SOD1
Ensembl | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| UniProt | |||||||||
| RefSeq (mRNA) | |||||||||
| RefSeq (protein) | |||||||||
| Location (UCSC) | Chr 21: 31.66 – 31.67 Mb | Chr 16: 90.02 – 90.02 Mb | |||||||
| PubMed search | [3] | [4] | |||||||
| View/Edit Human | View/Edit Mouse |
Superoxide dismutase [Cu-Zn] also known as superoxide dismutase 1 or hSod1 is an
Structure
SOD1 is a 32 kDa
Function
SOD1 binds copper and zinc ions and is one of three superoxide dismutases responsible for destroying free superoxide radicals in the body. The encoded isozyme is a soluble cytoplasmic and mitochondrial intermembrane space protein, acting as a homodimer to convert naturally occurring, but harmful, superoxide radicals to molecular oxygen and hydrogen peroxide.[9][11] Hydrogen peroxide can then be broken down by another enzyme called catalase.
SOD1 has been postulated to
Clinical significance
Role in oxidative stress
Most notably, SOD1 is pivotal in
In one study, deletions in the gene were reported in two familial cases of
Amyotrophic lateral sclerosis (Lou Gehrig's disease)
Mutations (over 150 identified to date) in this gene have been linked to
Virtually all known ALS-causing SOD1 mutations act in a dominant fashion; a single mutant copy of the SOD1 gene is sufficient to cause the disease. The exact molecular mechanism (or mechanisms) by which SOD1 mutations cause disease are unknown. It appears to be some sort of toxic gain of function,[21] as many disease-associated SOD1 mutants (including G93A and A4V) retain enzymatic activity and Sod1 knockout mice do not develop ALS (although they do exhibit a strong age-dependent distal motor neuropathy).
A4V mutation
A4V (alanine at codon 4 changed to valine) is the most common ALS-causing mutation in the U.S. population, with approximately 50% of SOD1-ALS patients carrying the A4V mutation.[25][26][27] Approximately 10 percent of all U.S. familial ALS cases are caused by heterozygous A4V mutations in SOD1. The mutation is rarely if ever found outside the Americas.
It was recently estimated that the A4V mutation occurred 540 generations (~12,000 years) ago. The haplotype surrounding the mutation suggests that the A4V mutation arose in the Asian ancestors of Native Americans, who reached the Americas through the Bering Strait.[28]
The A4V mutant belongs to the WT-like mutants. Patients with A4V mutations exhibit variable age of onset, but uniformly very rapid disease course, with average survival after onset of 1.4 years (versus 3–5 years with other dominant SOD1 mutations, and in some cases such as H46R, considerably longer). This survival is considerably shorter than non-mutant SOD1 linked ALS.
H46R mutation
H46R (histidine at codon 46 changed to arginine) is the most common ALS-causing mutation in the Japanese population, with about 40% of Japanese SOD1-ALS patients carrying this mutation. H46R causes a profound loss of copper binding in the active site of SOD1, and as such, H46R is enzymatically inactive. The disease course of this mutation is extremely long, with the typical time from onset to death being over 15 years.[29] Mouse models with this mutation do not exhibit the classical mitochondrial vacuolation pathology seen in G93A and G37R ALS mice and unlike G93A mice, deficiency of the major mitochondrial antioxidant enzyme, SOD2, has no effect on their disease course.[29]
G93A mutation
G93A (glycine 93 changed to alanine) is a comparatively rare mutation, but has been studied very intensely as it was the first mutation to be modeled in mice. G93A is a pseudo-WT mutation that leaves the enzyme activity intact.[27] Because of the ready availability of the G93A mouse from Jackson Laboratory, many studies of potential drug targets and toxicity mechanisms have been carried out in this model. At least one private research institute (ALS Therapy Development Institute) is conducting large-scale drug screens exclusively in this mouse model. Whether findings are specific for G93A or applicable to all ALS-causing SOD1 mutations is at present unknown. It has been argued that certain pathological features of the G93A mouse are due to overexpression artifacts, specifically those relating to mitochondrial vacuolation (the G93A mouse commonly used from Jackson Lab has over 20 copies of the human SOD1 gene).[30] At least one study has found that certain features of pathology are idiosyncratic to G93A and not extrapolatable to all ALS-causing mutations.[29] Further studies have shown that the pathogenesis of the G93A and H46R models are clearly distinct; some drugs and genetic interventions that are highly beneficial/detrimental in one model have either the opposite or no effect in the other.[31][32][33]
Down syndrome
Down syndrome (DS) is usually caused by a triplication of chromosome 21. Oxidative stress is thought to be an important underlying factor in DS-related pathologies. The oxidative stress appears to be due to the triplication and increased expression of the SOD1 gene located in chromosome 21. Increased expression of SOD1 likely causes increased production of hydrogen peroxide leading to increased cellular injury.
The levels of 8-OHdG in the DNA of persons with DS, measured in saliva, were found to be significantly higher than in control groups.[34] 8-OHdG levels were also increased in the leukocytes of persons with DS compared to controls.[35] These findings suggest that oxidative DNA damage may lead to some of the clinical features of DS.
Interactions
SOD1 has been shown to
References
- ^ a b c GRCh38: Ensembl release 89: ENSG00000142168 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000022982 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- PMID 21603028.
- ^ S2CID 265436.
- PMID 32144830.
- ^ PMID 25463043.
- ^ PMID 25433341.
- ^ PMID 15475574.
- ^ a b "Entrez Gene: SOD1 superoxide dismutase 1, soluble (amyotrophic lateral sclerosis 1 (adult))".
- S2CID 10556268.
- PMID 4056048.
- PMID 25868322.
- S2CID 24815784.
- PMID 16877401.
- PMID 17640558.
- PMID 26076368.
- S2CID 33105812.
- S2CID 21577500.
- ^ PMID 22482452.
- S2CID 207065284.
- S2CID 2102463.
- PMID 11311985.
- PMID 7951249.
- S2CID 25595595.
- ^ PMID 12655070.
- S2CID 46282375.
- ^ S2CID 23971601.
- PMID 16624935.
- PMID 22438926.
- S2CID 11227242.
- PMID 21600285.
- PMID 23714170.
- S2CID 13657691.
- PMID 9726962.
- S2CID 18141051.
- PMID 20561900.
- S2CID 25059353.
- S2CID 26076370.
Further reading
- de Belleroche J, Orrell R, King A (November 1995). "Familial amyotrophic lateral sclerosis/motor neurone disease (FALS): a review of current developments". Journal of Medical Genetics. 32 (11): 841–847. PMID 8592323.
- Ceroni M, Curti D, Alimonti D (2002). "Amyotrophic lateral sclerosis and SOD1 gene: an overview". Functional Neurology. 16 (4 Suppl): 171–180. PMID 11996514.
- Zelko IN, Mariani TJ, Folz RJ (August 2002). "Superoxide dismutase multigene family: a comparison of the CuZn-SOD (SOD1), Mn-SOD (SOD2), and EC-SOD (SOD3) gene structures, evolution, and expression". Free Radical Biology & Medicine. 33 (3): 337–349. PMID 12126755.
- Hadano S (June 2002). "[Causative genes for familial amyotrophic lateral sclerosis]". Seikagaku. The Journal of Japanese Biochemical Society. 74 (6): 483–489. PMID 12138710.
- Noor R, Mittal S, Iqbal J (September 2002). "Superoxide dismutase--applications and relevance to human diseases". Medical Science Monitor. 8 (9): RA210–RA215. PMID 12218958.
- Potter SZ, Valentine JS (April 2003). "The perplexing role of copper-zinc superoxide dismutase in amyotrophic lateral sclerosis (Lou Gehrig's disease)". Journal of Biological Inorganic Chemistry. 8 (4): 373–380. S2CID 22820101.
- Rotilio G, Aquilano K, Ciriolo MR (2004). "Interplay of Cu,Zn superoxide dismutase and nitric oxide synthase in neurodegenerative processes". IUBMB Life. 55 (10–11): 629–634. S2CID 19518719.
- Jafari-Schluep HF, Khoris J, Mayeux-Portas V, Hand C, Rouleau G, Camu W (January 2004). "[Superoxyde dismutase 1 gene abnormalities in familial amyotrophic lateral sclerosis: phenotype/genotype correlations. The French experience and review of the literature]". Revue Neurologique. 160 (1): 44–50. PMID 14978393.
- Faraci FM, Didion SP (August 2004). "Vascular protection: superoxide dismutase isoforms in the vessel wall". Arteriosclerosis, Thrombosis, and Vascular Biology. 24 (8): 1367–1373. PMID 15166009.
- Gagliardi S, Ogliari P, Davin A, Corato M, Cova E, Abel K, et al. (August 2011). "Flavin-containing monooxygenase mRNA levels are up-regulated in als brain areas in SOD1-mutant mice". Neurotoxicity Research. 20 (2): 150–158. S2CID 21856030.
- Battistini S, Ricci C, Lotti EM, Benigni M, Gagliardi S, Zucco R, et al. (June 2010). "Severe familial ALS with a novel exon 4 mutation (L106F) in the SOD1 gene". Journal of the Neurological Sciences. 293 (1–2): 112–115. S2CID 24895265.
112-115. sod 1








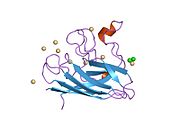




















![2nnx: Crystal Structure of the H46R, H48Q double mutant of human [Cu-Zn] Superoxide Dismutase](http://upload.wikimedia.org/wikipedia/commons/thumb/5/5f/PDB_2nnx_EBI.png/180px-PDB_2nnx_EBI.png)