Lipoprotein(a)
| LPA | |||
|---|---|---|---|
Gene ontology | |||
| Molecular function | |||
| Cellular component | |||
| Biological process | |||
| Sources:Amigo / QuickGO | |||
Ensembl |
| ||||||||
|---|---|---|---|---|---|---|---|---|---|
| UniProt |
| ||||||||
| RefSeq (mRNA) |
| ||||||||
| RefSeq (protein) |
|
| |||||||
| Location (UCSC) | Chr 6: 160.53 – 160.66 Mb | n/a | |||||||
| PubMed search | [2] | n/a | |||||||
| View/Edit Human | |||
Lipoprotein(a) is a
Lipoprotein(a) was discovered in 1963 by Kåre Berg.[7] The human gene encoding apolipoprotein(a) was successfully cloned in 1987.[8]
Structure
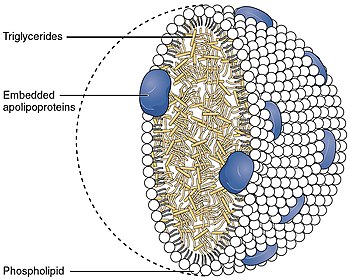
Lipoprotein(a) [Lp(a)] consists of an
There is a general inverse correlation between the size of the apo(a) isoform and the Lp(a) plasma concentration.
Populations
This section needs additional citations for verification. (October 2015) |
Lp(a) concentrations can vary by more than one thousand between individuals, from <0.2 to >200 mg/dL. This range of concentrations is observed in all populations studied by scientists so far. The mean and median concentrations differ among world populations. Most prominently, there is a two- to threefold higher mean Lp(a) plasma concentration in populations of African descent compared to Asian, Oceanic, or European populations. The general inverse correlation between apo(a) isoform size and Lp(a) plasma concentration is observed in all populations.[10] However, it was also discovered that mean Lp(a) associated with certain apo(a) isoforms varies between populations.
In addition to size effects, mutations in the LPA promoter may lead to a decreased apo(a) production.[13]
Function and pathology
Lp(a) is assembled at the hepatocyte cell membrane surface, which is similar to typical LDL particles. However, there are other possible locations of assembly. The particles mainly exist in plasma.[14][15][16][17]
Lp(a) contributes to the process of
Moreover, Lp(a) carries atherosclerosis-causing cholesterol and binds atherogenic pro-inflammatory oxidised phospholipids as a preferential carrier of oxidised phospholipids in human plasma,[22] which attracts inflammatory cells to vessel walls and leads to smooth muscle cell proliferation.[23][24][25] Moreover, Lp(a) also is hypothesised to be involved in wound healing and tissue repair by interacting with components of the vascular wall and extracellular matrix.[26][27] Apo(a), a distinct feature of the Lp(a) particle, binds to immobilized fibronectin and endows Lp(a) with the serine-proteinase-type proteolytic activity.[28]
Nonetheless, individuals without Lp(a) or with very low Lp(a) levels seem to be healthy.[
Another possibility, suggested by
Catabolism and clearance
The half-life of Lp(a) in circulation is approximately three to four days.[15] The mechanism and sites of Lp(a) catabolism are largely unknown. Uptake via the LDL receptor is not a major pathway of Lp(a) metabolism.[30][31] The kidney has been identified as playing a role in Lp(a) clearance from plasma.[32]
Disease
High Lp(a) in blood correlates with
Most commonly prescribed lipid-reducing drugs have little or no effect on Lp(a) concentration. Results using statin medications have been mixed in most trials, although a meta-analysis published in 2012 suggests that atorvastatin may be of benefit.[34]
High Lp(a) correlates with early atherosclerosis independently of other cardiac risk factors, including LDL. In patients with advanced cardiovascular disease, Lp(a) indicates a coagulant risk of plaque thrombosis. Apo(a) contains domains that are very similar to plasminogen (PLG). Lp(a) accumulates in the vessel wall and inhibits the binding of PLG to the cell surface, reducing plasmin generation, which increases clotting. This inhibition of PLG by Lp(a) also promotes the proliferation of smooth muscle cells. These unique features of Lp(a) suggest that Lp(a) causes generation of clots and atherosclerosis.[37]
In one homogeneous tribal population of Tanzania, vegetarians have higher levels of Lp(a) than fish eaters, raising the possibility that pharmacologic amounts of fish oil supplements may help lower the levels of Lp(a).[38] Researchers in studies in 1995 and 1998 concluded that regular consumption of moderate amounts of alcohol led to a significant decline in plasma levels of Lp(a).[39] Other studies did not report this.
Diagnostic testing
Numerous studies confirming a strong correlation between elevated Lp(a) and heart disease have led to the consensus that Lp(a) is an important independent predictor of cardiovascular disease.[3] Animal studies have shown that Lp(a) may directly contribute to atherosclerotic damage by increasing plaque size, inflammation, instability, and smooth muscle cell growth.[40] Genetic data also support the theory that Lp(a) causes cardiovascular disease.[4]
The European Atherosclerosis Society currently recommends that patients with a moderate or high risk of cardiovascular disease should have their Lp(a) levels checked. Any patient with one of the following risk factors should be screened:
- premature cardiovascular disease
- familial hypercholesterolaemia
- family history of premature cardiovascular disease
- family history of elevated Lp(a)
- recurrent cardiovascular disease despite statin treatment
- ≥3% ten-year risk of fatal cardiovascular disease according to the European guidelines
- ≥10% ten-year risk of fatal and/or non-fatal cardiovascular disease according to the U.S. guidelines[3]
If the level is elevated, treatment should be initiated to bring the level below 50 mg/dL. In addition, the patient's other cardiovascular risk factors (including LDL levels) should be managed optimally.[3] Apart from the total Lp(a) plasma concentration, the apo(a) isoform might be an important risk parameter as well.[41][42]
Prior studies of the relationship between Lp(a) and ethnicity have shown inconsistent results. Lp(a) levels seem to differ in different populations. For example, in some African populations, Lp(a) levels are higher on average than in other groups, so that using a risk threshold of 30 mg/dl could classify over 50% of the individuals as higher risk.[43][44][45][46] Some part of this complexity may be related to the different genetic factors involved in determining Lp(a) levels. One recent study showed that in different ethnic groups, different genetic alterations were associated with increased Lp(a) levels.[47]
More recent data suggest that prior studies were underpowered. The Atherosclerosis Risk in Communities (ARIC) Study followed 3467 African Americans and 9851 whites for 20 years. The researchers found that an elevated Lp(a) conferred the same risk in each group. African Americans had roughly three times the level of Lp(a), however, and Lp(a) also predicted an increased risk of stroke.[48]
Approximate levels of risk are indicated by the results below, although at present there are a variety of different methods by which to measure Lp(a). A standardized international reference material has been developed and is accepted by the WHO Expert Committee on Biological Standardization and the International Federation of Clinical Chemistry and Laboratory Medicine. Although further standardization is still needed, development of a reference material is an importance step toward standardizing results.[49][50]
Lipoprotein(a) - Lp(a)[51]
- Desirable: <14 mg/dL (<35 nmol/L)
- Borderline risk: 14–30 mg/dL (35–75 nmol/L)
- High risk: 31–50 mg/dL (75–125 nmol/L)
- Very high risk: >50 mg/dL (>125 nmol/L)
Lp(a) appears with different isoforms (per kringle repeats) of apolipoprotein; 40% of the variation in Lp(a) levels when measured in mg/dl can be attributed to different isoforms. Lighter Lp(a) are also associated with disease. Thus, a test with simple quantitative results may not provide a complete assessment of risk.[52]
Treatment
The current simplest treatment for elevated Lp(a) is to take 1–3 grams of
A meta-analysis suggested that atorvastatin may lower Lp(a) levels.[34] In severe cases, such as familial hypercholesterolemia or treatment-resistant hypercholesterolemia, LDL apheresis may dramatically reduce Lp(a). The goal of the treatment is to reduce levels to below 50 mg/dL. Cost is prohibitively high.[3]
A meta-analysis of six clinical trials confirmed that flaxseed supplementation modestly lowers Lp(a) levels.[54]
Testosterone is known to reduce Lp(a) levels.[55] Testosterone replacement therapy also appears to be associated with lower Lp(a) levels.[56][57] Estrogen replacement therapy in post-menopausal women will reduce Lp(a).[58] Raloxifene has not been shown to reduce Lp(a), while tamoxifen has.[59]
L-carnitine may also reduce Lp(a) levels. A systematic review and meta-analysis found a significant reduction with oral but not intravenous carnitine.[60] Other medications that are in various stages of development include thyromimetics, cholesterol-ester-transfer protein (CETP inhibitors), anti-sense oligonucleopeptides (such as Pelacarsen and Olpasiran), and proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors.[61][62]
The American Academy of Pediatrics now recommends that all children between the ages of nine and eleven years old be screened for hyperlipidemia. Lp(a) levels should be considered in particular in children with a family history of early heart disease or high blood cholesterol levels. However, there have not been enough studies to determine which therapies might be beneficial.[63]
Interactions
Lp(a) has been shown to
See also
- Lipoprotein
- Apolipoprotein
- Very-low-density lipoprotein
- Combined hyperlipidemia
References
- ^ a b c GRCh38: Ensembl release 89: ENSG00000198670 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ PMID 20965889.
- ^ S2CID 23045050.
- PMID 17478739.
- PMID 36708412.
- PMID 14064818.
- ^ S2CID 4344313.
- PMID 2956279.
- ^ S2CID 19657929.
- PMID 9548923.
- PMID 8943305.
- ^ PMID 10720444.
- PMID 7961823.
- ^ PMID 8432853.
- PMID 10431664.
- S2CID 45103589.
- PMID 25819754.
- PMID 20965889.
- PMID 25778403.
- S2CID 1212821.
- PMID 16000355.
- PMID 27108250.
- PMID 21529331.
- S2CID 24081304.
- S2CID 4322332.
- PMID 2146124.
- ^ PMID 2531657.
- S2CID 37023416.
- PMID 1830206.
- PMID 7883987.
- PMID 17495935.
- ISBN 978-0-9724959-0-5.
- ^ PMID 21996415.
- PMID 27733255.
- PMID 25936305.
- PMID 11698280.
- PMID 10323776.
- PMID 9603764.
- PMID 20477514.
- PMID 9247362.
- S2CID 12507462.
- PMID 1840066.
- S2CID 2188933.
- PMID 16267501.
- S2CID 44679184.
- PMID 21305047.
- PMID 22128224.
- PMID 11106328.
- S2CID 24696473.
- ISBN 978-0-312-34863-2.
- S2CID 912295.
- S2CID 5134822.
- PMID 31634874.
- PMID 8651107.
- PMID 8651107.
- PMID 21476974.)
{{cite journal}}: CS1 maint: DOI inactive as of April 2024 (link - PMID 28364865.
- PMID 28573436.
- PMID 26754058.
- PMID 21476974.)
{{cite journal}}: CS1 maint: DOI inactive as of April 2024 (link - PMID 36761062.
- PMID 22084329.
- PMID 9717723.
- PMID 12562843.
- PMID 10980194.
External links
- Lipoprotein(a) at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- Overview of all the structural information available in the PDB for UniProt: P08519 (Apolipoprotein(a)) at the PDBe-KB.