Tenosynovial giant cell tumor
| Tenosynovial giant cell tumor | |
|---|---|
| Other names | Localized: Localized pigmented villonodular synovitis (L-PVNS), Giant cell tumor of the tendon sheath (GCT-TS), Nodular tenosynovitis, Localized nodular tenosynovitis, and L-TGCT Diffuse: Pigmented villonodular synovitis (PVNS), Conventional PVNS, and D-TGCT |
CSF1R inhibitors | |
| Medication | Imatinib, Pexidartinib, vimseltinib |
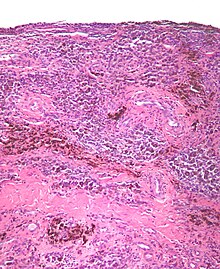
Tenosynovial giant cell tumor (TGCT) is a group of rare, typically non-malignant tumors of the joints. TGCT tumors often develop from the lining of joints (also known as synovial tissue).[1][2][2]: 100 [3][3]: 245 .
Common symptoms of TGCT include swelling, pain, stiffness and reduced mobility in the affected joint or limb.[2]: 102 This group of tumors can be divided into different subsets according to their site, growth pattern, and prognosis.[4][4]: 361 Localized/nodular TGCT is sometimes referred to as giant cell tumor of the tendon sheath;[2]: 100 diffuse TGCT is also called pigmented villonodular synovitis (PVNS).[2]: 102 These two distinct subtypes determined by radiographic appearance.[5] Localized TGCT is defined as a well circumscribed tumor while diffuse TGCT exhibits a locally aggressive and infiltrative behavior.[6]
Classification
Classification for TGCT encompasses two subtypes that can be divided according to site – within a joint (intra-articular) or outside of the joint (extra-articular) – and growth pattern (localized or diffuse) of the tumor(s).[2]: 100 [4]: 361 Localized and diffuse subsets of TGCT differ in their prognosis, clinical presentation, and biological behavior, but share a similar manner of disease development.[2]: 100
Localized TGCT

Localized TGCT is sometimes referred to as localized pigmented villonodular synovitis (L-PVNS), giant cell tumor of the tendon sheath (GCT-TS), nodular tenosynovitis, localized nodular tenosynovitis, and L-TGCT.[1]: 1 [2]: 100
The localized form of TGCT is more common.[2]: 100 [3]: 245 Localized TGCT tumors are typically 0.5 cm-4 cm),[2]: 101 develop over years,[2]: 100 are benign and non-destructive to the surrounding tissue, and may reoccur in the affected area.[2]: 101 The most common symptom is painless swelling.[2]: 101 Localized TGCT most often occurs in fingers, but can also occur in other joints.[2][7]
Diffuse TGCT
Diffuse TGCT is sometimes referred to as pigmented villonodular synovitis (PVNS), conventional PVNS, and D-TGCT.[1]: 1 [4]: 361 [8]: 1 [2]: 102
Diffuse TGCT occurs less frequently and is locally aggressive (in some cases, tumors may infiltrate surrounding soft tissue).[3]: 245 [1]: 1 [2]: 102 [8][8]: 1 It most commonly affects people under 40 years old, though the age of occurrence varies.[2]: 102 Diffuse TGCT may occur inside a joint (intra-articular) or outside of a joint (extra-articular). Intra-articular tumors typically occur in the knee (approximately 75% of cases) and hip (approximately 15% of cases).[2]: 102 Extra-articular tumors are usually found in the knee, thigh, and foot.[2]: 101 Symptoms include swelling, pain, sensitivity, and/or limited range of motion.[2]: 102 The rate of reoccurrence is estimated to be 18-46% for intra-articular tumors and 33-50% for extra-articular tumors.[2]: 103 [8]: 1
Complications
Diffuse TGCT is locally aggressive and can spread to surrounding tissues, causing bone erosion and tissue damage. If not treated early, it can spread to areas outside the joint, extra-articular, and potentially cause permanent loss of range as well as intense pain.[9][10]
Mechanism
TGCT tumors grow due to genetic overexpression of
Diagnosis
TGCT can be diagnosed by magnetic resonance imaging (
To identify or monitor using MRI, the minimum techniques required include T1 weighted images, T2 weighted images, and a fluid sensitive sequence.[23]
Treatment
Patients affected by TGCT should be managed within expert centers or reference networks, by a dedicated, experienced sarcoma multidisciplinary treatment team, including a pathologist, radiologist, orthopaedic surgeon, pain specialist, surgical, radiation and medical oncologists.[24] Patients initially treated at cancer centers have lower recurrence rates than those initially treated by community centers.[25]
Surgery has been the most common form of treatment for both localized[2]: 101 [4]: 361 and diffuse TGCT.[2]: 103 [4]: 361 [8]: 1 After surgery, patients may receive physical therapy in order to help rehabilitate affected joints.[18][10] However, recurrence of TGCT after surgery is common,[16] with a higher rate of recurrence for diffuse TGCT than for localized TGCT.[4]: 361 In cases of recurrent or resistant disease, multiple surgeries, total joint arthroplasties, or amputation may be required.[8]: 1
A multidisciplinary approach, supplementing surgery or other treatments, can also improve outcomes in cases of recurrent TGCT.[26] In the late 2010s, treatment with CSF1R inhibitors emerged as an option[27] that may help improve functionality for patients with recurrent TGCT or TGCT that is not easily managed by surgery.[4]: 361 An oral CSF-1R inhibitor pexidartinib is approved in the US and only available through a Risk Evaluation and Mitigation Strategy (REMS) Program,[28] and two other oral CSF-1R inhibitors, pimicotinib and vimseltinib are being developed in phase 3 trials.[29][30]
There is insufficient and contradictory evidence on radiation therapy, in the form of radiosynoviorthesis (yttrium injections) or external beam, before or after surgery and thus no recommendation for its use in TGCT can be made. [31]
For asymptomatic patients, active surveillance is the preferred method.[32][33] Active surveillance includes monitoring with MRI in intervals (e.g., every 6 months) to ensure the delay in treatment does not pose a potential harm.[34] This should be carefully weighed against the potential for over treatment.
Epidemiology
A study conducted in the Netherlands estimated that the worldwide incidence of TGCT is 43 cases per million
See also
- Fibroma of tendon sheath
- List of cutaneous conditions
References
- ^ PMID 22849738.
- ^ ISBN 9789283224341. Archived from the originalon July 19, 2016.
- ^ PMID 28199932.
- ^ S2CID 1608847.
- PMID 36502615.
- PMID 25465190.
- ^ PMID 28787222.
- ^ PMID 28744388.
- ^ "Clinical Study". The Stone Clinic. Archived from the original (web journal) on 2007-07-01. Retrieved 2007-08-07.
- ^ PMID 25679002.
- PMID 16407111.
The CSF1 translocations result in overexpression of CSF1. In cases of TGCT and PVNS carrying this translocation, it is present in a minority of the intratumoral cells, leading to CSF1 expression only in these cells, whereas the majority of cells express CSF1R but not CSF1, suggesting a tumor-landscaping effect with aberrant CSF1 expression in the neoplastic cells, leading to the abnormal accumulation of nonneoplastic cells that form a tumorous mass.
- S2CID 29544370.
As the CSF1 translocation is postulated to play an important role in the biology of PVNS/TGCT, the consistent presence of CSF1 expression in translocation-negative cases implies that other mechanisms can lead to CSF1 up-regulation.
- PMID 21765227.
- PMID 24917565.
- PMID 10524485. Archived from the originalon 2011-06-06. Retrieved 2020-08-06.
- ^ PMID 28161138.
- PMID 20062758.
- ^ PMID 19047769.
- S2CID 37108679.
- PMID 23185646.
- PMID 26755356.
- PMID 20884045.
- PMID 36502615.
- PMID 36502615.
- PMID 20884045.
- PMID 22733940.
- PMID 28716061.
The tumor-permissive and immunosuppressive characteristics of tumor-associated macrophages (TAM) have fueled interest in therapeutically targeting these cells. In this context, the colony-stimulating factor 1 (CSF1)/colony-stimulating factor 1 receptor (CSF1R) axis has gained the most attention, and various approaches targeting either the ligands or the receptor are currently in clinical development.
- ^ "FDA approves pexidartinib for tenosynovial giant cell tumor". FDA. 20 December 2019.
- ^ "CTG Labs - NCBI".
- ^ "CTG Labs - NCBI".
- PMID 36502615.
- PMID 38215550.
- ISSN 0305-7372.
- PMID 36502615.
