Lipoprotein lipase
Ensembl | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| UniProt | |||||||||
| RefSeq (mRNA) | |||||||||
| RefSeq (protein) | |||||||||
| Location (UCSC) | Chr 8: 19.9 – 19.97 Mb | Chr 8: 69.33 – 69.36 Mb | |||||||
| PubMed search | [3] | [4] | |||||||
| View/Edit Human | View/Edit Mouse |
| Lipoprotein lipase | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Identifiers | |||||||||
ExPASy | NiceZyme view | ||||||||
| KEGG | KEGG entry | ||||||||
| MetaCyc | metabolic pathway | ||||||||
| PRIAM | profile | ||||||||
| PDB structures | RCSB PDB PDBe PDBsum | ||||||||
| Gene Ontology | AmiGO / QuickGO | ||||||||
| |||||||||
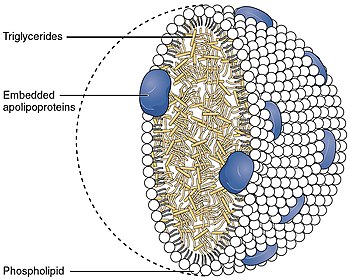
Lipoprotein lipase (LPL) (EC 3.1.1.34, systematic name triacylglycerol acylhydrolase (lipoprotein-dependent)) is a member of the
- triacylglycerol + H2O = diacylglycerol + a carboxylate
It is also involved in promoting the cellular uptake of
LPL is attached to the luminal surface of
Synthesis
In brief, LPL is secreted from heart, muscle and adipose
Homodimerization is required before LPL can be secreted from cells.[16][17] After secretion, LPL is carried across endothelial cells and presented into the capillary lumen by the protein glycosylphosphatidylinositol-anchored high-density lipoprotein-binding protein 1.[18][19]
Structure
Mechanism

The active site of LPL is composed of the conserved Ser-132, Asp-156, and His-241 triad. Other important regions of the N-terminal domain for catalysis includes an
The LPL non-covalent homodimer has a head-to-tail arrangement of the monomers. The Ser/Asp/His triad is in a hydrophobic groove that is blocked from solvent by the lid.[5][11] Upon binding to ApoC-II and lipid in the lipoprotein, the C-terminal domain presents the lipid substrate to the lid region. The lipid interacts with both the lid region and the hydrophobic groove at the active site; this causes the lid to move, providing access to the active site. The β5 loop folds back into the protein core, bringing one of the electrophiles of the oxyanion hole into position for lipolysis.[5] The glycerol backbone of the lipid is then able to enter the active site and is hydrolyzed.
Two molecules of ApoC-II can attach to each LPL dimer.
Function
LPL gene encodes lipoprotein lipase, which is expressed in the heart, muscle, and adipose tissue.[26][27] LPL functions as a homodimer, and has the dual functions of triglyceride hydrolase and ligand/bridging factor for receptor-mediated lipoprotein uptake. Through catalysis, VLDL is converted to IDL and then to LDL. Severe mutations that cause LPL deficiency result in type I hyperlipoproteinemia, while less extreme mutations in LPL are linked to many disorders of lipoprotein metabolism.[28]
Regulation
LPL is controlled transcriptionally and posttranscriptionally.[29] The circadian clock may be important in the control of Lpl mRNA levels in peripheral tissues.[30]
LPL
Consistent with this, dietary macronutrients differentially affect adipose and muscle LPL activity. After 16 days on a high-carbohydrate or a high-fat diet, LPL activity increased significantly in both tissues 6 hours after a meal of either composition, but there was a significantly greater rise in adipose tissue LPL in response to the high-carbohydrate diet compared to the high-fat diet. There was no difference between the two diets' effects on insulin sensitivity or fasting LPL activity in either tissue.[32]
The concentration of LPL displayed on endothelial cell surface cannot be regulated by endothelial cells, as they neither synthesize nor degrade LPL. Instead, this regulation occurs by managing the flux of LPL arriving at the lipolytic site and by regulating the activity of LPL present on the endothelium. A key protein involved in controlling the activity of LPL is ANGPTL4, which serves as a local inhibitor of LPL. Induction of ANGPTL4 accounts for the inhibition of LPL activity in white adipose tissue during fasting. Growing evidence implicates ANGPTL4 in the physiological regulation of LPL activity in a variety of tissues.[33]
An ANGPTL3-4-8 model was proposed to explain the variations of LPL activity during the fed-fast cycle.[34] Specifically, feeding induces ANGPTL8, activating the ANGPTL8–ANGPTL3 pathway, which inhibits LPL in cardiac and skeletal muscles, thereby making circulating triglycerides available for uptake by white adipose tissue, in which LPL activity is elevated owing to diminished ANGPTL4; the reverse is true during fasting, which suppresses ANGPTL8 but induces ANGPTL4, thereby directing triglycerides to muscles. The model suggests a general framework for how triglyceride trafficking is regulated.[34]
Clinical significance
Lipoprotein lipase deficiency leads to hypertriglyceridemia (elevated levels of triglycerides in the bloodstream).[35] In mice, overexpression of LPL has been shown to cause insulin resistance,[36][37] and to promote obesity.[30]
A high adipose tissue LPL response to a high-carbohydrate diet may predispose toward fat gain. One study reported that subjects gained more body fat over the next four years if, after following a high-carbohydrate diet and partaking of a high-carbohydrate meal, they responded with an increase in adipose tissue LPL activity per adipocyte, or a decrease in skeletal muscle LPL activity per gram of tissue.[38]
LPL expression has been shown to be a prognostic predictor in Chronic lymphocytic leukemia.[39] In this haematological disorder, LPL appears to provide fatty acids as an energy source to malignant cells.[40] Thus, elevated levels of LPL mRNA or protein are considered to be indicators of poor prognosis.[41][42][43][44][45][46][47][48][49][50]
Interactions
Lipoprotein lipase has been shown to
In other organisms
The LPL gene is highly conserved across vertebrates. Lipoprotein lipase is involved in lipid transport in the placentae of live bearing lizards (Pseudemoia entrecasteauxii).[54]
Interactive pathway map
Click on genes, proteins and metabolites below to link to respective articles. [§ 1]
- ^ The interactive pathway map can be edited at WikiPathways: "Statin_Pathway_WP430".
References
- ^ a b c GRCh38: Ensembl release 89: ENSG00000175445 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000015568 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ S2CID 40089672.
- PMID 9684736.
- PMID 7868983.
- PMID 16314153.
- PMID 270715.
- PMID 26289657.
- ^ PMID 1730040.
- PMID 12091482.
- ^ PMID 1445192.
- PMID 2521859.
- ^ PMID 8144612.
- ^ PMID 2753912.
- PMID 2644281.
- PMID 17403372.
- PMID 20620994.
- PMID 30559189.
- PMID 31072929.
- PMID 10777674.
- ^ PMID 8663292.
- PMID 1656440.
- PMID 12682050.
- ^ Protein Atlas, Protein Atlas. "Tissue expression of LPL - Summary - The Human Protein Atlas". www.proteinatlas.org. The Human Protein Atlas. Retrieved 25 July 2019.
- ^ Gene Cards, Gene Cards. "Human Gene Database". www.genecards.org. GeneCardsSuite. Retrieved 25 July 2019.
- ^ "Entrez Gene: LPL lipoprotein lipase".
- PMID 19318514.
- ^ S2CID 31204290.
- PMID 2677048.
- PMID 9701186.
- S2CID 10273285.
- ^ PMID 27053679.
- PMID 17706445.
- PMID 11334409.
- PMID 11390966.
- S2CID 40167321.
- PMID 29206143.
- PMID 26643954.
- PMID 15802535.
- PMID 15858619.
- PMID 16434371.
- S2CID 20532204.
- PMID 19709746.
- PMID 21508119.
- PMID 23478142.
- S2CID 22647616.
- PMID 29953583.
- PMID 27504855.
- PMID 7510694.
- PMID 7989348.
- PMID 1281473.
- PMID 23939756.
Further reading
- Zechner R (1997). "The tissue-specific expression of lipoprotein lipase: implications for energy and lipoprotein metabolism". Curr. Opin. Lipidol. 8 (2): 77–88. PMID 9183545.
- Fisher RM, Humphries SE, Talmud PJ (1998). "Common variation in the lipoprotein lipase gene: effects on plasma lipids and risk of atherosclerosis". Atherosclerosis. 135 (2): 145–59. PMID 9430364.
- Beisiegel U (1998). "Lipoprotein metabolism". Eur. Heart J. 19 Suppl A: A20–3. PMID 9519338.
- Pentikäinen MO, Oksjoki R, Oörni K, Kovanen PT (2002). "Lipoprotein lipase in the arterial wall: linking LDL to the arterial extracellular matrix and much more". Arterioscler. Thromb. Vasc. Biol. 22 (2): 211–7. PMID 11834518.
- Lichtenstein L, Berbée JF, van Dijk SJ, van Dijk KW, Bensadoun A, Kema IP, Voshol PJ, Müller M, Rensen PC, Kersten S (November 2007). "Angptl4 upregulates cholesterol synthesis in liver via inhibition of LPL- and HL-dependent hepatic cholesterol uptake". Arterioscler. Thromb. Vasc. Biol. 27 (11): 2420–7. PMID 17761937.
- Lichtenstein L, Mattijssen F, de Wit NJ, Georgiadi A, Hooiveld GJ, van der Meer R, He Y, Qi L, Köster A, Tamsma JT, Tan NS, Müller M, Kersten S (December 2010). "Angptl4 protects against severe proinflammatory effects of saturated fat by inhibiting fatty acid uptake into mesenteric lymph node macrophages". Cell Metab. 12 (6): 580–92. PMID 21109191.
External links
- GeneReviews/NCBI/NIH/UW entry on Familial Lipoprotein Lipase Deficiency
- Gene therapy for lipoprotein lipase deficiency
- Lipoprotein+lipase at the U.S. National Library of Medicine Medical Subject Headings (MeSH)