Immunoglobulin A

Immunoglobulin A (Ig A, also referred to as sIgA in its secretory form) is an
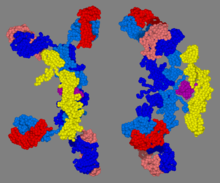
IgA has two subclasses (
Forms
IgA1 vs. IgA2
IgA exists in two
- IgA1 is the predominant IgA subclass found in serum. Most lymphoid tissues have a predominance of IgA1-producing cells.[11]
- In IgA2, the heavy and light chains are not linked with non-covalent bonds. In secretory lymphoid tissues (e.g., gut-associated lymphoid tissue, or GALT), the share of IgA2 production is larger than in the non-secretory lymphoid organs (e.g. spleen, peripheral lymph nodes).
Both IgA1 and IgA2 have been found in external secretions like colostrum, maternal milk, tears and saliva, where IgA2 is more prominent than in the blood.[9] Polysaccharide antigens tend to induce more IgA2 than protein antigens.[10]
Both IgA1 and IgA2 can be in membrane-bound form.[12] (see B-cell receptor)
Serum vs. secretory IgA
It is also possible to distinguish forms of IgA based upon their location – serum IgA vs. secretory IgA.[citation needed]
In secretory IgA, the form found in secretions,
The oligomeric forms of IgA in the external (mucosal) secretions also contain a polypeptide of a much larger molecular mass (70 kD) called the
Physiology
Serum IgA
In the blood, IgA interacts with an
Secretory IgA
The high prevalence of IgA in mucosal areas is a result of a cooperation between
Secretory IgA levels fluctuate diurnally, with the highest levels found in the small intestine and feces around ZT6, the middle of the light period.[15] The regulation of IgA secretion is related to the microbiota, and IgA is known to control specific members of oscillating microbes through direct interactions.[15] However, the underlying cause of the rhythmic secretion of IgA is not completely understood and may differ from one region of the body to another.
Production of sIgA against specific antigens depends on sampling of
sIgA primarily acts by blockading
Clearance of IgA is mediated at least in part by asialoglycoprotein receptors, which recognizes galactose-terminating IgA N-glycans.[8]
Pathology
Genetic
Decreased or absent IgA due to an inherited inability to produce IgA is termed
Anti-IgA antibodies, sometimes present in individuals with low or absent IgA, can result in serious anaphylactic reactions when transfused with blood products that incidentally contain IgA. However, most persons with suspected IgA anaphylactic reactions had experienced acute generalized reactions that were from causes other than anti-IgA transfusion.[18]
Microbial
Neisseria species including Neisseria gonorrhoeae (which causes gonorrhea),[19] Streptococcus pneumoniae,[20] and Haemophilus influenzae type B[21] all release a protease that destroys IgA. Additionally, Blastocystis species have been shown to have several subtypes that generate cysteine and aspartic protease enzymes which degrade human IgA.[22]
Autoimmune and immune-mediated
IgA nephropathy is caused by IgA deposits in the kidneys. The pathogenesis involves the production of hypoglycosylated IgA1, which accumulates and subsequently leads to the formation of immune complexes and the production of IgA-specific IgG, further leading to tissue inflammation.[23]
Henoch–Schönlein purpura (HSP) is a systemic vasculitis caused by deposits of IgA and complement component 3 (C3) in small blood vessels. HSP occurs usually in small children and involves the skin and connective tissues, scrotum, joints, gastrointestinal tract and kidneys. It usually follows an upper respiratory infection and resolves within a couple weeks as the liver clears out the IgA aggregates.[28]
Linear IgA bullous dermatosis and IgA pemphigus are two examples of IgA-mediated immunobullous diseases. IgA-mediated immunobullous diseases can often be difficult to treat even with usually effective medications such as rituximab.[29]
Drug-induced
Vancomycin can induce a linear IgA bullous dermatosis in some patients.[30]
See also
- List of target antigens in pemphigus
- TGF beta
References
- PMID 19079336.
- PMID 19109255.
- S2CID 2586305.
- PMID 15489184.
- S2CID 8445606.
- ISBN 978-0-8385-0590-8.[page needed]
- PMID 15812489.
- ^ PMID 25578468.
- ^ PMID 7118169.
- ^ PMID 16487254.
- PMID 19079156.
- S2CID 26094982.
- ^ PMID 16611558.
- PMID 1924341.
- ^ PMID 36671834.
- ^ PMID 21975936.
- PMID 20101521.
- PMID 7719037.
- PMID 6430698.
- PMID 2117567.
- S2CID 30615746.
- PMID 24883113.
- S2CID 3989355.
- PMID 10702491.
- S2CID 13285781.
- PMID 31297187.
- PMID 10804933.
- PMID 10589705.
- PMID 25901938.
- S2CID 222420540.
External links
- Immunoglobulin+A at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- Herich, R. (2017). "Is the role of IgA in local immunity completely known?". Food and Agricultural Immunology. 28 (2): 223–237. .
