Cryptococcus neoformans
| Cryptococcus neoformans | |
|---|---|

| |
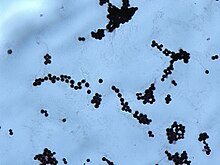
| Yeast state of Cryptococcus neoformans | |
| Scientific classification | |
| Domain: | Eukaryota |
| Kingdom: | Fungi |
| Division: | Basidiomycota |
| Class: | Tremellomycetes |
| Order: | Tremellales |
| Family: | Cryptococcaceae |
| Genus: | Cryptococcus |
| Species: | C. neoformans
|
| Binomial name | |
| Cryptococcus neoformans (San Felice) Vuill. (1901)
| |
| Synonyms | |
|
Saccharomyces neoformans San Felice (1895) | |
Cryptococcus neoformans is an encapsulated
Classification
Cryptococcus neoformans has undergone numerous nomenclature revisions since its first description in 1895. It formerly contained two
The teleomorph was first described in 1975 by K.J. Kwon-Chung, who obtained cultures of Filobasidiella neoformans by crossing strains of the yeast C. neoformans. She was able to observe
Characteristics
This section may be too technical for most readers to understand. (February 2020) |
Cryptococcus neoformans typically grows as a
The first genome sequence for a strain of C. neoformans (var. neoformans; now C. deneoformans) was published in 2005.[11]
Studies suggest that colonies of C. neoformans and related fungi growing within the ruins of the Chernobyl Nuclear Power Plant may be able to metabolize ionizing radiation.[12]
Pathology
Infection with C. neoformans is termed
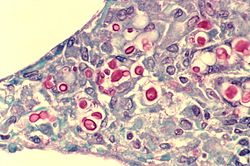
In human infection, C. neoformans is spread by inhalation of aerosolized basidiospores, and can disseminate to the central nervous system, where it can cause meningoencephalitis.[20] In the lungs, C. neoformans cells are phagocytosed by alveolar macrophages.[21] Macrophages produce oxidative and nitrosative agents, creating a hostile environment, to kill invading pathogens.[22] However, some C. neoformans cells can survive intracellularly in macrophages.[21] Intracellular survival appears to be the basis for latency, disseminated disease, and resistance to eradication by antifungal agents. One mechanism by which C. neoformans survives the hostile intracellular environment of the macrophage involves upregulation of expression of genes involved in responses to oxidative stress.[21]
Traversal of the blood–brain barrier by C. neoformans plays a key role in meningitis pathogenesis.
Meiosis (sexual reproduction), another possible survival factor for intracellular C. neoformans
The vast majority of environmental and clinical isolates of C. neoformans are mating type alpha. Filaments of mating type alpha have haploid nuclei ordinarily, but these can undergo a process of diploidization (perhaps by endoduplication or stimulated nuclear fusion) to form diploid cells termed
Serious complications of human infection
Infection starts in lungs, disseminates via blood to meninges and then to other parts of the body. Capsule inhibits phagocytosis. Can cause a systemic infection, including fatal meningitis known as meningoencephalitis in normal, diabetic and immunocompromised hosts. The infection from C. neoformans in the brain can be fatal if untreated. CNS (central nervous system) infection may also be present as a brain abscess known as cryptococcomas, subdural effusion, dementia, isolated cranial nerve lesion, spinal cord lesion, and ischemic stroke. If cryptococcal meningitis occurs, mortality rate is between 10 and 30%.[28] Cryptococcal meningitis causes more than 180000 deaths annually[29].The estimated one-year mortality of HIV-related people who receive treatment for cryptococcal meningitis is 70% in low-income countries versus 20–30% for high-income countries.[30] The symptoms include headache, fever, neck stiffness, nausea and vomiting, photophobia. The diagnosis methods contain a serum cryptococcal antigen test and lumbar puncture with cerebrospinal fluid (CSF) examination to find out the Cryptococcus neoformans.[31]
Treatment
Cryptococcosis that does not affect the central nervous system can be treated with fluconazole alone.
Cryptococcal meningitis should be treated for two weeks with intravenous
A single high dose of liposomal amphotericin B with 14 days of flucytosine and fluconazole is recommended by the newest WHO guideline for cryptococcal meningitis.[36] A new study found that brain glucose can trigger amphotericin B (AmB) tolerance of C. neoformans during meningitis which means it needs longer treatment time to kill the fungal cells. The study found that the brain glucose induced AmB tolerance of C. neoformans via glucose repression activator Mig1. Mig1 inhibits the production of ergosterol, the target of AmB, and promotes the production of inositol phosphoryl ceramide (IPC), which competes with AmB for ergosterol to limit AmB efficacy in mouse brain and human CSF. Strikingly, Results of this study indicated that IPC synthase inhibitor aureobasidin A (AbA) can enhance the anti-cryptococcal activity of AmB. AbA+AmB AmB had an even better therapeutic effect in a mouse model of cryptococcal meningitis than AmB+flucytosine which may bring new hope for the treatment of Cryptococcal meningitis.[37]
In Africa, oral fluconazole at a rate of 200 mg daily is often used. However, this does not result in cure, because it merely suppresses the fungus and does not kill it; viable fungus can continue to be grown from cerebrospinal fluid of patients not having taken fluconazole for many months. An increased dose of 400 mg daily does not improve outcomes,[38] but prospective studies from Uganda and Malawi reported that higher doses of 1200 mg per day have more fungicidal activity.[39] The outcomes with fluconazole monotherapy have 30% worse survival than amphotericin-based therapies, in a recent systematic review.[40]
References
- ^ PMID 9452400.
- PMID 18802457.
- PMID 32956032.
- PMID 25721988.
- PMID 765816.
- ISBN 9781683671220.
- PMID 6171578.
- PMID 8862601.
- PMID 17642731.
- PMID 16272534.
- PMID 15653466.
- PMID 17520016.
- PMID 22783238.
- PMID 19265539.
- PMID 18936186.
- PMID 24743149.
- S2CID 1612240.
- S2CID 11639313.
- PMID 22127880.
- PMID 19620339.
- ^ PMID 16087747.
- PMID 2050398.
- PMID 22460646.
- PMID 24398759.
- ^ "Fungal protein found to cross blood-brain barrier".
- ^ S2CID 52857557.
- PMID 18295550.
- ^ Canada, Public Health Agency of (August 19, 2011). "Pathogen Safety Data Sheets: Infectious Substances – Cryptococcus neoformans". www.canada.ca.
- ^ {{Chen, L. et al. (2024) ‘Brain glucose induces tolerance of Cryptococcus neoformans to amphotericin B during meningitis’, Nature Microbiology [Preprint]. Available at: https://doi.org/10.1038/s41564-023-01561-1}}
- ^ Rajasingham, R. et al. (2017) ‘Global burden of disease of HIV-associated cryptococcal meningitis: an updated analysis’, The Lancet Infectious Diseases, 17(8), pp. 873–881. Available at: https://doi.org/10.1016/S1473-3099(17)30243-8
- ^ Guidelines for diagnosing, preventing and managing cryptococcal disease among adults, adolescents and children living with HIV from WHO 2022 https://www.who.int/publications/i/item/9789240052178
- PMID 10770733.
- PMID 11101078.
- PMID 12746781.
- PMID 5479794.
- ^ "New guidelines from WHO recommend a simpler, safer treatment for cryptococcal disease in people living with HIV".
- ^ {{Chen, L. et al. (2024) ‘Brain glucose induces tolerance of Cryptococcus neoformans to amphotericin B during meningitis’, Nature Microbiology [Preprint]. Available at: https://doi.org/10.1038/s41564-023-01561-1}}
- PMID 16846523.
- PMID 18990067.
- PMID 23055838.
External links
 Media related to Cryptococcus neoformans at Wikimedia Commons
Media related to Cryptococcus neoformans at Wikimedia Commons- A good overview of Cryptococcus neoformans biology from the Science Creative Quarterly
- Cryptococcus neoformans biology, general information, life cycle image at MetaPathogen
- The outcome of Cryptococcus neoformans intracellular pathogenesis in human monocytes
