Autoregulation
Autoregulation is a process within many biological systems, resulting from an internal adaptive mechanism that works to adjust (or mitigate) that system's response to stimuli. While most systems of the body show some degree of autoregulation, it is most clearly observed in the kidney, the heart, and the brain.[1] Perfusion of these organs is essential for life, and through autoregulation the body can divert blood (and thus, oxygen) where it is most needed.
Cerebral autoregulation
More so than most other organs, the brain is very sensitive to increased or decreased blood flow, and several mechanisms (metabolic, myogenic, and neurogenic) are involved in maintaining an appropriate cerebral blood pressure. Brain blood flow autoregulation is abolished in several disease states such as traumatic brain injury,[2] stroke,[3] brain tumors, or persistent abnormally high CO2 levels.[4][5]
Homeometrics and heterometric autoregulation of the heart
Homeometric autoregulation, in the context of the circulatory system, is the heart's ability to increase contractility and restore stroke volume when afterload increases.[6] Homeometric autoregulation occurs independently of cardiomyocyte fiber length, via the Bowditch and/or Anrep effects.[7]
- Via the Bowditch effect, positive inotropy occurs secondary to an increased cardiac frequency. The exact mechanism for this remains unknown, but it appears to be the result of an increased exposure of the heart to contractile substances arising from the increased flow caused by an increased cardiac frequency.[7]
- Via the Anrep effect, positive inotropy occurs secondary to increased ventricular pressure.[7]
This is in contrast to
Coronary circulatory autoregulation
Since the heart is a very aerobic organ, needing oxygen for the efficient production of ATP & Creatine Phosphate from fatty acids (and to a smaller extent, glucose & very little lactate), the coronary circulation is auto regulated so that the heart receives the right flow of blood & hence sufficient supply of oxygen. If a sufficient flow of oxygen is met and the resistance in the coronary circulation rises (perhaps due to vasoconstriction), then the coronary perfusion pressure (CPP) increases proportionally, to maintain the same flow. In this way, the same flow through the coronary circulation is maintained over a range of pressures. This part of coronary circulatory regulation is known as auto regulation and it occurs over a plateau, reflecting the constant blood flow at varying CPP & resistance. The slope of a CBF (coronary blood flow) vs. CPP graph gives 1/Resistance. Autoregulation maintains a normal blood flow within the pressure range of 70–110 mm Hg. Blood flow is independent of bp. However autoregulation of blood flow in the heart is not so well developed like that in brain.
Renal autoregulation
Regulation of renal blood flow is important to maintaining a stable glomerular filtration rate (GFR) despite changes in systemic blood pressure (within about 80-180 mmHg). In a mechanism called
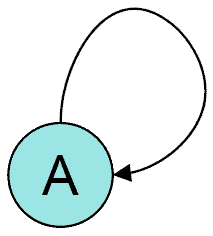
Autoregulation of genes

This is so-called "steady-state system". An example is a system in which a protein P that is a product of gene G "positively regulates its own production by binding to a regulatory element of the gene coding for it,"[11] and the protein gets used or lost at a rate that increases as its concentration increases. This feedback loop creates two possible states "on" and "off". If an outside factor makes the concentration of P increase to some threshold level, the production of protein P is "on", i.e. P will maintain its own concentration at a certain level, until some other stimulus will lower it down below the threshold level, when concentration of P will be insufficient to make gene G express at the rate that would overcome the loss or use of the protein P. This state ("on" or "off") gets inherited after cell division, since the concentration of protein a usually remains the same after mitosis. However, the state can be easily disrupted by outside factors. [11]
Similarly, this phenomenon is not only restricted to genes but may also apply to other genetic units, including mRNA transcripts. Regulatory segments of mRNA called a
See also
References
- ^ "CV Physiology | Autoregulation of Organ Blood Flow". www.cvphysiology.com. Retrieved 2020-07-12.
- PMID 19877773.
- S2CID 23424407.
- PMID 2201348.
- PMID 10475580.
- S2CID 14858415.
- ^ ISBN 9780470720066.
- ISBN 9781455770052.
- PMID 19330465.
- ^ PMID 15283759.
- ^ a b Jablonka E.; Lachmann M.; Lamb M.J. (1992). "Evidence, Mechanisms and Models for the Inheritance of Acquired Characters". Journal of Theoretical Biology. 158 (2): 245–268. .
- PMID 23283231.
