Alcohol detoxification
Alcohol detoxification (also known as detox) is the abrupt cessation of
As such, the term "detoxification" may be somewhat of a misnomer since the process need not refer exclusively to the removal of toxic substances from the body. Detoxification may or may not be indicated depending upon an individual's age, medical status, and history of alcohol intake. For example, a young man who binge drinks and seeks treatment one week after his last use of alcohol may not require detoxification before beginning treatment for alcohol use disorder.
Some addiction medicine practitioners use the term "withdrawal management" instead of "detoxification".[2][3]
Withdrawal symptoms
The symptoms of alcohol withdrawal can range from mild to severe depending on the level of alcohol dependence a person has experienced. Symptoms can be behavioural (anxiety, agitation, irritability), neurological (tremor, hallucinations, increased risk of seizures), and physical (changes in heart rate, body temperature, blood pressure, nausea). Symptoms typically occur between 6 and 24 hours since cessation of drinking. In severe cases delirium tremens may occur, which is a medical emergency and could result in death.[4]
Management
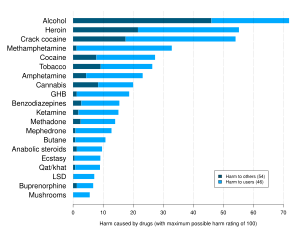
Benzodiazepines are the most common family of drugs used for alcohol detoxification,[5] followed by barbiturates.[6]
Benzodiazepines
Benzodiazepines such as chlordiazepoxide (Librium), diazepam (Valium), lorazepam (Ativan) or oxazepam (Serax) are the most commonly used drugs used to reduce alcohol withdrawal symptoms. There are several treatment patterns in which it is used:[medical citation needed]
- The first option takes into consideration the varying degrees of tolerance. In it, a standard dose of the benzodiazepine is given every half-hour until light sedation is reached. Once a baseline dose is determined, the medication is tapered over the ensuing 3 to 10 days.
- Another option is to give a standard dose of benzodiazepine based on history and adjust based on withdrawal phenomenon.
- A third option is to defer treatment until symptoms occur. This method should not be used in patients with prior, alcohol-related seizures. This has been effective in
Dosing of the benzodiazepines can be guided by the CIWA scale.[10] The scale is available online.[11]
Regarding the choice of benzodiazepine:
- Chlordiazepoxide (Librium) is the benzodiazepine of choice in uncomplicated alcohol withdrawal due to its long half-life.[12]
- Lorazepam or diazepam is available as an injection for patients who cannot safely take medications by mouth.
- Lorazepam and oxazepam are indicated in patients with impaired liver function because they are metabolised outside of the liver.
Nitrous oxide
Other
This section needs additional citations for verification. (January 2024) |

Some hospitals administer alcohol to prevent alcohol withdrawal although there are potential problems with this practice.[18]
Various vitamins, especially from the
Baclofen has been shown in animal studies and in small human studies to enhance detoxification. This drug acts as a GABAB receptor agonist and this may be beneficial.
Phenibut is used in Eastern Europe for alcohol detoxification as it has sedative and anxiolytic effects.
See also
- Drug detoxification
- Detoxification, the process, real or perceived, of removing toxins from the body.
References
- S2CID 5667719.
- ^ "Adult Substance Use Withdrawal Management Services | Texas Health and Human Services".
- ^ "The ASAM Clinical Practice Guideline on Alcohol Withdrawal Management" (PDF). asam.org. 23 January 2020. Retrieved 17 July 2023.
- PMID 15053409.
- at OVID
- S2CID 46899136.
- PMID 8046805.
- PMID 12020181.
- PMID 11444401.
- PMID 2597811.
- PMID 10102003. (see appendix 2)
- ^ Duncan Raistrick; Nick Heather & Christine Godfrey (November 2006). "Review of the Effectiveness of Treatment for Alcohol Problems" (PDF). National Treatment Agency for Substance Misuse, London. Archived from the original (PDF) on 2011-12-03. Retrieved 2011-11-29.
- ^ Gillman M.A, Lichtigfeld, F.J. 2004 Enlarged double-blind randomised trial of benzodiazepines against psychotropic analgesic nitrous oxide for alcohol withdrawal, Addictive Behaviors, Volume 29, Issue 6, Pages 1183–1187
- ^ "South African Brain Institute (SABRI) - profile". S A B R I.
- PMID 2863754.
- PMID 3300587.
- PMID 2653057.
- PMID 12578486.
