Snakebite
| Snakebite | |
|---|---|
drunkenness[6] | |
| Prevention | Protective footwear, avoiding areas where snakes live, not handling snakes[1] |
| Treatment | Washing the wound with soap and water, antivenom[1][7] |
| Prognosis | Depends on type of snake[8] |
| Frequency | Up to 5 million a year[3] |
| Deaths | 94,000–125,000 per year[3] |
A snakebite is an injury caused by the bite of a snake, especially a
The outcome depends on the type of snake, the area of the body bitten, the amount of snake venom injected, the general health of the person bitten and whether or not anti-venom serum has been administered by a doctor in a timely manner.[11][8] Problems are often more severe in children than adults, due to their smaller size.[3][12][13] Allergic reactions to snake venom can further complicate outcomes and can include anaphylaxis, requiring additional treatment and in some cases resulting in death.[11]
Snakes bite both as a method of hunting, and as a means of protection.
Prevention of snake bites can involve wearing protective footwear, avoiding areas where snakes live, and not handling snakes.[1] Treatment partly depends on the type of snake.[1] Washing the wound with soap and water and holding the limb still is recommended.[1][7] Trying to suck out the venom, cutting the wound with a knife, or using a tourniquet is not recommended.[1] Antivenom is effective at preventing death from bites; however, antivenoms frequently have side effects.[3][18] The type of antivenom needed depends on the type of snake involved.[7] When the type of snake is unknown, antivenom is often given based on the types known to be in the area.[7] In some areas of the world, getting the right type of antivenom is difficult and this partly contributes to why they sometimes do not work.[3] An additional issue is the cost of these medications.[3] Antivenom has little effect on the area around the bite itself.[7] Supporting the person's breathing is sometimes also required.[7]
The number of venomous snakebites that occur each year may be as high as five million.[3] They result in about 2.5 million envenomations and 20,000 to 125,000 deaths.[3][14] The frequency and severity of bites vary greatly among different parts of the world.[14] They occur most commonly in Africa, Asia, and Latin America,[3] with rural areas more greatly affected.[3][13] Deaths are relatively rare in Australia, Europe and North America.[14][18][19] For example, in the United States, about seven to eight thousand people per year are bitten by venomous snakes (about one in 40 thousand people) and about five people die (about one death per 65 million people).[1]
Signs and symptoms

The most common first symptom of all snakebites is an overwhelming fear, which may contribute to other symptoms, and may include
Dry snakebites and those inflicted by a non-venomous species may still cause severe injury. The bite may become infected from the snake's saliva. The fangs sometimes harbor pathogenic microbial organisms, including Clostridium tetani, and may require an updated tetanus immunization.[24][15]
Most snakebites, from either a venomous or a non-venomous snake, will have some type of local effect.
Bites by some snakes, such as the
Some Australian elapids and most viper envenomations will cause
The venom of elapids, including
Venom emitted from some types of cobras, almost all vipers and some sea snakes causes necrosis of muscle tissue.[18] Muscle tissue will begin to die throughout the body, a condition known as rhabdomyolysis. Rhabdomyolysis can result in damage to the kidneys as a result of myoglobin accumulation in the renal tubules. This, coupled with hypotension, can lead to acute kidney injury, and, if left untreated, eventually death.[18]
Snakebite is also known to cause depression and post-traumatic stress disorder in a high proportion of people who survive.[33]
Cause
In the developing world most snakebites occur in those who work outside such as farmers, hunters, and fishermen. They often happen when a person steps on the snake or approaches it too closely. In the United States and Europe snakebites most commonly occur in those who keep them as pets.[34]
The type of snake that most often delivers serious bites depends on the region of the world. In Africa, it is
Pathophysiology
Since
Some dry bites may also be the result of imprecise timing on the snake's part, as venom may be prematurely released before the fangs have penetrated the person.
While most snakes must open their mouths before biting, African and Middle Eastern snakes belonging to the family Atractaspididae are able to fold their fangs to the side of their head without opening their mouth and jab a person.[38]
Snake venom
It has been suggested that snakes evolved the mechanisms necessary for venom formation and delivery sometime during the Miocene epoch.[39] During the mid-Tertiary, most snakes were large ambush predators belonging to the superfamily Henophidia, which use constriction to kill their prey. As open grasslands replaced forested areas in parts of the world, some snake families evolved to become smaller and thus more agile. However, subduing and killing prey became more difficult for the smaller snakes, leading to the evolution of snake venom. The most likely hypothesis holds that venom glands evolved from specialized salivary glands. The venom itself evolved through the process of natural selection; it retained and emphasized the qualities that made it useful in killing or subduing prey. Today we can find various snake species in stages of this hypothesized development. There are the highly efficient envenoming machines - like the rattlesnakes - with large capacity venom storage, hollow fangs that swing into position immediately before the snake bites, and spare fangs ready to replace those damaged or lost.[40][39] Other research on Toxicofera, a hypothetical clade thought to be ancestral to most living reptiles, suggests an earlier time frame for the evolution of snake venom, possibly to the order of tens of millions of years, during the Late Cretaceous.[41]
Snake venom is produced in modified
Venom in many snakes, such as pit vipers, affects virtually every organ system in the human body and can be a combination of many toxins, including
In
Snake venom is known to cause neuromuscular paralysis, usually as a flaccid paralysis that is descending; starting at the facial muscles, causing ptosis or drooping eyelids and dysarthria or poor articulation of speech, and descending to the respiratory muscles causing respiratory compromise.[43] The neurotoxins can either bind to and block membrane receptors at the post-synaptic neurons or they can be taken up into the pre-synaptic neuron cells and impair neurotransmitter release.[43] Venom toxins that are taken up intra-cellularly, into the cells of the pre-synaptic neurons are much more difficult to reverse using anti-venom as they are inaccessible to the anti-venom when they are intracellular.[43]
The strength of venom differs markedly between species and even more so between families, as measured by
Prevention
Snakes are most likely to bite when they feel threatened, are startled, are provoked, or when they have been cornered. Snakes are likely to approach residential areas when attracted by prey, such as
When in the wilderness, treading heavily creates ground vibrations and noise, which will often cause snakes to flee from the area. However, this generally only applies to vipers, as some larger and more aggressive snakes in other parts of the world, such as mambas and cobras,[45] will respond more aggressively. If presented with a direct encounter, it is best to remain silent and motionless. If the snake has not yet fled, it is important to step away slowly and cautiously.[citation needed]
The use of a flashlight when engaged in camping activities, such as gathering firewood at night, can be helpful. Snakes may also be unusually active during especially warm nights when ambient temperatures exceed 21 °C (70 °F). It is advised not to reach blindly into hollow logs, flip over large rocks, and enter old cabins or other potential snake hiding-places. When rock climbing, it is not safe to grab ledges or crevices without examining them first, as snakes are cold-blooded and often sunbathe atop rock ledges.[citation needed]
In the United States, more than 40 percent of people bitten by snakes intentionally put themselves in harm's way by attempting to capture wild snakes or by carelessly handling their dangerous pets—40 percent of that number had a
It is also important to avoid snakes that
As a dead snake is incapable of regulating the venom injected, a bite from a dead snake can often contain large amounts of venom.[48]Treatment
It may be difficult to determine if a bite by any species of snake is life-threatening. A bite by a North American
Snake identification
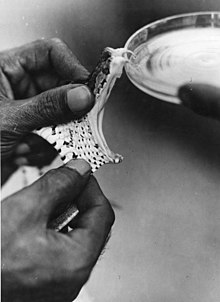
Identification of the snake is important in planning treatment in certain areas of the world, but is not always possible. Ideally the dead snake would be brought in with the person, but in areas where snake bite is more common, local knowledge may be sufficient to recognize the snake. However, in regions where polyvalent antivenoms are available, such as North America, identification of snake is not a high priority item. Attempting to catch or kill the offending snake also puts one at risk for re-envenomation or creating a second person bitten, and generally is not recommended.[52]
The three types of venomous snakes that cause the majority of major clinical problems are
First aid
Snakebite first aid recommendations vary, in part because different snakes have different types of venom. Some have little local effect, but life-threatening systemic effects, in which case containing the venom in the region of the bite by pressure immobilization is desirable. Other venoms instigate localized tissue damage around the bitten area, and immobilization may increase the severity of the damage in this area, but also reduce the total area affected; whether this trade-off is desirable remains a point of controversy. Because snakes vary from one country to another, first aid methods also vary.[citation needed]
Many organizations, including the American Medical Association and American Red Cross, recommend washing the bite with soap and water. Australian recommendations for snake bite treatment recommend against cleaning the wound. Traces of venom left on the skin/bandages from the strike can be used in combination with a snake bite identification kit to identify the species of snake. This speeds determination of which antivenom to administer in the emergency room.[54]
Pressure immobilization
As of 2008, clinical evidence for
The object of pressure immobilization is to contain venom within a bitten limb and prevent it from moving through the lymphatic system to the vital organs. This therapy has two components: pressure to prevent lymphatic drainage, and immobilization of the bitten limb to prevent the pumping action of the skeletal muscles.[citation needed]
Antivenom
Until the advent of
Antivenom is injected into the person intravenously, and works by binding to and neutralizing venom enzymes. It cannot undo damage already caused by venom, so antivenom treatment should be sought as soon as possible. Modern antivenoms are usually polyvalent, making them effective against the venom of numerous snake species. Pharmaceutical companies which produce antivenom target their products against the species native to a particular area. Although some people may develop serious adverse reactions to antivenom, such as anaphylaxis, in emergency situations this is usually treatable and hence the benefit outweighs the potential consequences of not using antivenom. Giving adrenaline (epinephrine) to prevent adverse reactions to antivenom before they occur might be reasonable in cases where they occur commonly.[60] Antihistamines do not appear to provide any benefit in preventing adverse reactions.[60]
Chronic Complications
Chronic health effects of snakebite include but is not limited to non-healing and chronic ulcers, musculoskeletal disorders, amputations, chronic kidney disease, and other neurological and endocrine complications.[61][62] The treatment of chronic complications of snakebite has not been well researched and there a systems approach consisting of a multi-component intervention.[63][50]
Outmoded

The following treatments, while once recommended, are considered of no use or harmful, including tourniquets, incisions, suction, application of cold, and application of electricity.[57] Cases in which these treatments appear to work may be the result of dry bites.
- Application of a tourniquet to the bitten limb is generally not recommended. There is no convincing evidence that it is an effective first-aid tool as ordinarily applied.[64] Tourniquets have been found to be completely ineffective in the treatment of Crotalus durissus bites,[65] but some positive results have been seen with properly applied tourniquets for cobra venom in the Philippines.[66] Uninformed tourniquet use is dangerous, since reducing or cutting off circulation can lead to gangrene, which can be fatal.[64] The use of a compression bandage is generally as effective, and much safer.
- Cutting open the bitten area, an action often taken prior to suction, is not recommended since it causes further damage and increases the risk of infection; the subsequent cauterization of the area with fire or silver nitrate (also known as infernal stone) is also potentially threatening.[67]
- Sucking out venom, either by mouth or with a pump, does not work and may harm the affected area directly.[68] Suction started after three minutes removes a clinically insignificant quantity—less than one-thousandth of the venom injected—as shown in a human study.[69] In a study with pigs, suction not only caused no improvement but led to necrosis in the suctioned area.[70] Suctioning by mouth presents a risk of further poisoning through the mouth's mucous tissues.[71] The helper may also release bacteria into the person's wound, leading to infection.
- Immersion in warm water or sour milk, followed by the application of snake-stones(also known as la Pierre Noire), which are believed to draw off the poison in much the way a sponge soaks up water.
- Application of a one-percent solution of potassium permanganate or chromic acid to the cut, exposed area.[67] The latter substance is notably toxic and carcinogenic.
- Drinking abundant quantities of alcohol following the cauterization or disinfection of the wound area.[67]
- Use of electroshock therapy in animal tests has shown this treatment to be useless and potentially dangerous.[72][73][74][75]
In extreme cases, in remote areas, all of these misguided attempts at treatment have resulted in injuries far worse than an otherwise mild to moderate snakebite. In worst-case scenarios, thoroughly constricting tourniquets have been applied to bitten limbs, completely shutting off blood flow to the area. By the time the person finally reached appropriate medical facilities their limbs had to be
In development
Several new drugs and treatments are under development for snakebite. For instance, the metal chelator dimercaprol has recently been shown to potently antagonize the activity of Zn2+-dependent snake venom metalloproteinases in vitro.[76] New monoclonal antibodies, polymer gels and a small molecule inhibitor called Varespladib are in development.[77] A core outcome set (minimal list of consensus outcomes that should be used in future intervention research) for snakebite in South Asia is being developed.[78]
Epidemiology
Earlier estimates for snakebite vary from 1.2 to 5.5 million, with 421,000 to 2.5 million being envenomings, and causing 20,000 to 125,000 deaths.[3][14] More recent modelling estimates that in 2019, about 63,400 people died globally from snakebite, with 51,100 of these deaths happenning in India.[79] Since reporting is not mandatory in much of the world, the data on the frequency of snakebites is not precise.[14] Many people who survive bites have permanent tissue damage caused by venom, leading to disability.[18] Most snake envenomings and fatalities occur in South Asia, Southeast Asia, and sub-Saharan Africa, with India reporting the most snakebite deaths of any country.[14] Available evidence on the effect of climate change on the epidemiology of snakebite is limited but it is expected that there will be a geographic shift in risk of snakebite: northwards in North America and southwards in South America and in Mozambique, and increase in incidence of bite in Sri Lanka.[80]
Most snakebites are caused by non-venomous snakes. Of the roughly 3,000 known species of snake found worldwide, only 15% are considered dangerous to humans.
Worldwide, snakebites occur most frequently in the summer season when snakes are active and humans are outdoors.[14][82] Agricultural and tropical regions report more snakebites than anywhere else.[14][28] In the United States, those bitten are typically male and between 17 and 27 years of age.[2][82][83] Children and the elderly are the most likely to die.[2][49]
Mechanics

When venomous snakes bite a target, they secrete venom through their venom delivery system. The venom delivery system generally consists of two venom glands, a compressor muscle, venom ducts, a fang sheath, and fangs. The primary and accessory venom glands store the venom quantities required during envenomation. The compressor muscle contracts during bites to increase the pressure throughout the venom delivery system. The pressurized venom travels through the primary venom duct to the secondary venom duct that leads down through the fang sheath and fang. The venom is then expelled through the exit orifice of the fang. The total volume and flow rate of venom administered into a target varies widely, sometimes as much as an order of magnitude. One of the largest factors is snake species and size, larger snakes have been shown to administer larger quantities of venom.[84]
Predatory vs. defensive bites
Snake bites are classified as either predatory or defensive in nature. During defensive strikes, the rate of venom expulsion and total volume of venom expelled is much greater than during predatory strikes. Defensive strikes can have 10 times as much venom volume expelled at 8.5 times the flow rate.[85] This can be explained by the snake's need to quickly subdue a threat. While employing similar venom expulsion mechanics, predatory strikes are quite different from defensive strikes. Snakes usually release the prey shortly after the envenomation allowing the prey to run away and die. Releasing prey prevents retaliatory damage to the snake. The venom scent allows the snake to relocate the prey once it is deceased.[84] The amount of venom injected has been shown to increase with the mass of the prey animal.[86] Larger venom volumes allow snakes to effectively euthanize larger prey while remaining economical during strikes against smaller prey. This is an important skill as venom is a metabolically expensive resource.[citation needed]
Venom Metering
Venom metering is the ability of a snake to have neurological control over the amount of venom released into a target during a strike based on situational cues. This ability would prove useful as venom is a limited resource, larger animals are less susceptible to the effects of venom, and various situations require different levels of force. There is a lot of evidence to support the venom metering hypothesis. For example, snakes frequently use more venom during defensive strikes, administer more venom to larger prey, and are capable of dry biting. A dry bite is a bite from a venomous snake that results in very little or no venom expulsion, leaving the target asymptomatic.[87] However, there is debate among many academics about venom metering in snakes. The alternative to venom metering is the pressure balance hypothesis.[citation needed]
The pressure balance hypothesis cites the retraction of the fang sheath as the many mechanism for producing outward venom flow from the venom delivery system. When isolated, fang sheath retraction has experimentally been shown to induce very high pressures in the venom delivery system.[88] A similar method was used to stimulate the compressor musculature, the main muscle responsible for the contraction and squeezing of the venom gland, and then measuring the induced pressures. It was determined that the pressure created from the fang sheath retraction was at times an order of magnitude greater than those created by the compressor musculature. Snakes do not have direct neurological control of the fang sheath, it can only be retracted as the fangs enter a target and the target's skin and body provide substantial resistance to retract the sheath. For these reasons, the pressure balance hypothesis concludes that external factors, mainly the bite and physical mechanics, are responsible for the quantity of venom expelled.[citation needed]
Venom Spitting
Venom spitting is another venom delivery method that is unique to some Asiatic and African cobras. In venom spitting, a stream of venom is propelled at very high pressures outwards up to 3 meters. The venom stream is usually aimed at the eyes and face of the target as a deterrent for predators. There are non-spitting cobras that provide useful information on the unique mechanics behind venom spitting. Unlike the elongated oval shaped exit orifices of non-spitting cobras, spitting cobras have circular exit orifice at their fang tips.[89] This combined with the ability to partially retract their fang sheath by displacing the palato-maxillary arch and contracting the adductor mandibulae, allows the spitting cobras to create large pressures within the venom delivery system.[90] While venom spitting is a less common venom delivery system, the venom can still cause the effects if ingested.[citation needed]
Society and culture

Snakes were both
Historically, snakebites were seen as a means of execution in some cultures.
Snakebite as a surreptitious form of murder has been featured in stories such as Sir
Research
In 2018, the World Health Organization listed snakebite envenoming as a neglected tropical disease.[99][100] In 2019, they launched a strategy to prevent and control snakebite envenoming, which involved a program targeting affected communities and their health systems.[101][102] A policy analysis however found that the placement of snakebite in the global health agenda of WHO is fragile due to reluctance acceptance of the disease in the neglected tropical disease community and the perceived colonial nature of the network driving the agenda.[103]
Key institutions conducting snakebite research on snakebite are George Institute for Global Health, Liverpool School of Tropical Medicine and Indian Institute of Science.
Other animals
Several animals acquired immunity against venom of snakes that occur in the same habitat.[104] This has been documented in some humans as well.[105]
References
- ^ U.S. National Institute for Occupational Safety and Health. 24 February 2012. Archivedfrom the original on 29 April 2015. Retrieved 19 May 2015.
- ^ PMID 12151473.
- ^ a b c d e f g h i j k l m n o p q "Animal bites: Fact sheet N°373". World Health Organization. February 2015. Archived from the original on 4 May 2015. Retrieved 19 May 2015.
- ^ "Eldorado - Outdoor Safety & Ethics".
- ^ "What to do if you encounter a rattlesnake".
- ^ "Alcohol and Snake Bites – Reptiles Magazine". December 2011.
- ^ a b c d e f g h "Neglected tropical diseases: Snakebite". World Health Organization. Archived from the original on 30 September 2015. Retrieved 19 May 2015.
- ^ ISBN 978-0-323-05472-0. Archivedfrom the original on 21 May 2015.
- ^ "Definition of Snakebite". www.merriam-webster.com. Retrieved 17 June 2019.
- PMID 25109149.
- ^ a b c d Eske J, Biggers A (14 December 2018). "How to identify and treat snake bites". Medical News Today. Healthline Media UK Ltd. Retrieved 4 May 2022.
- ISBN 978-92-4-156357-4. Archivedfrom the original on 2 February 2017.
- ^ a b c "Snake antivenoms: Fact sheet N°337". World Health Organization. February 2015. Archived from the original on 18 April 2017. Retrieved 16 May 2017.
- ^ PMID 18986210.
- ^ S2CID 222070778.
- ^ World Health Organization. Prevalence of snakebite envenoming. [https://web.archive.org/web/20170922113845/http://www.who.int/snakebites/epidemiology/en/ ]. Accessed April 15, 2019
- ^ "WHO | Snakebite envenomation turns again into a neglected tropical disease!". WHO. Archived from the original on 22 September 2017.
- ^ PMID 17979738.
- PMID 9868843.
- ^ a b MedlinePlus – Snake bites Archived 4 December 2010 at the Wayback Machine From Tintinalli JE, Kelen GD, Stapcynski JS, eds. Emergency Medicine: A Comprehensive Study Guide. 6th ed. New York, NY: McGraw Hill; 2004. Update date: 27 February 2008. Updated by: Stephen C. Acosta, MD, Department of Emergency Medicine, Portland VA Medical Center, Portland, OR. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc. Retrieved on 19 mars, 2009
- ^ Health-care-clinic.org – Snake Bite First Aid – Snakebite Archived 16 January 2016 at the Wayback Machine Retrieved on 21 mars, 2009
- ^ Snake bite image example at MDconsult – Patient Education – Wounds, Cuts and Punctures, First Aid for Archived 7 January 2016 at the Wayback Machine
- PMID 3625968.
- ^ Otten E, Blomkalns A. Venomous animal injuries. In: Marx J, Hockberger R,Walls R, eds. Rosen's Emergency Medicine: Concepts and Clinical Practice. St Louis: Mosby; 2002
- ^ Lamsal S (3 June 2023). "Snakebites in Nepal are a medical emergency. Here are things you should know about them". Online Khabar. Retrieved 21 June 2023.
- PMID 1084700.
- PMID 8433414.
- ^ PMID 16729843.
- ^ Cuhna JP (6 August 2021). "Symptoms and Signs of Snakebite (Snake Bite)". eMedicineHealth. WebMD. Retrieved 26 July 2022.
- ISBN 978-1-4557-0717-1.
- ^ (PDF) from the original on 28 April 2011. Retrieved 24 July 2009.
- from the original on 27 July 2022. Retrieved 27 July 2022.
- PMID 33257419.
- ^ ISBN 978-0-444-53499-6. Archivedfrom the original on 8 September 2017.
- ISBN 978-0-394-48882-0.
- ^ .
The second major assumption that underlies venom metering is the snake's ability to accurately assess the target
- (PDF) from the original on 9 January 2009.
With the species and size of target held constant, the duration of venom flow, maximum venom flow rate and total venom volume were all significantly lower in predatory than in defensive strikes
- from the original on 7 January 2016. Retrieved 19 May 2014.
- ^ (PDF) from the original on 10 October 2012. Retrieved 25 July 2009.
- ISBN 978-0-394-48882-0.
- S2CID 4386245. Archived from the original(PDF) on 30 May 2009. Retrieved 18 September 2009.
- S2CID 1322336.
- ^ S2CID 245771267.
- ISBN 978-1-86812-575-3.
- ^ Haji R. "Venomous snakes and snake bites" (PDF). Zoocheck Canada. Archived from the original (PDF) on 25 April 2012. Retrieved 25 October 2013.
- PMID 3655676.
- PMID 1559468.
- PMID 10375322.
- ^ S2CID 37771848.
- ^ PMID 33048936.
- PMID 29662699.
- ^ PMID 33995385.
- PMID 16412486.
- ^ Chris Thompson. "Treatment of Australian Snake Bites". Australian anaesthetists' website. Archived from the original on 23 March 2007.
- S2CID 40768561.
- ^ PMID 23244230.
- ^ PMID 22065370.
- S2CID 22415445.
- ^ White J (November 1991). "Oxyuranus microlepidotus". Chemical Safety Information from Intergovernmental Organizations. Archived from the original on 3 August 2009. Retrieved 24 July 2009.
Without appropriate antivenom treatment up to 75% of taipan bites will be fatal. Indeed, in the era prior to specific antivenom therapy, virtually no survivors of taipan bite were recorded.
- ^ PMID 10796682.
- PMID 34355162.
- S2CID 237541103.
- S2CID 237541103.
- ^ (PDF) from the original on 30 December 2008.
- PMID 9655642.
- S2CID 29451180.
- ^ a b c Lupano G, Peola P (1915). Corso di Scienze Naturali a uso delle Scuole Complementari [A Course of Natural Sciences for the Complementary Institutes] (in Italian). G.B. Paravia. p. 68.
- PMID 16781926.
- PMID 14747805.
- PMID 11055564.
- ^ Riggs BS, Smilkstein MJ, Kulig KW, et al. Rattlesnake envenomation with massive oropharyngeal edema following incision and suction (Abstract). Presented at the AACT/AAPCC/ABMT/CAPCC Annual Scientific Meeting, Vancouver, Canada, September 27 October 2, 1987.
- PMID 3671201.
- S2CID 222260195.
- PMID 3257850.
- PMID 3438923.
- PMID 32376771.
- ^ "The search for better antivenoms heats up as snakebites get renewed attention". Chemical & Engineering News. Retrieved 15 October 2020.
- PMID 36300033.
- S2CID 253111038.
- S2CID 253452433.
- ^ S2CID 86568032. Archived from the original(PDF) on 2 June 2010. Retrieved 26 September 2009.
Estimates of the number of venomous colubrids approach 700 species. Most may not produce a venom capable of causing serious damage to humans, but at least five species (Dispholidus typus, Thelotornis capensis, Rhabdophis tigrinus, Philodryas olfersii and Tachymenis peruviana) have caused human fatalities
- ^ PMID 3277335.
- PMID 4956000.
- ^ a b Hayes WK, Herbert SS, Rehling GC, Gennaro JF (2002). "Factors that influence venom expenditure in viperids and other snake species during predatory and defensive contexts". Biology of the Vipers (PDF). Eagle Mountain Publishing. pp. 207–233.
- PMID 11815658.
- S2CID 53160144.
- S2CID 36838996.
- PMID 17094108.
- S2CID 58587928.
- PMID 15339944.
- ^ PMID 15496528.
This echoed the opinion of the Egyptian physicians who wrote the earliest known account of the treatment of snake bite, the Brooklyn Museum Papyri, dating perhaps from 2200 BC. They regarded bites by horned vipers 'fy' as non-lethal, as the victims could be saved.
- ISBN 978-0-374-71221-1.
- ^ a b c Anil A (2004). "Homicide with snakes: A distinct possibility and its medicolegal ramifications". Anil Aggrawal's Internet Journal of Forensic Medicine and Toxicology. 4 (2). Archived from the original on 18 July 2007.
- ^ Crawford A (1 April 2007). "Who Was Cleopatra? Mythology, propaganda, Liz Taylor and the real Queen of the Nile". Smithsonian. Retrieved 4 September 2009.
- ISBN 978-1-78022-114-4.
- PMID 19535618.
- from the original on 8 October 2011. Retrieved 4 September 2009.
A third unusual death was a tragic fatality (1987), recorded as a homicide, which resulted when a large rattlesnake (G. v. lutosus) bit a 22-month-old girl after the snake had been placed around her neck (Washington County). The child died in approximately 5 h.
- S2CID 21805895.
Ein etwa 20-jähriger Arbeiter wurde nach dem Biss seiner Puffotter (Bitis arietans) in die Hand auf die toxikologische Intensivstation aufgenommen. Zunächst berichtet der Patient, dass es beim "Melken" der Giftschlange zu dem Biss gekommen sei, erst im weiteren Verlauf räumt er einen Suizidversuch ein. Als Gründe werden Einsamkeit angeführt sowie unerträgliche Schmerzen im Penis.
- PMID 31129124.
- S2CID 189458866.
- ^ "Snakebite: WHO targets 50% reduction in deaths and disabilities". World Health Organization. Retrieved 30 May 2019.
- PMID 30789906.
- PMID 37604596.
- ^ Bittel J. "The Animals That Venom Can't Touch". Smithsonian. Retrieved 29 May 2018.
- ^ Collins B (11 February 2018). "Poison pass: the man who became immune to snake venom". the Guardian. Retrieved 29 May 2018.
- Bibliography
- ISBN 978-0-520-20014-2.
- Mackessy SP, ed. (2010). Handbook of Venoms and Toxins of Reptiles (2nd ed.). Boca Raton, FL: CRC Press. ISBN 978-0-8493-9165-1.
- Valenta J (2010). Venomous Snakes: Envenoming, Therapy (2nd ed.). Hauppauge, NY: Nova Science Publishers. ISBN 978-1-60876-618-5.
Further reading
- Campbell JA, Lamar WW (2004). The Venomous Reptiles of the Western Hemisphere. Ithaca, NY: Cornell University Press 978-0-8014-4141-7.
- Spawls S, Branch B (1995). The Dangerous Snakes of Africa: Natural History, Species Directory, Venoms and Snakebite. Sanibel Island, FL: Ralph Curtis Publishing. ISBN 978-0-88359-029-4.
- Sullivan JB, Wingert WA, Norris Jr RL (1995). "North American Venomous Reptile Bites". Wilderness Medicine: Management of Wilderness and Environmental Emergencies. 3: 680–709.
- Thorpe RS, ISBN 978-0-19-854986-4.
External links
- WHO Snake Antivenoms Database
- Organization (2016). Guidelines for the management of snakebites. Regional Office for South-East Asia, World Health Organization. ISBN 978-92-9022-530-0.


