Seminoma
| Seminoma | |
|---|---|
| Other names | Pure seminoma, classical seminoma |
 | |
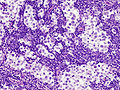
| Histopathology of classical seminoma, with typical features.[1] | |
| Specialty | Urology, oncology |

A seminoma is a germ cell tumor of the testicle or, more rarely, the mediastinum or other extra-gonadal locations. It is a malignant neoplasm and is one of the most treatable and curable cancers, with a survival rate above 95% if discovered in early stages.[3]
Testicular seminoma originates in the germinal epithelium of the seminiferous tubules.[4] About half of germ cell tumors of the testicles are seminomas.[5] Treatment usually requires removal of one testicle. However, fertility usually isn't affected. All other sexual functions will remain intact.
Signs and symptoms
The average age of diagnosis is between 35 and 50 years. This is about 5 to 10 years older than men with other germ cell tumors of the testes. In most cases, they produce masses that are readily felt on
Some cases of seminoma can present as a primary tumour outside the testis, most commonly in the mediastinum.[6] In the ovary, the tumor is called a dysgerminoma, and in non-gonadal sites, particularly the central nervous system, it is called a germinoma.[5]
Diagnosis

The cut surface of the tumour is fleshy and lobulated, and varies in colour from cream to tan to pink. The tumour tends to bulge from the cut surface, and small areas of
Microscopic examination shows that seminomas are usually composed of either a sheet-like or lobular pattern of cells with a fibrous
-
Gross pathology of seminoma
-
Histopathological image of metastatic seminoma in the inguinal lymph node. Hematoxylin & eosin stain.
-
Histopathological image of metastatic seminoma in the inguinal lymph node. At higher magnification. Hematoxylin & eosin stain.
-
Micrograph (high magnification) of a seminoma. H&E stain.
-
Testicular seminoma, showing a typically prominentstromaseparating the clusters of tumor cells.
-
Orchidectomyspecimen showing seminoma
-
The germ cell markersCD117 (positive immunohistochemistry pictured) are useful for diagnosis.[10]
Relation to spermatocytic tumor
Treatment
Intratesticular masses that appear suspicious on an
The preferred treatment for most forms of stage 1 seminoma is active surveillance. Stage 1 seminoma is characterized by the absence of clinical evidence of metastasis. Active surveillance consists of periodic history and physical examinations, tumor marker analysis, and radiographic imaging. Around 85-95% of these cases will require no further treatment. Modern radiotherapy techniques as well as one or two cycles of single-agent carboplatin have been shown to reduce the risk of relapse, but carry the potential of causing delayed side effects. Regardless of treatment strategy, stage 1 seminoma has nearly a 100% cure rate.[13]
Stage 2 seminoma is indicated by the presence of retroperitoneal metastasis. Cases require radiotherapy or, in advanced cases, combination chemotherapy. Large residual masses found after chemotherapy may require surgical resection. Second-line treatment is the same as for nonseminomas.[12]
Stage 3 seminoma is characterized by the presence of metastasis outside the retroperitoneum—the lungs in "good risk" cases or elsewhere in "intermediate risk" cases. This is treated with combination chemotherapy. Second-line treatment follows nonseminoma protocols.[12]
References
- ^ By Mikael Häggström, MD. Reference for findings: Michelle R. Downes, M.D. "Testis & paratestis - Seminoma". Pathology Outlines. Last author update: 7 January 2020. Last staff update: 19 April 2022
- PMID 10851829.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - ^ "Testicular cancer". Medline Plus. Retrieved 13 December 2012.
- ^ "Seminoma" at Dorland's Medical Dictionary
- ^ ISBN 978-0-7817-7942-5.
- ^ PMID 10355653.
- PMID 2148879.
- S2CID 7015398.
- PMID 7505805. (registration required)
- ^ Michelle R. Downes, M.D. "Testis & epididymis - Germ cell tumors - Seminoma". Pathology Outlines. Topic Completed: 7 January 2020. Minor changes: 26 January 2021
- PMID 3583416.
- ^ a b c "NCCN Testicular Cancer Guidelines". NCCN Clinical Practice Guidelines in Oncology.
- PMID 24002502.






![The germ cell markers OCT 3/4 and CD117 (positive immunohistochemistry pictured) are useful for diagnosis.[10]](http://upload.wikimedia.org/wikipedia/commons/thumb/0/05/Positive_CD117_immunohistochemistry_in_seminoma.jpg/120px-Positive_CD117_immunohistochemistry_in_seminoma.jpg)