Seventh cholera pandemic
| seventh cholera pandemic | |
|---|---|
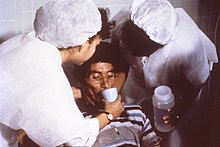 Cholera rehydration nurses | |
| Disease | Cholera |
| Bacteria strain | Vibrio cholerae biotype El Tor |
| Location | Asia, Africa, Europe, the Americas |
| First outbreak | Makassar, South Sulawesi |
| Arrival date | 1961 |
| Confirmed cases | 1,126,229 |
The seventh cholera pandemic is the
This
In 1991, the strain made a comeback in Latin America. It began in Peru, where it killed roughly 10,000 people.[5] Research has traced the origin of the strain to the seventh cholera pandemic.[6] Researchers initially suspected the strain came to Latin America through Asia from contaminated water, but samples from Latin America and samples from Africa were found to be identical.[7]

This rapid transmission of the pathogen around the globe in the 20th century can be attributed chiefly to the major hub, the Bay of Bengal, from where the disease spread.
Cholera is caused by eating food or drinking water that is contaminated with the bacteria
Introduction
The transmission of cholera is closely linked to inadequate access to clean water and sanitation facilities and hence, people at risk largely live in slums and poor communities.[10]
Epidemiology
The 7th pandemic is traced to early 1961 and is ongoing.[1] The evolution of the classical cholera strain known from the first six pandemics was revealed through genetic analysis. The first observation of the new lineage came from a laboratory in El Tor, Egypt, in 1897. By this time, the ‘El Tor’ strain differed from its relatives by 30%.[11] It originated in South-Asia, then transitioned to its non-pathogenic form in the Middle East in 1900. Sometime between 1903 and 1908, the El Tor strain picked up DNA that triggered its ability to cause disease in humans.[11] Hence, it had mutated into the El Tor pandemic strain.[12] Makassar, South Sulawesi was the source of a 1960 outbreak of the El Tor strain, where it gained new genes that likely increased transmissibility.[11] Cholera spread overseas in 1961, indicating a pandemic strain.
Many studies point to Indonesia as the source of the seventh cholera pandemic; however, research has indicated that outbreaks in China between 1960 and 1990 were associated with the same sub-lineages. These strains spread globally from the Bay of Bengal on multiple occasions.[13] China has been classified as both a sink and source during the pandemic spread of cholera throughout the 1960s and 1970s. The suggestion that the pandemic spread of cholera may have been augmented by Chinese cases, in addition to China being identified as an origin for bordering countries, contrasts with the view that the pandemic began in Indonesia.[13]
Spread and mortality
The El Tor cholera outbreak was first reported in Java, a seaside community near Kendal which was visited by travellers from Makassar in May 1961.[14] Shortly after, Semarang and Djakarta became infected in June.[citation needed]
The disease was carried into
By February 1, 1962, 4,107 people were infected with cholera, with 897 deaths (21.8% mortality). By September, despite a massive vaccination campaign, cholera had rapidly moved through the Philippines, where the number of infected people reached 15,000 by March 1962, with 2,005 deaths. In the Philippines alone, mortality reached 1,682 in 1962.[16] It was reintroduced into British Borneo, supposedly by an asymptomatic traveller from Jolo Island. Outbreaks subsequently occurred in Cambodia, Thailand, Singapore and India.[15]
In 1963, WHO declared that cholera remained the number-one killer in diseases subject to international quarantine, having been reported in Taiwan, Pakistan, Afghanistan, Iran, Southern Russia, Iraq, Korea, Burma, Cambodia, South Vietnam, Malaysia, Singapore, Nepal, Thailand, Uzbekistan and Hong Kong.[16]
The mid-60s saw cholera infiltrate Southeast Asia, with outbreaks in
The cholera strain reached the Middle East and Africa in 1970 and spread rapidly. It is thought that a traveler returning from Asia or the Middle East introduced the disease into Africa.[18] The Arabian Peninsula, Syria and Jordan became infected, followed by Guinea in August 1970. Cholera was first thought to have spread along waterways along the coast and into the interior along the rivers.
In November 1970 infected individuals seemed to travel by modernised rapid transport. This allowed cholera to extend 1,000 km, when it appeared in Mopti, Mali. Subsequently, customary large gatherings of people facilitated the outward radiation of cholera.[18] From 1970 to 1971, Sierra Leone, Liberia, Côte d'Ivoire, Ghana, Togo, Benin, Nigeria and southern Cameroon, experienced outbreaks. The west-African outbreak of cholera during 1970–1971 infected more than 400,000 persons.[19] Africa had a high cholera fatality rate of 16% by 1962. 25 countries were infected by the end of 1971 and, between 1972 and 1991, cholera spread throughout much of the remainder of Africa.[18]
Research
An international campaign began in 1970, including the research laboratory in Dhaka, Bangladesh; the Southeast Asia Treaty Organisation (SEATO), the United Kingdom, Australia, and various American agencies. Human volunteers took part in an NIH-sponsored series of tests to develop an effective cholera vaccine. At this time, new outbreaks of cholera were occurring in Egypt, South Korea, and the Soviet Union.[16]
The 1964 invention of use of oral rehydration salts (ORS) to treat cholera was endorsed by
The cholera pandemic beginning in 1962 is identified through the ‘El Tor’ biotype, and considerable research has been undertaken into this specific strain of cholera. The El Tor biotype has been demonstrated to have increased resistance to the environment.[20] This has heightened the risk of unknowing transmission from asymptomatic carriage in humans, as opposed to the classical biotype that caused the first six cholera pandemics.[citation needed]
Previously, health workers who were against the administration of the cholera vaccine based their opinion on the view that always limited resources should be directed at immediate rehydration and improved practices, and longer-term investment to provide safe water and improved sanitation. Such practices as appropriately cooking food before consumption, using sterilised water, following general personal hygiene, and sanitising environments, decrease the spread of cholera.[21] In the 21st century, cholera control activities have typically still been focused on emergency responses to outbreaks, with limited attention to the underlying causes that can prevent recurrence.[22]
But, the development of new and improved
The clinical severity of the El Tor biotype causing pandemic cholera in 1962, also resulted in modern research assessing administration of antimicrobials in the initial phase of an outbreak. This was tested in the 1970s with tetracycline but was found not to be useful due to resistance against this antibiotic.[25] Questions have been raised alluding to newer drugs, and whether the administration of these will be more useful than such previous attempts.[20]
The ongoing seventh pandemic has affirmed that cholera is still prevalent in society and can cause high mortality. In 1992 the Global Task Force on Cholera Control (GTFCC) was organized to coordinate activities and support countries after a severe cholera outbreak in Peru. Today it consists of more than 30 collaborating institutions, including NGOs, academic institutions, and UN agencies supporting affected countries.[26] In 2017 they convened a high-level meeting with officials from cholera-affected countries, donors, and technical partners to announce their strategy “The Global Roadmap to 2030”, an initiative to end cholera as a threat to public health by 2030. The three components of the strategy are: “early detection and quick response to contain the outbreaks; a multi-sectorial {sic} approach to prevent cholera recurrence, and, coordination of technical support and advocacy, resource mobilisation and partnership at the global level.[22]
References
- ^ PMID 31395455.
- ^ "Cholera factsheet" (Press release). Geneva, Switzerland: World Health Organization.
- ^ a b c Ahiarah L (6 May 2008). "Cholera". www.austincc.edu. Archived from the original on 2016-10-15. Retrieved 2015-11-24.
- ^ ISBN 9781851096589.
%22Seventh%20Cholera%20pandemic%22.
- ^ "Cholera's seven pandemics". www.cbc.ca. Retrieved 2015-11-24.
- ^ "Global epidemics and impact of cholera". www.who.int. Archived from the original on January 26, 2005. Retrieved 2015-11-24.
- PMID 20587187.
- ^ "General Information | Cholera | CDC". www.cdc.gov. 2018-12-13. Retrieved 2020-05-26.
- PMID 22748592.
- ^ "Cholera". www.who.int. Retrieved 2020-05-26.
- ^ a b c Shultz D (18 November 2016). "How today's cholera pandemic was born". Science. AAAS. Retrieved 2020-05-26.
- PMID 27849586.
- ^ PMID 25768799.
- ^ World Health Organization Regional Office for the Western Pacific (1962). "Meeting for the Exchange of Information on El Tor Vibrion Paracholera, Manila, Philippines, 16-19 April 1962 : final report".
{{cite journal}}: Cite journal requires|journal=(help) - ^ PMID 13962884.
- ^ )
- PMID 25197514.
- ^ ISBN 978-1-55581-067-2.
- S2CID 44643420.
- ^ PMID 21283611.
- PMID 31258350.
- ^ PMID 29379258.
- PMID 3879198.
- ^ "Cholera Fact Sheet". www.health.ny.gov. 2017. Retrieved 2020-05-26.
- PMID 11381101.
- ^ "Global Task Force on Cholera Control". GTFCC. 2017. Retrieved 26 July 2022.
