Transitional cell carcinoma
This article needs additional citations for verification. (September 2016) |
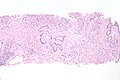
| Transitional cell carcinoma | |
|---|---|
| Other names | Urothelial carcinoma |
Hematoxylin and eosin stain. | |
| Specialty | Oncology |
Transitional cell carcinoma is a type of cancer that arises from the transitional epithelium, a tissue lining the inner surface of these hollow organs.[1] It typically occurs in the urothelium of the urinary system; in that case, it is also called urothelial carcinoma. It is the most common type of bladder cancer and cancer of the ureter, urethra, and urachus. Symptoms of urothelial carcinoma in the bladder include hematuria (blood in the urine). Diagnosis includes urine analysis and imaging of the urinary tract (cystoscopy).
It accounts for 95% of bladder cancer cases and bladder cancer is in the top 10 most common malignancy disease in the world and is associated with approximately 200,000 deaths per year in the United States alone.[2][3] It is the second most common type of kidney cancer, but accounts for only five to 10 percent of all primary renal malignant tumors.[4] Men and older people have a higher rate of urothelial carcinomas. Other risk factors include smoking and exposure to aromatic amines.[5]
Treatment approaches depend on the stage and spread of the tumour. Tumour removal (resection), chemotherapy and chemoradiation may be indicated.
Signs and symptoms
Signs and symptoms of transitional cell carcinomas depend on the location and extent of the cancer. Symptoms of bladder cancer is blood in the urine.[5]
Causes
Urothelial carcinoma is a prototypical example of a
. Some particular examples are listed below:- Certain drugs, such as upper urinary tract).[7]
- Radiation exposure
- ]
- Presence of an abnormal extra chromosome, classified as a small supernumerary marker chromosome (sSMC), in this malignancy's tumor cells.[citation needed] The sSMC has an isochromosome-like structure consisting of two copies of the short (i.e. p) arm of chromosome 5. In consequence, the malignant cells bearing it have four copies of this p arm's genetic material, two from each of the normal chromosome 5's and two from the sSMC.[8] "sSMC i(5)(p10)" is the single most common recurrent structural chromosomal abnormality in transitional cell carcinoma, being present in its malignant cells in most cases of the disease. Transitional cell bladder carcinomas associated with this sSMS are more aggressive and invasive than those not associated with it.[9]
Growth and spread
Transitional cell carcinomas are often multifocal, with 30–40% of patients having more than one
Diagnosis

Transitional refers to the histological subtype of the cancerous cells as seen under a microscope.

Classification
Transitional cell carcinomas are mostly papillary (70%,[2] and 30% non-papillary).[2]
The 1973
-
Transitional cell carcinoma, being low-grade to the left, and high-grade to the right. H&E stain
-
Papillary transitional cell carcinoma, low grade
-
Histopathology of urothelial carcinoma of the urinary bladder, showing a nested pattern of invasion. Transurethral biopsy. H&E stain
-
Histopathology of urothelial carcinoma of the urinary bladder.
-
Histopathology of urothelial carcinoma of the urinary bladder.
-
Micrograph of urethral urothelial cell carcinoma. H&E stain
Treatment
Localized/early transitional cell carcinomas of bladder
Transitional cell carcinomas can be very difficult to treat. Treatment for localized stage transitional cell carcinomas is surgical resection of the tumor, but recurrence is common. Some patients are given
Localized/early transitional cell carcinomas can also be treated with infusions of
In patients with evidence of early muscular invasion, radical curative surgery in the form of a cysto-prostatectomy usually with lymph node sampling can also be performed. In such patients, a bowel loop is often used to create either a "neo-bladder" or an "ileal conduit" which act as a place for the storage of urine before it is evacuated from the body either via the urethra or a urostomy respectively.
Advanced or metastatic transitional cell carcinomas
First-line
Taxanes or vinflunine have been used as second-line therapy (after progression on a platinum containing chemotherapy).[16]
Immunotherapy such as pembrolizumab is often used as second-line therapy for metastatic urothelial carcinoma that has progressed despite treatment with GC or MVAC, however this is based on low certainty evidence.[17][5]
In May 2016, the FDA granted
In April 2021, the FDA granted accelerated approval to sacituzumab govitecan for people with locally advanced or metastatic urothelial cancer (mUC) who previously received a platinum-containing chemotherapy and either a programmed death receptor-1 (PD-1) or a programmed death-ligand 1 (PD-L1) inhibitor.[20]
Prostate
Transitional cell carcinomas can also be associated with the prostate.[21][22]
See also
References
- ^ "transitional cell carcinoma" at Dorland's Medical Dictionary
- ^ PMID 27737647.
- ^ "Types of Bladder Cancer: TCC & Other Variants". CancerCenter.com. Retrieved 2018-08-10.
- ^ "Kidney Cancer - Introduction". Cancer.Net. 2012-06-25. Retrieved 2019-12-02.
- ^ PMID 37811690.
- ^ a b "Bladder Cancer Risk Factors | Risk for Bladder Cancer". www.cancer.org. Retrieved 2023-10-14.
- PMID 19689473.
- PMID 26322288.
- PMID 16083510.
- PMID 10511795.
- S2CID 246429500.
- PMID 37938166.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - PMID 18270948.
- ^ Sauter G, Algaba F, Amin MB, Busch C, Cheville J, Gasser T, Grignon D, Hofstaedter F, Lopez-Beltran A, Epstein JI. Noninvasive urothelial neoplasias: WHO classification of noninvasive papillary urothelial tumors. In World Health Organization classification of tumors. Pathology and genetics of tumors of the urinary system and male genital organs. Eble JN, Epstein JI, Sesterhenn I (eds): Lyon, IARCC Press, p. 110, 2004
- S2CID 21471159.
- ^ Immunotherapy Proceeds to Change Bladder Cancer Treatment 2017
- PMID 29208439.
- ^ "FDA approves new, targeted treatment for bladder cancer". FDA. 18 May 2016. Archived from the original on May 19, 2016. Retrieved 20 May 2016.
- ^ Failed confirmatory trial raises questions about atezolizumab for advanced urothelial cancer. June 2017
- ^ "FDA grants accelerated approval to sacituzumab govitecan for advanced urothelial cancer". U.S. Food and Drug Administration (FDA). 13 April 2021. Archived from the original on April 13, 2021. Retrieved 13 April 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- PMID 18439852.
- PMID 12478124.