Penetrating head injury
| Penetrating head injury | |
|---|---|
| Other names | Open-head injury |
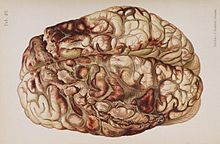 | |
| An illustration of a brain after an "encircling" gunshot wound showing the pattern of injury caused by the bullet's path | |
| Specialty | Emergency medicine |
A penetrating head injury, or open head injury, is a
A penetrating head injury involves "a wound in which an object breaches the cranium but does not exit it." In contrast, a perforating head injury is a wound in which the object passes through the head and leaves an
Cause


In penetrating injury from high-velocity missiles, injuries may occur not only from initial
Low-velocity objects usually cause penetrating injuries in the regions of the
Pathophysiology
Though it is more likely to cause
Studies with
While blunt trauma to the head does not present a risk of shock due to hemorrhage, penetrating head trauma does.[5]
Diagnosis and treatment
A person with a penetrating head injury may be evaluated using X-ray, CT scan, or MRI (MRI can only be used when the penetrating object would not be magnetic, because MRI uses magnetism and could move the object, causing further injury).[5]
Surgery may be required to debride or repair the injury or to relieve excessive intracranial pressure.[5] Intracranial pressure is monitored and attempts are made to maintain it within normal ranges.[5] Intravenous fluids are given and efforts are taken to maintain high blood oxygen levels.[5]
Prognosis
The highest-velocity injuries tend to have the worst associated damage.[7] A study published in 1991, which documented 314 individuals who had had penetrating cranial injuries caused by gunshot wounds, found that 73% died from their injuries at the scene of the incident, and a further 19% ultimately died later, thus indicating a total mortality rate of 92%.[2] Perforating injuries have an even worse prognosis.[2]
Penetrating head trauma can cause impairment or loss of abilities controlled by parts of the brain that are
People with
People with penetrating head trauma may have complications such as
See also
References
- ^ University of Vermont College of Medicine. "Neuropathology: Trauma to the CNS." Accessed through web archive on August 8, 2007.
- ^ a b c d e f g h i j Vinas FC and Pilitsis J. 2006. "Penetrating Head Trauma." Emedicine.com. Retrieved on February 6, 2007.
- PMID 17169147.
- ^ Brain Injury Association of America (BIAUSA). "Types of Brain Injury." Archived 2007-10-18 at the Wayback Machine Retrieved on February 6, 2007.
- ^ PMID 16962454.
- ^ Orlando Regional Healthcare, Education and Development. 2004. "Overview of Adult Traumatic Brain Injuries." Archived 2008-02-27 at the Wayback Machine Retrieved on January 16, 2008.
- ^ Dawodu S. 2007. "Traumatic Brain Injury: Definition, Epidemiology, Pathophysiology" Emedicine.com. Retrieved on February 6, 2007.
- S2CID 18066655.
- ^ Shepherd S. 2004. "Head Trauma." Emedicine.com. Retrieved on February 6, 2007.
