Analeptic

An analeptic, in
Medical use

Analeptics have been used throughout history for two main purposes, to help patients recover from anesthesia more efficiently and to manage respiratory distress and apnea, particularly in infants.
Anesthesia recovery
Analeptics can be used to increase the speed of recovery from propofol, remifentanil, and sevoflurane. In clinical settings, analeptics such as doxapram have been used to help patients recover from anesthesia better, as well as to remove some of the potential negative side effects of potent anesthetics.
Respiratory distress management
The three most prevalent clinical analeptic uses of caffeine are in the treatment of
Ample research also suggests that caffeine significantly reduces the occurrence of bronchopulmonary dysplasia, which is a chronic lung disorder defined by the need for supplemental oxygen after a postmenstrual age of 36 weeks.[6] Bronchopulmonary dysplasia is common in infants with low birth weight (<2500 g) and very low birth weight (<1500 g) who received mechanical ventilator machines to help manage respiratory distress syndrome. Currently, no treatment is known for bronchopulmonary dysplasia, as the risks of treatment are generally thought to outweigh the necessity for using a mechanical ventilator. Caffeine only reduces occurrence.
Theophylline is no longer used as a respiratory analeptic in newborn infants. Theophylline has a very narrow therapeutic index, so its dosages must be supervised by direct measurement of serum theophylline levels to avoid toxicity.
Mechanism of action
Analeptics are a diverse group of medications that work through a variety of chemical pathways; analeptic medications work through four main mechanisms to stimulate respiration. Analeptics can act as
Two common potassium channel blockers are doxapram and
The third common mechanism of which analeptics take advantage is to act as serotonin receptor agonists.
With respect to breathing, caffeine acts as a competitive
Doxapram
Doxapram is an
Methylxanthines caffeine and theophylline

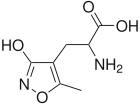
The naturally occurring compounds
History
After their introduction in the early 20th century, analeptics were used to study the new life-threatening problem of barbiturate overdose. Prior to the 1930s, naturally occurring stimulants such as camphor and caffeine were used in the treatment of barbiturate overdose.[10] Between 1930 and 1960, synthetic analeptics such as nikethamide, pentylenetetrazol, bemegride, amphetamine, and methylphenidate replaced the naturally occurring compounds in treating barbiturate overdose. Recently, analeptics have been turned to the treatment of ADHD due to more efficient ways to treat barbiturate overdoses.[11]
One of the first widely used analeptics was
Doxapram use is declining in humans, though it is an effective CNS and respiratory stimulant, primarily because of shorter-lasting
