Calcium metabolism

Calcium metabolism is the movement and regulation of
An important aspect of calcium
Body compartment content
Calcium is the most abundant mineral in the human body.[3] The average adult body contains in total approximately 1 kg, 99% in the skeleton in the form of calcium phosphate salts.[3] The extracellular fluid (ECF) contains approximately 22 mmol, of which about 9 mmol is in the plasma.[4] Approximately 10 mmol of calcium is exchanged between bone and the ECF over a period of twenty-four hours.[5]
Blood concentration
The concentration of calcium ions inside cells (in the intracellular fluid) is more than 7,000 times lower than in the blood plasma (i.e. at <0.0002 mmol/L, compared with 1.4 mmol/L in the plasma)
Normal plasma levels
The plasma total calcium concentration is in the range of 2.2–2.6 mmol/L (9–10.5 mg/dL), and the normal ionized calcium is 1.3–1.5 mmol/L (4.5–5.6 mg/dL).
Between 35 and 50% of the calcium in plasma is protein-bound, and 5–10% is in the form of complexes with organic acids and phosphates. The remainder (50–60%) is ionized. The ionized calcium can be determined directly by colorimetry, or it can be read off from nomograms, though the usefulness of the latter is limited when the pH and protein content of the plasma deviate widely from the normal.[4]
Function
Calcium has several main functions in the body.
Bound to serum proteins
It readily binds to proteins, particularly those with amino acids whose side chains terminate in carboxyl (-COOH) groups (e.g. glutamate residues). When such binding occurs the electrical charges on the protein chain change, causing the protein's tertiary structure (i.e. 3-dimensional form) to change. Good examples of this are several of the
Voltage gated sodium channels
The
Intracellular signalling
Because the intracellular calcium ion concentration is extremely low (see above) the entry of minute quantities of calcium ions from the endoplasmic reticulum or from the extracellular fluids, cause rapid, very marked, and readily reversible changes in the relative concentration of these ions in the
Bone
Calcium acts structurally as
Muscle
In
Sources
Not all the calcium in the diet can be readily absorbed from the gut. The calcium that is most readily absorbed is found in dairy products (72%), vegetables (7%), grains (5%), legumes (4%), fruit (3%), protein (3%). The calcium contained in vegetable matter is often complexed with
Bone storage
Calcium flow to and from the bone may be positive, negative, or neutral. When it is neutral, about 5–10 mmol is turned over a day. Bone serves as an important storage point for calcium, as it contains 99% of the total body calcium. Calcium release from bone is regulated by parathyroid hormone in conjunction with calcitriol manufactured in the kidney under the influence of PTH. Calcitonin (a hormone secreted by the thyroid gland when plasma ionized calcium levels are high or rising; not to be confused with "calcitriol" which is manufactured in the kidney) stimulates incorporation of calcium into bone.
Intestinal absorption
The normal adult diet contains about 25 mmol of calcium per day. Only about 5 mmol of this is absorbed into the body per day (see below).[16]
Calcium is absorbed across the intestinal epithelial cell's
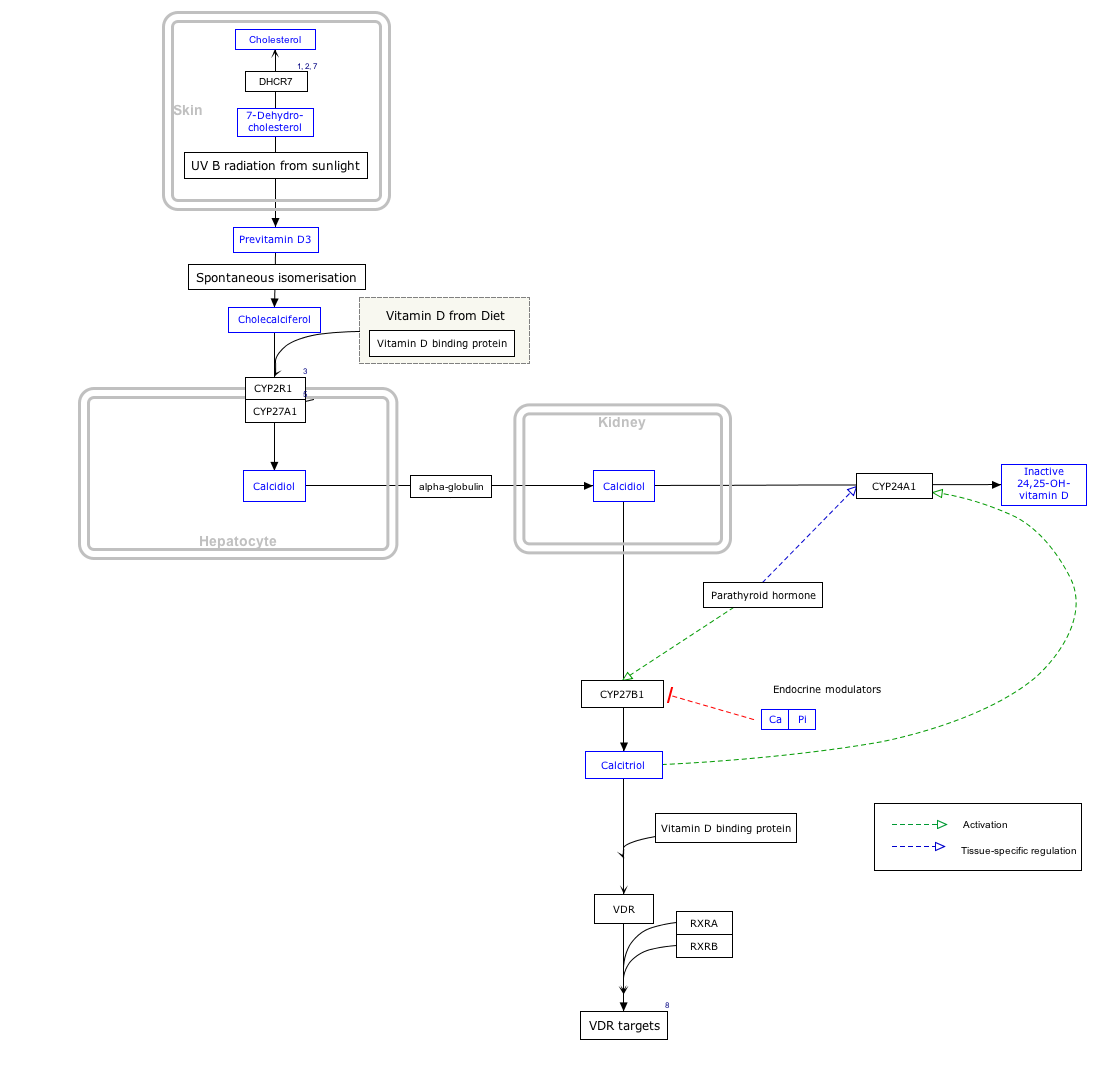
The active absorption of calcium from the gut is regulated by the
Low PTH levels in the blood (which occur under physiological conditions when the plasma ionized calcium levels are high) inhibit the conversion of cholecalciferol into calcitriol, which in turn inhibits calcium absorption from the gut. The opposite happens when the plasma ionized calcium levels are low: parathyroid hormone is secreted into the blood and the kidneys convert more calcifediol into the active calcitriol, increasing calcium absorption from the gut.[24]
Reabsorption
Intestine
Since about 15 mmol of calcium is excreted into the intestine via the bile per day,[4] the total amount of calcium that reaches the duodenum and jejunum each day is about 40 mmol (25 mmol from the diet plus 15 mmol from the bile), of which, on average, 20 mmol is absorbed (back) into the blood. The net result is that about 5 mmol more calcium is absorbed from the gut than is excreted into it via the bile. If there is no active bone building (as in childhood), or increased need for calcium during pregnancy and lactation, the 5 mmol calcium that is absorbed from the gut makes up for urinary losses that are only partially regulated.[16]
Kidneys
The
The kidney influences the plasma ionized calcium concentration in yet another manner. It processes vitamin D3 into calcitriol, the active form that is most effective in promoting the intestinal absorption of calcium. This conversion of vitamin D3 into calcitriol, is also promoted by high plasma parathyroid hormone levels.[24][26]
Excretion
Intestine
Most excretion of excess calcium is via the bile and feces, because the plasma calcitriol levels (which ultimately depend on the plasma calcium levels) regulate how much of the biliary calcium is reabsorbed from the intestinal contents.
Kidneys
Urinary excretion of calcium is normally about 5 mmol (200 mg) /day. This is less in comparison to what is excreted via the feces (15 mmol/day).
Regulation
The plasma ionized calcium concentration is regulated within narrow limits (1.3–1.5 mmol/L). This is achieved by both the
High plasma level
When the concentration of calcium rises, the parafollicular cells of the thyroid gland increase their secretion of calcitonin, a polypeptide hormone, into the blood. At the same time, the parathyroid glands reduce the secretion of parathyroid hormone (PTH), also a polypeptide hormone, into the blood. The resulting high levels of calcitonin in the blood stimulate osteoblasts in bone to remove calcium from blood plasma and deposit it as bone.
The reduced levels of PTH inhibit removal of calcium from the skeleton. The low levels of PTH have several other effects: there is increased loss of calcium in the urine, but more importantly, the loss of phosphate ions through urine is inhibited. Phosphate ions will therefore be retained in the plasma where they form insoluble salts with calcium ions, thereby removing them from the ionized calcium pool in the blood. The low levels of PTH also inhibit the formation of calcitriol (not to be confused with calcitonin) from cholecalciferol (vitamin D3) by the kidneys.
The reduction in the blood calcitriol concentration acts (comparatively slowly) on the epithelial cells (

Low plasma level
When the plasma ionized calcium level is low or falls the opposite happens. Calcitonin secretion is inhibited and PTH secretion is stimulated, resulting in calcium being removed from bone to rapidly correct the plasma calcium level. The high plasma PTH levels inhibit calcium loss via the urine while stimulating the excretion of phosphate ions via that route. They also stimulate the kidneys to manufacture calcitriol (a steroid hormone), which enhances the ability of the cells lining the gut to absorb calcium from the intestinal contents into the blood, by stimulating the production of
Thus fast short term regulation of the plasma ionized calcium level primarily involves rapid movements of calcium into or out of the skeleton. Long term regulation is achieved by regulating the amount of calcium absorbed from the gut or lost via the feces.[2][5][28][29]
Disorders
A diet adequately rich in calcium may reduce calcium loss from bone with advancing (post-
Research
The role that calcium might have in reducing the rates of colorectal cancer has been the subject of many studies. However, given its modest efficacy, there is no current medical recommendation to use calcium for cancer reduction.
See also
Footnotes
- Kidney stonesare therefore often a first indication of hyperparathyroidism, especially since the hypercalcuria is accompanied by an increase in urinary phosphate excretion (a direct result of the high plasma PTH levels). Together the calcium and phosphate tend to precipitate out as water-insoluble salts, which readily form solid “stones”.
References
- ISBN 978-0805349405
- ^ PMID 24470090.
- ^ PMID 20089499.
- ^ ISBN 978-3-9801244-0-9.
- ^ ISBN 978-0-7234-2190-0.
- PMID 10097179.
- ^ a b Harrison TR. Principles of Internal Medicine (third ed.). New York: McGraw-Hill Book Company. pp. 170, 571–579.
- ISBN 978-0-321-98122-6.
- PMID 15173218.
- S2CID 30618615.
- PMID 2519609.
- S2CID 4352361.
- .
- S2CID 86290753.
- PMID 11755039.
- ^ a b Barrett KE, Barman SM, Boitano S, Brooks H, "Chapter 23. Hormonal Control of Calcium & Phosphate Metabolism & the Physiology of Bone" (Chapter). Barrett KE, Barman SM, Boitano S, Brooks H: Ganong's Review of Medical Physiology, 23e: http://www.accessmedicine.com/content.aspx?aID=5244785 Archived 2011-07-07 at the Wayback Machine.
- ^ PMID 17129178.
- )
- PMID 19073913.
- PMID 30770447.
- PMID 19779013.
- ^ "Absorption of Minerals and Metals". www.vivo.colostate.edu. Retrieved 19 April 2018.
- PMID 22460535.
- ^ a b Stryer L. Biochemistry (Fourth Edition). Chapter 27 "Vitamin D is derived from cholesterol by the ring-splitting action of light". New York, W.H. Freeman and Company.
- ^ PMID 25287933.
- ^ Tortora GJ, Anagnostakos NP. Principles of Anatomy and Physiology (Fifth Edition) p. 696. New York, Harper & Row Publishers.
- ISBN 978-1-4160-2328-9.
- ^ ISBN 978-1-4160-2328-9.
- ^ a b c Guyton A (1976). ‘’Medical Physiology’’. p.1062; New York, Saunders and Co.
- S2CID 18794160. Archived from the originalon 2012-08-03.
External links
- Calcium at Lab Tests Online
- Nosek TM. "Section 5/5ch6/5ch6line". Essentials of Human Physiology.[dead link]