Proteinopathy
| Proteinopathy | |
|---|---|
 | |
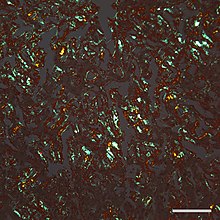
| Micrograph of a section of the cerebral cortex from a person with Alzheimer's disease, immunostained with an antibody to amyloid beta (brown), a protein fragment that accumulates in amyloid plaques and cerebral amyloid angiopathy. 10X microscope objective. |
In
The concept of proteopathy can trace its origins to the mid-19th century, when, in 1854,
Pathophysiology
In most, if not all proteinopathies, a change in the
The likelihood that proteinopathy will develop is increased by certain
It is hypothesized that chaperones and co-chaperones (proteins that assist protein folding) may antagonize proteotoxicity during aging and in protein misfolding-diseases to maintain proteostasis.[27][28][29]
Seeded induction
Some proteins can be induced to form abnormal assemblies by exposure to the same (or similar) protein that has folded into a disease-causing conformation, a process called 'seeding' or 'permissive templating'.
In all of these instances, an aberrant form of the protein itself appears to be the pathogenic agent. In some cases, the deposition of one type of protein can be experimentally induced by aggregated assemblies of other proteins that are rich in β-sheet structure, possibly because of structural complementarity of the protein molecules. For example, AA amyloidosis can be stimulated in mice by such diverse
List of proteinopathies
| Proteinopathy | Major aggregating protein |
| Alzheimer's disease[16] | Amyloid β peptide ( tauopathies )
|
| Cerebral β- amyloid angiopathy[50]
|
Amyloid β peptide ( Aβ )
|
| Retinal ganglion cell degeneration in glaucoma[51] | Amyloid β peptide ( Aβ )
|
Prion diseases (multiple)[52]
|
Prion protein
|
synucleinopathies (multiple)[53]
|
α-Synuclein |
Tauopathies (multiple)[54]
|
Microtubule-associated protein tau (Tau protein) |
FTLD) (Ubi+, Tau-)[55]
|
TDP-43
|
FUS[55]
|
Fused in sarcoma (FUS) protein |
C9ORF72, ubiquilin-2 (UBQLN2 )
| |
| Proteins with tandem glutamine expansions | |
| Familial British dementia[50] | ABri |
| Familial Danish dementia[50] | ADan |
| Hereditary cerebral hemorrhage with amyloidosis (Icelandic) (HCHWA-I)[50]
|
Cystatin C |
| CADASIL[60] | Notch 3
|
| Alexander disease[61] | Glial fibrillary acidic protein (GFAP) |
Pelizaeus-Merzbacher disease
|
proteolipid protein (PLP)
|
| Seipinopathies[62] | Seipin |
| Familial amyloidotic neuropathy, Senile systemic amyloidosis
|
Transthyretin[63] |
| Serpinopathies (multiple)[64] | Serpins
|
| AL (light chain) amyloidosis (primary systemic amyloidosis) | Monoclonal immunoglobulin light chains[63]
|
| AH (heavy chain) amyloidosis | Immunoglobulin heavy chains[63]
|
| AA (secondary) amyloidosis | Amyloid A protein[63] |
Type II diabetes[65]
|
Islet amyloid polypeptide (IAPP; amylin )
|
| Aortic medial amyloidosis | Medin ( lactadherin)[63]
|
ApoAI amyloidosis
|
Apolipoprotein AI[63] |
| ApoAII amyloidosis | Apolipoprotein AII[63] |
| ApoAIV amyloidosis | Apolipoprotein AIV[63] |
| Familial amyloidosis of the Finnish type (FAF) | Gelsolin[63] |
| Lysozyme amyloidosis | Lysozyme[63] |
| Fibrinogen amyloidosis | Fibrinogen[63] |
| Dialysis amyloidosis | Beta-2 microglobulin[63] |
| Inclusion body myositis/myopathy[66] | Amyloid β peptide ( Aβ )
|
Cataracts[67]
|
Crystallins
|
| Retinitis pigmentosa with rhodopsin mutations[68] | rhodopsin |
| Medullary thyroid carcinoma | Calcitonin[63] |
| Cardiac atrial amyloidosis | Atrial natriuretic factor[63]
|
Pituitary prolactinoma
|
Prolactin[63] |
| Hereditary lattice corneal dystrophy | Keratoepithelin[63] |
| Cutaneous lichen amyloidosis[69] | Keratins
|
Mallory bodies[70]
|
Keratin intermediate filament proteins |
| Corneal lactoferrin amyloidosis | Lactoferrin[63] |
| Pulmonary alveolar proteinosis | Surfactant protein C (SP-C)[63] |
| Odontogenic (Pindborg) tumor amyloid | Odontogenic ameloblast-associated protein[63] |
Seminal vesicle amyloid
|
Semenogelin I[63] |
| Apolipoprotein C2 amyloidosis | Apolipoprotein C2 (ApoC2)[63]
|
| Apolipoprotein C3 amyloidosis | Apolipoprotein C3 (ApoC3)[63]
|
Lect2 amyloidosis
|
Leukocyte chemotactic factor-2 (Lect2)[63] |
| Insulin amyloidosis | Insulin[63] |
| Galectin-7 amyloidosis (primary localized cutaneous amyloidosis) | Galectin-7 (Gal7)[63] |
| Corneodesmosin amyloidosis | Corneodesmosin[63] |
| Enfuvirtide amyloidosis[71] | Enfuvirtide[63] |
| Cystic fibrosis[72] | cystic fibrosis transmembrane conductance regulator (CFTR) protein |
| Sickle cell disease[73] | Hemoglobin |
| Plasma cell dyscrasias (monoclonal gammopathies) | gamma globulin |
Exfoliation syndrome[74] aka pseudoexfoliation syndrome
|
aggregated fibrillar material esp. LOXL1 |
Management
The development of effective treatments for many proteopathies has been challenging.
For example, Amyloid A (AA) amyloidosis can be reduced by treating the
Several other treatment strategies for proteopathies are being investigated, including
Additional images
-
Micrograph of tauopathy (brown) in a neuronal cell body (arrow) and process (arrowhead) in the cerebral cortex of a patient with Alzheimer's disease. Bar = 25 microns (0.025mm).
See also
- Amyloidosis
- Neurofibrillary tangles
- Protein toxicity
- Prion
- Transmissible spongiform encephalopathy
References
- ^ S2CID 54314137.
- ^ S2CID 32618330.
- ^ PMID 18295611.
- S2CID 23797549.
- ^ S2CID 39124185.
- S2CID 12480248.
- PMID 28108533.
- PMID 24274755.
- ^ PMID 10940217.
- PMID 9690671.
- S2CID 32899741.
- PMID 21460436.
- PMID 21956718.
- PMID 25416971.
- ^ PMID 10470028.
- ^ PMID 24005412.
- S2CID 6451881.
- PMID 22424229.
- PMID 33308303.
- PMID 27893962.
- S2CID 8993435.
- PMID 21947062.
- PMID 20879875.
- PMID 25904048.
- PMID 22487856.
- PMID 19300591.
- PMID 19421006.
- PMID 25437566.
- PMID 27491084.
- PMID 16042548.
- ^ S2CID 46630402.
- PMID 11357156.
- PMID 15851020.
- PMID 22511864.
- S2CID 27127208.
- PMID 19503072.
- PMID 19651612.
- PMID 21245577.
- PMID 21600984.
- S2CID 11991816.
- PMID 20498711.
- PMID 21321227.
- PMID 19151706.
- PMID 28096245.
- PMID 21454603.
- PMID 15829582.
- PMID 15063745.
- PMID 18055549.
- PMID 20357103.
- ^ PMID 14533778.
- PMID 17684098.
- ISBN 0-87969-693-1.
- S2CID 12590215.
- S2CID 45101893.
- ^ PMID 28100023.
- S2CID 18510138.
- PMID 22918486.
- PMID 17417937.
- PMID 23801983.
- PMID 10712425.
- PMID 17498694.
- PMID 18790819.
- ^ PMID 27884064.
- S2CID 21633779.
- PMID 28159831.
- S2CID 24365234.
- from the original on 2018-07-23. Retrieved 2021-09-15.
- S2CID 38832894.
- S2CID 25820489.
- PMID 15819411.
- PMID 24446896.
- PMID 27734094.
- S2CID 8139305.
- PMID 29547474.
- ^ PMID 16409147.
- ^ PMID 21471435.
- PMID 11260801.
- PMID 12090553.
- PMID 28869766.
- PMID 22785404.
- ^ PMID 30228867.
- PMID 25482846.
- PMID 10827225.
- ^ PMID 26656838.
- PMID 26894299.
- PMID 22939619.
- S2CID 46766370.
- S2CID 49475930.

