Spasmodic torticollis
| Spasmodic torticollis | |
|---|---|
 | |
| Muscles of the neck | |
| Specialty | Neurology |
Spasmodic torticollis is an extremely painful chronic
Signs and symptoms
Initial symptoms of spasmodic torticollis are usually mild. Some feel an invisible tremor of their head for a few months at onset. Then the head may turn, pull or tilt in jerky movements, or sustain a prolonged position involuntarily. Over time, the involuntary spasm of the neck muscles will increase in frequency and strength until it reaches a plateau. Symptoms can also worsen while the patient is walking or during periods of increased stress. Other symptoms include muscle hypertrophy, neck pain, dysarthria and tremor.[2] Studies have shown that over 75% of patients report neck pain,[1] and 33% to 40% experience tremor of the head.[3]
Pathophysiology

The pathophysiology of spasmodic torticollis is still relatively unknown. Spasmodic torticollis is considered neurochemical in nature, and does not result in structural neurodegenerative changes. Although no lesions are present in the
Diagnosis
The most commonly used scale to rate the severity of spasmodic torticollis is the Toronto Western Spasmodic Torticollis Rating Scale (TWSTRS). It has been shown that this rating system has widespread acceptance for use in clinical trials, and has been shown to have “good interobserver reliability.”[8] There are three scales in the TWSTRS: torticollis severity scale, disability scale, and pain scale. These scales are used to represent the severity, the pain, and the general lifestyle of spasmodic torticollis.[citation needed]
Classification
Spasmodic torticollis is a form of focal
Primary
Primary spasmodic torticollis is defined as having no other abnormality other than dystonic movement and occasional tremor in the neck.
Secondary
When other conditions lead to spasmodic torticollis, it is said that the spasmodic torticollis is secondary. A variety of conditions can cause brain injury, from external factors to diseases. These conditions are listed below:[1]
- Central nervous system tumor
- Central pontine myelinolysis
- Cerebrovasculardiseases
- Drug induced
- Infectious or post infectious encephalopathies
- Kernicterus
- Metabolic
- Paraneoplasticsyndromes
- Perinatal (during birth) cerebralinjury
- trauma
- Toxins
Secondary spasmodic torticollis is diagnosed when any of the following are present: history of
Head positions
To further classify spasmodic torticollis, one can note the position of the head.
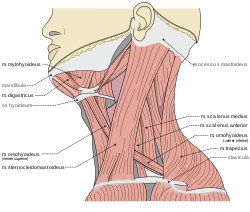
- Torticollis is the horizontal turning (rotational collis) of the head, and uses the contralateral sternocleidomastoidmuscles. This is the "chin-to-shoulder" version.
- Laterocollis is the tilting of the head from side to side. This is the "ear-to-shoulder" version. This involves many more muscles: ipsilateral sternocleidomastoid, ipsilateral splenius, ipsilateral scalene complex, ipsilateral levator scapulae, and ipsilateral posterior paravertebrals.
- The flexion of the neck (head tilts forwards) is anterocollis. This is the "chin-to-chest" version and is the most difficult version to address. This movement utilizes the bilateral sternocleidomastoid, bilateral scalene complex, bilateral submental complex.
- Retrocollis is the extension of the neck (head tilts back) and uses the following muscles for movement: bilateral splenius, bilateral upper trapezius, bilateral deep posterior paravertebrals. This is the "chin-in-the-air" version.
A combination of these head positions is common; many patients experience turning and tilting actions of the head.[10]
Treatment
There are several treatments for spasmodic torticollis, the most commonly used being botulinum toxin injections in the dystonic muscle of the neck. Other treatments include
This suggests that the desynchronization of the frequency range is movement related.[5] Obtaining relief via a "sensory trick", also known as a geste antagoniste, is a common characteristic present in focal dystonias, most prevalently in cervical dystonia; however, it has also been seen in patients with blepharospasm.[11] Sensory tricks offer only temporary and often partial relief of spasmodic torticollis. 74% of patients report only partial relief of spasmodic torticollis compared to 26% reporting complete relief. The sensory trick must also be applied by the patient themselves. When the sensory trick is applied by an examiner, only 32% of patients report relief comparable to relief during self-application.[7] Since the root of the problem is neurological, doctors have explored sensorimotor retraining activities to enable the brain to "rewire" itself and eliminate dystonic movements.[12][13][14][15]
Oral medications
In the past, dopamine blocking agents have been used in the treatment of spasmodic torticollis. Treatment was based on the theory that there is an imbalance of the neurotransmitter dopamine in the basal ganglia. These drugs have fallen out of fashion due to various serious side effects: sedation, parkinsonism, and tardive dyskinesia.[16] Other oral medications can be used in low doses to treat early stages of spasmodic torticollis. Relief from spasmodic torticollis is higher in those patients who take
Higher doses of these medications can be used for later stages of spasmodic torticollis; however, the frequency and severity of side effects associated with the medications are usually not tolerated. Side effects include dry mouth, cognitive disturbance, drowsiness, diplopia, glaucoma and urinary retention.[18]
Botulinum toxin

The most commonly used treatment for spasmodic torticollis is the use of botulinum toxin injection in the dystonic musculature. Botulinum toxin type A is most often used; it prevents the release of
Some patients experience or develop immunoresistance to botulinum toxin type A and must use botulinum toxin type B. Approximately 4% to 17% of patients develop botulinum toxin type A antibodies. The only botulinum toxin type B accessible in the United States is Myobloc. Treatment using botulinum toxin type B is comparable to type A, with an increased frequency of the side effect dry mouth.[10][21]
Common side effects include pain at the injection site (up to 28%),
Deep brain stimulation

Deep brain stimulation to the basal ganglia and thalamus has recently been used as a successful treatment for tremors of patients with Parkinson's disease. This technique is currently, as of 2007, being trialed in patients with spasmodic torticollis. Patients are subjected to stimulation of the globus pallidus internus, or the subthalamic nucleus. The device is analogous to a pacemaker: an external battery is placed subcutaneously, with wires under the skin which enter the skull and a region of the brain. To stimulate the globus pallidus internus, microelectrodes are placed into the globus pallidus internus bilaterally. After the surgery is performed, multiple visits are required to program the settings for the stimulator. The stimulation of the globus pallidus internus disrupts the abnormal discharge pattern in the globus pallidus internus, resulting in inhibition of hyperactive cortical activity. Globus pallidus internus deep brain stimulation is the preferred surgical procedure, due to the lower frequency of side effects.[16] Advantages of deep brain stimulation include the reversibility of the procedure, and the ability to adjust the settings of the stimulation.[17]
In one study, patients who had developed immunoresistance to botulinum toxin underwent globus pallidus internus deep brain stimulation, showing improvement by 54.4% after three to six months.[citation needed]
There is a low rate of side effects for those who undergo deep brain stimulation. The most common side effect is headache, occurring in 15% of patients, followed by infection (4.4%) and cognitive dysfunction (4%). Serious side effects are seizure (1.2%), intracerebral hemorrhage (0.6%), intraventricular
Physical Interventions
Physical treatment options for cervical dystonia include biofeedback, mechanical braces as well as patients self-performing a
Epidemiology
Spasmodic torticollis is one of the most common forms of dystonia seen in neurology clinics, occurring in approximately 0.390% of the United States population in 2007 (390 per 100,000).[3] Worldwide, it has been reported that the incidence rate of spasmodic torticollis is at least 1.2 per 100,000 person years,[27] and a prevalence rate of 57 per 1 million.[28] The exact prevalence of the disorder is not known; several family and population studies show that as many as 25% of cervical dystonia patients have relatives that are undiagnosed.[29][30] Studies have shown that spasmodic torticollis is not diagnosed immediately; many patients are diagnosed well after a year of seeking medical attention.[1] A survey of 59 patients diagnosed with spasmodic torticollis show that 43% of the patients visited at least four physicians before the diagnosis was made.[31]
There is a higher prevalence of spasmodic torticollis in females; females are 1.5 times more likely to develop spasmodic torticollis than males. The prevalence rate of spasmodic torticollis also increases with age, most patients show symptoms from ages 50–69. The average onset age of spasmodic torticollis is 41.[1]
References
- ^ S2CID 28374695.
- ^ "Spasmodic Torticollis – Signs and Symptoms". NSTA. National Spasmodic Torticollis Association. Retrieved December 29, 2018.
- ^ PMID 17442609.
- S2CID 45602523.
- ^ PMID 12785748.
- ^ S2CID 29200547.
- ^ S2CID 3255050.
- PMID 16427167.
- S2CID 53173608.
- ^ .
- S2CID 27142003.
- ^ "Dystonia. Rewiring the brain through movement and dance | Federico Bitti | TEDxNapoli". 13 July 2015 – via www.youtube.com.
- ^ "How your movements can heal your brain | Joaquin Farias | TEDxNapoli". 13 July 2015 – via www.youtube.com.
- ^ Farias J. Limitless. How your movements can heal your brain. An essay on the neurodynamics of dystonia. Galene editions 2016
- ^ Farias J. Intertwined. How to induce neuroplasticity. A new approach to rehabilitate dystonias. Galene editions 2012.
- ^ PMID 18267265.
- ^ PMID 17878433.
- PMID 17355914.
- ^ S2CID 46954613.
- ^ "Botulinum Neurotoxin Injections". Dystonia Medical Research Foundation. 2022-09-28. Retrieved 2022-09-28.
- PMID 24587850.
- PMID 27176573.
- PMID 33180963.
- ^ Silfors, Anders; Göran Solders (2002). "Living with dystonia. A questionnaire among members of the Swedish Dystonia Patient Association". Läkartidningen. 99 (8): 786–789.
- S2CID 16366190.
- S2CID 20722262.
- S2CID 25177370.
- S2CID 26041305.
- S2CID 37961232.
- PMID 9750909.
- S2CID 27554275.
