X-inactivation

1.Early stage embryonic cell of a female human
2.Maternal X chromosome
3.Paternal X chromosome
4.Mitosis and random X-chromosome inactivation event
5.Paternal chromosome is randomly inactivated in one daughter cell, maternal chromosome is inactivated in the other
6.Paternal chromosome is randomly inactivated in both daughter cells
7.Maternal chromosome is randomly inactivated in both daughter cells
8.Three possible random combination outcomes

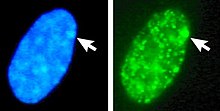
Left: DNA (DAPI)-stained nucleus. Arrow indicates the location of Barr body(Xi). Right: DNA associated histones protein detected
X-inactivation (also called Lyonization, after English geneticist
The choice of which X chromosome will be inactivated in a particular embryonic cell is random in placental mammals such as humans, but once an X chromosome is inactivated it will remain inactive throughout the lifetime of the cell and its descendants in the organism (its cell line). The result is that the choice of inactivated X chromosome in all the cells of the organism is a random distribution, often with about half the cells having the paternal X chromosome inactivated and half with an inactivated maternal X chromosome; but commonly, X-inactivation is unevenly distributed across the cell lines within one organism (skewed X-inactivation).
Unlike the random X-inactivation in placental mammals, inactivation in marsupials applies exclusively to the paternally-derived X chromosome.
Mechanism
Cycle of X-chromosome activation in rodents
The paragraphs below have to do only with rodents and do not reflect XI in the majority of mammals. X-inactivation is part of the activation cycle of the X chromosome throughout the female life. The egg and the fertilized zygote initially use maternal transcripts, and the whole embryonic genome is silenced until
In the early blastocyst, this initial, imprinted X-inactivation is reversed in the cells of the inner cell mass (which give rise to the embryo), and in these cells both X chromosomes become active again. Each of these cells then independently and randomly inactivates one copy of the X chromosome.[5] This inactivation event is irreversible during the lifetime of the individual, with the exception of the germline. In the female germline before meiotic entry, X-inactivation is reversed, so that after meiosis all haploid oocytes contain a single active X chromosome.
Overview
The Xi marks the inactive, Xa the active X chromosome. XP denotes the paternal, and XM to denotes the maternal X chromosome. When the egg (carrying XM), is fertilized by a sperm (carrying a Y or an XP) a diploid zygote forms. From zygote, through adult stage, to the next generation of eggs, the X chromosome undergoes the following changes:
- XiP XiM zygote → undergoing zygotic genome activation, leading to:
- XaP XaM → undergoing imprinted (paternal) X-inactivation, leading to:
- XiP XaM → undergoing X-activation in the early blastocyst stage, leading to:
- XaP XaM → undergoing random X-inactivation in the embryonic lineage (inner cell mass) in the blastocyst stage, leading to:
- XiP XaM OR XaP XiM → undergoing X-reactivation in primordial germ cells before meiosis, leading to:
- XaM XaP diploid germ cells in meiotic arrest. As the meiosis I only completes with ovulation, human germ cells exist in this stage from the first weeks of development until puberty. The completion of meiosis leads to:
- XaM AND XaP haploid germ cells (eggs).
The X activation cycle has been best studied in mice, but there are multiple studies in humans. As most of the evidence is coming from mice, the above scheme represents the events in mice. The completion of the meiosis is simplified here for clarity. Steps 1–4 can be studied in in vitro fertilized embryos, and in differentiating stem cells; X-reactivation happens in the developing embryo, and subsequent (6–7) steps inside the female body, therefore much harder to study.
Timing
The timing of each process depends on the species, and in many cases the precise time is actively debated. [The whole part of the human timing of X-inactivation in this table is highly questionable and should be removed until properly substantiated by empirical data]
| Process | Mouse | Human | |
| 1 | Zygotic genome activation | 2–4 cell stage[7] | 2–8 cell stage[7] |
| 2 | Imprinted (paternal) X-inactivation | 4–8 cell stage[6][8] | Unclear if it takes place in humans[9] |
| 3 | X-activation | Early blastocyst stage | Early blastocyst stage |
| 4 | Random X-inactivation in the embryonic lineage (inner cell mass) | Late blastocyst stage | Late blastocyst stage, after implantation[9] |
| 5 | X-reactivation in primordial germ cells before meiosis | From before developmental week 4 up to week 14[10][11] |
Inheritance of inactivation status across cell generations
The descendants of each cell which inactivated a particular X chromosome will also inactivate that same chromosome. This phenomenon, which can be observed in the coloration of
Selection of one active X chromosome
Typical females possess two X chromosomes, and in any given cell one chromosome will be active (designated as Xa) and one will be inactive (Xi). However, studies of individuals with extra copies of the X chromosome show that in cells with more than two X chromosomes there is still only one Xa, and all the remaining X chromosomes are inactivated. This indicates that the default state of the X chromosome in females is inactivation, but one X chromosome is always selected to remain active.
It is understood that X-chromosome inactivation is a random process, occurring at about the time of gastrulation in the epiblast (cells that will give rise to the embryo). The maternal and paternal X chromosomes have an equal probability of inactivation. This would suggest that women would be expected to suffer from X-linked disorders approximately 50% as often as men (because women have two X chromosomes, while men have only one); however, in actuality, the occurrence of these disorders in females is much lower than that. One explanation for this disparity is that 12–20% [13] of genes on the inactivated X chromosome remain expressed, thus providing women with added protection against defective genes coded by the X-chromosome. Some[who?] suggest that this disparity must be evidence of preferential (non-random) inactivation. Preferential inactivation of the paternal X-chromosome occurs in both marsupials and in cell lineages that form the membranes surrounding the embryo,[14] whereas in placental mammals either the maternally or the paternally derived X-chromosome may be inactivated in different cell lines.[15]
The time period for X-chromosome inactivation explains this disparity. Inactivation occurs in the epiblast during gastrulation, which gives rise to the embryo.[16] Inactivation occurs on a cellular level, resulting in a mosaic expression, in which patches of cells have an inactive maternal X-chromosome, while other patches have an inactive paternal X-chromosome. For example, a female heterozygous for haemophilia (an X-linked disease) would have about half of her liver cells functioning properly, which is typically enough to ensure normal blood clotting.[17][18] Chance could result in significantly more dysfunctional cells; however, such statistical extremes are unlikely. Genetic differences on the chromosome may also render one X-chromosome more likely to undergo inactivation. Also, if one X-chromosome has a mutation hindering its growth or rendering it non viable, cells which randomly inactivated that X will have a selective advantage over cells which randomly inactivated the normal allele. Thus, although inactivation is initially random, cells that inactivate a normal allele (leaving the mutated allele active) will eventually be overgrown and replaced by functionally normal cells in which nearly all have the same X-chromosome activated.[17]
It is hypothesized that there is an autosomally-encoded 'blocking factor' which binds to the X chromosome and prevents its inactivation.[19] The model postulates that there is a limiting blocking factor, so once the available blocking factor molecule binds to one X chromosome the remaining X chromosome(s) are not protected from inactivation. This model is supported by the existence of a single Xa in cells with many X chromosomes and by the existence of two active X chromosomes in cell lines with twice the normal number of autosomes.[20]
Sequences at the X inactivation center (XIC), present on the X chromosome, control the silencing of the X chromosome. The hypothetical blocking factor is predicted to bind to sequences within the XIC.
Expression of X-linked disorders in heterozygous females
The effect of female X heterozygosity is apparent in some localized traits, such as the unique coat pattern of a calico cat. It can be more difficult, however, to fully understand the expression of un-localized traits in these females, such as the expression of disease.
Since males only have one copy of the X chromosome, all expressed X-chromosomal genes (or alleles, in the case of multiple variant forms for a given gene in the population) are located on that copy of the chromosome. Females, however, will primarily express the genes or alleles located on the X-chromosomal copy that remains active. Considering the situation for one gene or multiple genes causing individual differences in a particular phenotype (i.e., causing variation observed in the population for that phenotype), in homozygous females it doesn't particularly matter which copy of the chromosome is inactivated, as the alleles on both copies are the same. However, in females that are heterozygous at the causal genes, the inactivation of one copy of the chromosome over the other can have a direct impact on their phenotypic value. Because of this phenomenon, there is an observed increase in phenotypic variation in females that are heterozygous at the involved gene or genes than in females that are homozygous at that gene or those genes.[21] There are many different ways in which the phenotypic variation can play out. In many cases, heterozygous females may be asymptomatic or only present minor symptoms of a given disorder, such as with X-linked adrenoleukodystrophy.[22]
The differentiation of phenotype in heterozygous females is furthered by the presence of X-inactivation skewing. Typically, each X-chromosome is silenced in half of the cells, but this process is skewed when preferential inactivation of a chromosome occurs. It is thought that skewing happens either by chance or by a physical characteristic of a chromosome that may cause it to be silenced more or less often, such as an unfavorable mutation.[23][24]
On average, each X chromosome is inactivated in half of the cells, although 5-20% of women display X-inactivation skewing.[23] In cases where skewing is present, a broad range of symptom expression can occur, resulting in expression varying from minor to severe depending on the skewing proportion. An extreme case of this was seen where monozygotic female twins had extreme variance in expression of Menkes disease (an X-linked disorder) resulting in the death of one twin while the other remained asymptomatic.[25]
It is thought that X-inactivation skewing could be caused by issues in the mechanism that causes inactivation, or by issues in the chromosome itself.[23][24] However, the link between phenotype and skewing is still being questioned, and should be examined on a case-by-case basis. A study looking at both symptomatic and asymptomatic females who were heterozygous for Duchenne and Becker muscular dystrophies (DMD) found no apparent link between transcript expression and skewed X-Inactivation. The study suggests that both mechanisms are independently regulated, and there are other unknown factors at play.[26]
Chromosomal component
The X-inactivation center (or simply XIC) on the X chromosome is
The XIC contains four non-
Xist and Tsix RNAs
The X-inactive specific transcript (
Prior to inactivation, both X chromosomes weakly express Xist RNA from the Xist gene. During the inactivation process, the future Xa ceases to express Xist, whereas the future Xi dramatically increases Xist RNA production. On the future Xi, the Xist RNA progressively coats the chromosome, spreading out from the XIC;[33] the Xist RNA does not localize to the Xa. The silencing of genes along the Xi occurs soon after coating by Xist RNA.
Like Xist, the
Tsix is a negative regulator of Xist; X chromosomes lacking Tsix expression (and thus having high levels of Xist transcription) are inactivated much more frequently than normal chromosomes.Like Xist, prior to inactivation, both X chromosomes weakly express Tsix RNA from the Tsix gene. Upon the onset of X-inactivation, the future Xi ceases to express Tsix RNA (and increases Xist expression), whereas Xa continues to express Tsix for several days.
Rep A is a long non coding RNA that works with another long non coding RNA, Xist, for X inactivation. Rep A inhibits the function of Tsix, the antisense of Xist, in conjunction with eliminating expression of Xite. It promotes methylation of the Tsix region by attracting PRC2 and thus inactivating one of the X chromosomes.[29]
Silencing
The inactive X chromosome does not express the majority of its genes, unlike the active X chromosome. This is due to the silencing of the Xi by repressive heterochromatin, which compacts the Xi DNA and prevents the expression of most genes.
Compared to the Xa, the Xi has high levels of
Barr bodies
DNA packaged in heterochromatin, such as the Xi, is more condensed than DNA packaged in euchromatin, such as the Xa. The inactive X forms a discrete body within the nucleus called a Barr body.[38] The Barr body is generally located on the periphery of the nucleus, is late replicating within the cell cycle, and, as it contains the Xi, contains heterochromatin modifications and the Xist RNA.
Expressed genes on the inactive X chromosome
A fraction of the genes along the X chromosome escape inactivation on the Xi. The Xist gene is expressed at high levels on the Xi and is not expressed on the Xa.[39] Many other genes escape inactivation; some are expressed equally from the Xa and Xi, and others, while expressed from both chromosomes, are still predominantly expressed from the Xa.[40][41][42] Up to one quarter of genes on the human Xi are capable of escape.[40] Studies in the mouse suggest that in any given cell type, 3% to 15% of genes escape inactivation, and that escaping gene identity varies between tissues.[41][42]
Many of the genes which escape inactivation are present along regions of the X chromosome which, unlike the majority of the X chromosome, contain genes also present on the
The existence of genes along the inactive X which are not silenced explains the defects in humans with abnormal numbers of the X chromosome, such as Turner syndrome (X0, caused by SHOX gene[43]) or Klinefelter syndrome (XXY). Theoretically, X-inactivation should eliminate the differences in gene dosage between affected individuals and individuals with a normal chromosome complement. In affected individuals, however, X-inactivation is incomplete and the dosage of these non-silenced genes will differ as they escape X-inactivation, similar to an autosomal aneuploidy.
The precise mechanisms that control escape from X-inactivation are not known, but silenced and escape regions have been shown to have distinct chromatin marks.[41][44] It has been suggested that escape from X-inactivation might be mediated by expression of long non-coding RNA (lncRNA) within the escaping chromosomal domains.[2]
Uses in experimental biology
Stanley Michael Gartler used X-chromosome inactivation to demonstrate the clonal origin of cancers. Examining normal tissues and tumors from females heterozygous for isoenzymes of the sex-linked G6PD gene demonstrated that tumor cells from such individuals express only one form of G6PD, whereas normal tissues are composed of a nearly equal mixture of cells expressing the two different phenotypes. This pattern suggests that a single cell, and not a population, grows into a cancer.[45] However, this pattern has been proven wrong for many cancer types, suggesting that some cancers may be polyclonal in origin.[46]
Besides, measuring the methylation (inactivation) status of the polymorphic human androgen receptor (HUMARA) located on X-chromosome is considered the most accurate method to assess clonality in female cancer biopsies.[47] A great variety of tumors was tested by this method, some, such as renal cell carcinoma,[48] found monoclonal while others (e.g. mesothelioma[49]) were reported polyclonal.
Researchers have also investigated using X-chromosome inactivation to silence the activity of autosomal chromosomes. For example, Jiang et al. inserted a copy of the Xist gene into one copy of chromosome 21 in
History
In 1959
In 1961,
See also
- Sex-determination system
- Dosage compensation
- Barr body
- Heterochromatin
- Epigenetics
- Skewed X-inactivation
- Developmental disorders thought to be related to X-inactivation:
References
- PMID 15377381.
- ^ PMID 21047393.
- S2CID 4190616.
- ]
- ^ S2CID 26326026.
- ^ S2CID 206552108.
- ^ PMID 23892778.
- PMID 28134930.
- ^ PMID 24733023.
- PMID 29760424.
- PMID 26046443.
- PMID 9445416.
- PMID 26719789.
- PMID 8982455.
- S2CID 39402646.
- ^ Migeon, B (2010). "X chromosome inactivation in human cells". The Biomedical & Life Sciences Collection. Henry Stewart Talks, Ltd: 1–54. Retrieved 15 December 2013.
- ^ a b Gartler SM, Goldman MA (2001). "X-Chromosome Inactivation" (PDF). Encyclopedia of Life Sciences. Nature Publishing Group: 1–2.
- PMID 23637618.
- S2CID 5234164.
- ^ Barakat TS, Gribnau J (2010). "X Chromosome Inactivation and Embryonic Stem Cells". In Meshorer E, Plath K (eds.). The Cell Biology of Stem Cells. Landes Bioscience and Springer Science+Business Media.
- PMID 25880738.
- S2CID 11375978.
- ^ PMID 8651285.
- ^ S2CID 5516967.
- PMID 26239182.
- PMID 22894145.
- ^ S2CID 10899129.
- ^ S2CID 30636065.
- ^ a b Mercer, T.R., Dinger, M.E., Mattick, J.S., (2009). Long non-coding RNAs: insight into functions. Nature Reviews Genetics. (10) 155–159.
- PMID 19036803.
- PMID 17203100.)
Figure 1 Xist RNA encompasses the X from which it is transcribed.
{{cite journal}}: External link in|quote= - S2CID 4329368.
- ^ S2CID 4371247.
- PMID 16285873.
- PMID 28758948.
- S2CID 205001095.
- PMID 10804171.
- S2CID 4093883.
- PMID 12429693.
- ^ S2CID 4358447.
- ^ PMID 23178118.
- ^ PMID 20363980.
- ^ "Turner syndrome: MedlinePlus Genetics". medlineplus.gov. Retrieved 10 February 2023.
- PMID 20573260.
- S2CID 33941451.
- PMID 18614394.
- PMID 17435115.
- S2CID 24870232.
- PMID 25471750.
- PMID 23863942.
- PMID 14428474.
- S2CID 4146768.
- PMID 18156501.
- PMID 13868717.
Further reading
- Huynh KD, Lee JT (May 2005). "X-chromosome inactivation: a hypothesis linking ontogeny and phylogeny". Nature Reviews. Genetics. 6 (5): 410–8. S2CID 19245310.
- Goto T, Monk M (June 1998). "Regulation of X-chromosome inactivation in development in mice and humans" (Review Article). Microbiology and Molecular Biology Reviews. 62 (2): 362–78. PMID 9618446.
- Lyon MF (December 2003). "The Lyon and the LINE hypothesis". Seminars in Cell & Developmental Biology (Review Article). 14 (6): 313–8. PMID 15015738.
- Ng K, Pullirsch D, Leeb M, Wutz A (January 2007). "Xist and the order of silencing" (Review Article). EMBO Reports. 8 (1): 34–9. PMID 17203100.
- Cerase A, Pintacuda G, Tattermusch A, Avner P (August 2015). "Xist localization and function: new insights from multiple levels". Genome Biology. 16 (1): 166. PMID 26282267.
External links
 Media related to X chromosome inactivation at Wikimedia Commons
Media related to X chromosome inactivation at Wikimedia Commons- Kruszelnicki K (11 February 2004). "Hybrid Auto-Immune Women 3". ABC Science.
