Patent ductus arteriosus
| Patent ductus arteriosus | |
|---|---|
| Other names | Persistent ductus arteriosus |
genetic conditions | |
| Diagnostic method | Echocardiography, Doppler, X-ray |
| Prevention | Screening at birth, high index of suspicion in neonates at risk |
| Treatment | Nonsteroidal anti-inflammatory drugs (NSAIDs), surgery |
Patent ductus arteriosus (PDA) is a medical condition in which the ductus arteriosus fails to close after birth: this allows a portion of oxygenated blood from the left heart to flow back to the lungs through the aorta, which has a higher blood pressure, to the pulmonary artery, which has a lower blood pressure. Symptoms are uncommon at birth and shortly thereafter, but later in the first year of life there is often the onset of an increased work of breathing and failure to gain weight at a normal rate. With time, an uncorrected PDA usually leads to pulmonary hypertension followed by right-sided heart failure.
The ductus arteriosus is a
If the congenital defect transposition of the great vessels is present in addition to a PDA, the PDA is not surgically closed since it is the only way that oxygenated blood can mix with deoxygenated blood. In these cases, prostaglandins are used to keep the PDA open, and NSAIDs are not administered until surgical correction of the two defects is completed.
In full-term newborns, PDA occurs in 1 in 2,000 births, and accounts for 5–10% of congenital heart disease cases. PDA occurs in 20–60% of all premature newborns, where its incidence inversely linked with gestational age and weight.[2]
Signs and symptoms
Common symptoms include:[citation needed]
- dyspnea(shortness of breath)
Signs include:[citation needed]
- tachycardia (a heart rate exceeding the normal resting rate)
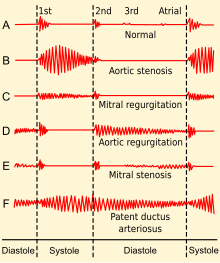
- continuous "machine-like" (also described as "rolling-thunder" and "to-and-fro") heart murmur (usually from aorta to pulmonary artery, with higher flow during systole and lower flow during diastole)
- ventricular dilation and volume overload)
- left subclavicular thrill
- bounding pulse
- widened pulse pressure
- increased cardiac output
- increased systolic pressure
- poor growth[3]
- differential cyanosis, i.e. cyanosis of the lower extremities but not of the upper body.
People with patent ductus arteriosus typically present in good health, with normal respirations and heart rate. If the PDA is moderate or large, widened
Risk factors
Known risk factors include:[6]
- Preterm birth
- Congenital rubella syndrome
- Chromosomal abnormalities (e.g., Down syndrome)
- Genetic conditions such as Loeys–Dietz syndrome (would also present with other heart defects), Wiedemann–Steiner syndrome, and CHARGE syndrome.
- Fetal Alcohol Spectrum Disorder
Diagnosis
PDA is usually diagnosed using
A chest
-
Illustration of PDA
-
PDA
-
An echocardiogram of a stented persisting ductus arteriosus: One can see the aortic arch and the stent leaving. The pulmonary artery is not seen.
-
An echocardiogram of a coiled PDA: One can see the aortic arch, the pulmonary artery, and the coil between them.
Prevention
Some evidence suggests that intravenous NSAIDs, such as
Treatment
Symptomatic PDA can be treated with both surgical and non-surgical methods.[10]
Conservative
Neonates without adverse symptoms may simply be monitored as
Surgery
Surgically, the DA may be closed by ligation (though support in premature infants is mixed).[11] This can either be performed manually and be tied shut, or with intravascular coils or plugs that leads to formation of a thrombus in the DA.[citation needed]
Devices developed by
Prostaglandin inhibitors
Because
While
Prognosis
If left untreated, the disease may progress from left-to-right shunt (
History
Adult
Since PDA is usually identified in infants, it is less common in adults, but it can have serious consequences, and is usually corrected surgically upon diagnosis.[citation needed]
See also
References
- ISBN 978-0-323-35214-7, retrieved 14 November 2023
- PMID 23055849.
- ^ a b MedlinePlus - Patent ductus arteriosus Update Date: 21 December 2009
- ^ "Medically Sound: Critical Blood Flow Redirection and a Fetus under Pressure – Fetal Heart Defects". Medically Sound. 6 October 2020. Retrieved 1 November 2020.
- PMC 5295518.
- ISSN 0733-8651.
- ^ "Tests and Diagnosis". Mayo Clinic. 16 December 2015. Retrieved 1 April 2015.
- ^ PMID 20614421.
- PMID 31985838.
- ^ Zahaka, KG and Patel, CR. "Congenital defects'". Fanaroff, AA and Martin, RJ (eds.). Neonatal-perinatal medicine: Diseases of the fetus and infant. 7th ed. (2002):1120–1139. St. Louis: Mosby.
- PMID 20808624.
- ^ Alejandra Martins (2 October 2014). "The inventions of the Bolivian doctor who saved thousands of children". BBC Mundo. Retrieved 30 March 2015.
- ^ Hines MH, Bensky AS, Hammon JW Jr et al. Video-assisted thoracoscopic ligation of patent ductus arteriosus: safe and outpatient. Ann Thorac Surg 1998;66:853–8.
- ^ circ.ahajournals.org
- ^ MayoClinic > Patent ductus arteriosus (PDA). 22 Dec. 2009
- PMID 25692606.
- PMID 29624206.
- PMID 31985831.
- PMID 29584842.
- S2CID 240438747.
- ^ "Medically Sound: Diagnosing and treating congenital heart defects". Medically Sound. 6 October 2020. Retrieved 1 November 2020.
- S2CID 228100506.
- ^ fa.hms.harvard.edu; Robert E. Gross, Harvard Medical School Office for Faculty Affairs.




