Synovial fluid
| Synovial fluid | |
|---|---|
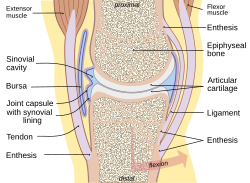 A typical joint | |
| Details | |
| Identifiers | |
| Latin | synovia |
| MeSH | D013582 |
| TA98 | A03.0.00.031 |
| TA2 | 1535 |
| FMA | 12277 |
| Anatomical terminology | |
Synovial fluid, also called synovia,
Structure
The inner membrane of synovial joints is called the synovial membrane and secretes synovial fluid into the joint cavity.[3] Synovial fluid is an ultrafiltrate from plasma, and contains proteins derived from the blood plasma and proteins that are
produced by cells within the joint tissues.
- reduction of friction — synovial fluid lubricates the articulating joints[7][page needed]
- shock absorption — as a rheopectic properties,[8] becoming more viscous under applied pressure; the synovial fluid in diarthrotic joints becomes thick the moment shear is applied in order to protect the joint and subsequently, thins to normal viscosity instantaneously to resume its lubricating function between shocks.[9] [dubious]
- nutrient and waste transportation — the fluid supplies oxygen and nutrients and removes carbon dioxide and metabolic wastes from the chondrocytes in the surrounding cartilage
- molecular sieving - pressure within the joint forces hyaluronan.[10]
Composition
Synovial tissue is sterile and composed of vascularized connective tissue that lacks a basement membrane. Two cell types (type A and type B) are present: Type A is derived from blood monocytes, and it removes the wear-and-tear debris from the synovial fluid. Type B produces
Synovial fluid contains
It also contains phagocytic cells that remove microbes and the debris that results from normal wear and tear in the joint.
Clinical significance
Collection
Synovial fluid may be collected by syringe in a procedure termed arthrocentesis, also known as joint aspiration.
Classification
Synovial fluid may be classified into normal, noninflammatory, inflammatory, septic, and hemorrhagic:
| Normal | Non-inflammatory | Inflammatory | Septic | Bleeding | |
| Volume (ml) | <3.5 | >3.5 | >3.5 | >3.5 | >3.5 |
| Viscosity | High | High | Low | Mixed | Low |
| Clarity | Clear | Clear | Cloudy | Opaque | Mixed |
| Color | Colorless/straw | Straw/yellow | Yellow | Mixed | Red |
| WBC/mm3 | <200 | <2,000[17] | 5,000[17]-75,000 | >50,000[17] | Similar to blood level |
Polys (%) |
<25 | <25[17] | 50[17]-70[17] | >70[17] | Similar to blood level |
| Gram stain | None | None | None | + (S aureus & Streptococcus) - (Neisseria gonorrhoeae) | None |
Glucose (mg/dl) concentration in synovial fluid is nearly equal to serum.
- Synovial fluid viscosity
Normal:
- Normal
- Traumatic arthritis
- Degenerative (Osteo) arthritis
- Pigmented villonodular synovitis
Normal or decreased:
- Systemic lupus erythematosus
Decreased:
- Rheumatic fever
- Rheumatoid arthritis
- Gout
- Pyogenic (Septic) arthritis
- Tubercular arthritis
- Less of lubrication in joints
Pathology

Many synovial fluid types are associated with specific diagnoses:[18][19]
- Noninflammatory (Group I)
- degenerative joint disease
- Trauma
- Rheumatic fever
- Chronic pseudogout
- Scleroderma
- Polymyositis
- Systemic lupus erythematosus
- Erythema nodosum
- Neuropathic arthropathy (with possible hemorrhage)
- Sickle-cell disease
- Hemochromatosis
- Acromegaly
- Amyloidosis
- Inflammatory (Group II)
- Rheumatoid arthritis
- Reactive arthritis
- Psoriatic arthritis
- Acute rheumatic fever
- Acute gout or pseudogout
- Scleroderma
- Polymyositis
- Systemic lupus erythematosus
- Ankylosing spondylitis
- Inflammatory bowel disease arthritis
- Infection (viral, fungal, bacterial) including Lyme disease
- Acute crystal synovitis(gout)
- Septic (Group III)
- Pyogenic bacterial infection
- Septic arthritis
- Hemorrhagic
- Trauma
- Tumors
- Hemophilia/coagulopathy
- Scurvy
- Ehlers-Danlos syndrome
- Neuropathic arthropathy
Analysis
Glucose (mg/dl) concentration in synovial fluid is nearly equal to serum.
The cytological and biochemical analysis of human synovial fluid began around 1940 using cadaver-derived fluid and comparing characteristics to those of, for instance, bovine synovial fluid.[20]
Chemistry
The mucin clot test is a very old approach to determining if an inflammatory infiltrate is present. In this test, acetic acid is added to the synovial fluid specimen. In a normal specimen, this should lead to a congealing of the hyaluronic acid, forming a 'mucin clot.' If inflammation is present, a mucin clot is not formed (the hyaluronic acid is degraded).[21]
Lactate is elevated in septic arthritis, usually above 250 mg/dL.
Complement factors are decreased in rheumatoid arthritis and lupus arthritis.
Microscopy
Microscopic analysis of synovial fluid is performed to evaluate for cell count and crystals. Crystals include
Monosodium urate crystals are seen in
Hydroxyapatite crystals are small and negatively birefringent. They are usually only detectable with an Alizarin Red S stain.
Corticosteroid crystals may be seen following therapeutic corticosteroid injection into the joint space. They appear blunt, jagged, and show variable birefringence.[21]
Cracking joints
When the two articulating surfaces of a synovial joint are separated from one other, the volume within the joint capsule is increased and a negative pressure results. The volume of synovial fluid within the joint is insufficient to fill the expanding volume of the joint and gases dissolved in the synovial fluid (mostly carbon dioxide) are liberated and quickly fill the empty space, leading to the rapid formation of a bubble.[22] This process is known as cavitation. Cavitation in synovial joints results in a high frequency 'cracking' sound.[23][24]
Etymology and pronunciation
The term synovia (/sɪˈnoʊviə/) came to English around 1640 (the anglicized form synovial is first recorded in the mid 18th century) from Neo-Latin, where it was coined perhaps by Paracelsus from Greek συν- "with" and Latin ovum "egg" and -ia because it resembles egg white in consistency and external appearance.[25][26][27][28][29]
The term synovium is a much more recent pseudo-Latin coinage for what is less confusingly called the synovial membrane. It is not recorded in general dictionaries, and medical dictionaries only explain its meaning, not its etymology, but it is apparently derived from the term synovia, i.e. the obfuscated etymology of mixed Greek and Latin elements of the singular term synovia was misunderstood and the word was erroneously reinterpreted as the plural of the previously non-existent term synovium (perhaps in analogy to other plural terms for liquids such as "waters" for amniotic fluid). If one insists on using this pseudo-Latin term synovium for the synovial membrane, the non-Latinate plural synoviums is better and less confusing than synovia.
References
- OCLC 908716294.
- ISBN 978-0-323-24145-8, retrieved 2020-10-18
- ISBN 978-0-12-809847-9, retrieved 2020-10-18
- PMID 25160569.
- PMID 25172828.
- ^ Edwards, Jo, ed. (2000). "Normal Joint Structure". Notes on Rheumatology. University College London. Archived from the original on 19 November 2012. Retrieved 5 April 2013.
- OCLC 850877694.
- PMID 24989639.
- ^ "Synovial fluid - OrthopaedicsOne Articles - OrthopaedicsOne". Retrieved 20 September 2016.
- PMID 15961430.
- PMID 16849228.
- PMID 21826801.
- ^ Hascall, Vincent C.; Laurent, Torvard C. (15 December 1997). "GlycoForum / Science of Hyaluronan". Glycoforum. 1: A2.
- ^ "Joints". University of Washington Medicine - Department of Orthopaedics and Sports Medicine. Archived from the original on 2013-08-07. Retrieved 2013-02-04.
- PMID 10743795.
- PMC 2833794.
- ^ ISBN 978-0-7817-7153-5.
- ^ "Lupus Anticoagulant". Family Practice Notebook. Archived from the original on 18 January 2013. Retrieved 7 April 2013.
- ^ American College of Rheumatology Archived September 5, 2004, at the Wayback Machine
- PMID 16694795and references therein
- ^ OCLC 692198047[pages needed]
- PMID 5557778.
- ^ Watson P, Kernoham WG, Mollan RAB. A study of the cracking sounds from the metacarpophalangeal joint. Proceedings of the Institute of Mechanical Engineering [H] 1989;203:109-118.
- ^ "What makes your knuckles pop?". 3 August 2000. Retrieved 20 September 2016.
- ^ "synovia" in the Collins Concise English Dictionary
- ^ "synovia" in the Random House Unabridged Dictionary
- ^ "synovia" in the American Heritage Dictionary
- ^ "synovial" in the Oxford Dictionaries Online
- ^ "synovia" in the Great Soviet Encyclopedia
Further reading
- Warman, M. (2003). "Delineating biologic pathways involved in skeletal growth and homeostasis through the study of rare Mendelian diseases that affect bones and joints". Arthritis Research & Therapy. 5: 5. PMC 2833794.
