335-6.
- S2CID 16992741.
- ^ from the original on 15 June 2022. Retrieved 28 December 2020.
- ^ from the original on 19 December 2020. Retrieved 28 December 2020.
- ^ a b Stedman's Medical Dictionary (Twenty-fifth ed.). Williams & Wilkins. 1990.
- PMID 5276838.
- ^ from the original on 5 October 2008. Retrieved 5 November 2008.
- ^ PMID 5276838.
- ISBN 978-0-7817-6919-8. Archivedfrom the original on 21 December 2015. Retrieved 6 October 2010.
- ISBN 978-90-6299-220-1.
- ISBN 978-0-7817-7087-3.
- ISBN 978-0-300-11322-8.
- ^ InformedHealth.org [Internet]. Institute for Quality and Efficiency in Health Care (IQWiG). 22 February 2018 – via www.ncbi.nlm.nih.gov.
- ^ "Inflammation | Definition, Symptoms, Treatment, & Facts | Britannica". www.britannica.com. 11 March 2024.
- ^ Robbins S, Cotran R, Kumar V, Abbas A, Aster J (2020). Pathologic basis of disease (10th ed.). Philadelphia, PA: Saunders Elsevier.
- ^ PMID 25833893.
- PMID 29987840.
- ^ S2CID 205214291.
- PMID 36724330.
- ISBN 978-0-323-66162-1, retrieved 17 February 2023
- ^ ISBN 978-1-4441-8499-0.
- PMID 24830021.
- PMID 17498057.
- PMID 25958181.
- S2CID 407449.
- S2CID 3079540.
- S2CID 35240781.
- PMID 15006539.
- PMID 21914164.
- ^ PMID 12490959.
- PMID 22914051.
- S2CID 205469320.
- PMID 19468060.
- ^ (PDF) from the original on 29 August 2022. Retrieved 9 June 2018.
- (PDF) from the original on 30 October 2022. Retrieved 9 June 2018.
- PMID 6399978.
- ^ PMID 11866137.
- PMID 27989142.
- PMID 22293091.
- PMID 24281019.
- ^ PMID 31395351.
- PMID 28050219.
- PMID 22094255.
- PMID 28522752.
- PMID 29358395.
- S2CID 18727504.
- ^ PMID 21090961.
- PMID 23772629.
- PMID 9697722.
- PMID 23228847.
- PMID 24487059.
- PMID 21317533.
- PMID 9557672.
- PMID 22403383.
- ^ PMID 24356306.
- PMID 24356113.
- PMID 26321639.
- PMID 26962940.
- ^ "Study of VX-765 in Subjects With Treatment-resistant Partial Epilepsy – Full Text View – ClinicalTrials.gov". clinicaltrials.gov. 19 December 2013. Archived from the original on 26 September 2022. Retrieved 21 May 2016.
- PMID 17299434.
- S2CID 37216623.
- from the original on 10 January 2020. Retrieved 11 September 2019.
- PMID 10973958.
- PMID 10548513.
- PMID 18673006.
- PMID 25911383.
- PMID 9785465.
- S2CID 11765495.
- S2CID 7905603.
- PMID 10947989.
- S2CID 22379843.
- PMID 24228900.
- S2CID 1512121.
- PMID 26357876.
- ^ Williams C (4 January 2015). "Is depression a kind of allergic reaction?". The Guardian. Archived from the original on 21 October 2022. Retrieved 11 December 2016.
- PMID 19251324.
- PMID 16491133.
- PMID 25364500.
- from the original on 22 October 2021. Retrieved 20 February 2023.
- from the original on 11 May 2021. Retrieved 22 September 2021.
- ^ PMID 27012931.
- PMID 15181022.
- PMID 10999830.
- S2CID 73100391.
- ^ PMID 9438411.
- ^ PMID 12379575.
- S2CID 4776835.
- PMID 20659330.
- PMID 28045401.
- S2CID 206227739.
External links
- Inflammation at the U.S. National Library of Medicine Medical Subject Headings (MeSH)



