Tauopathy
| Tauopathies | |
|---|---|
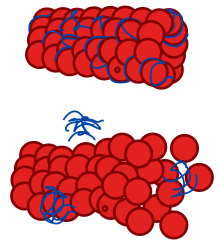 | |
| Diagram of a normal microtubule and one affected by tauopathy | |
| Specialty | Neurology |
Tauopathies are a class of
Tau Protein
Tau protein (also called tubulin associated unit or microtubule-associated protein tau (MAPT)) is a microtubule-associated protein that promotes polymerization and stabilization into microtubules by binding to tubulin. Variants of Tau isoforms, spanning from 352 to 441 amino acids, arise through the alternative splicing of exons 2,3 and 10 within the MAPT gene. The six isoforms are differentiated by the inclusion and exclusion of inserts of either 29 or 58 amino acids in the N-terminus domain. Furthermore, the isoforms are categorized based on the presence of either three (3R tau isoforms) or four (4R tau isoforms) tandem repeat sequences each consisting of 31 or 32 amino acids.[4]
Biomarkers for Tauopathies
Neuroimaging
Positron emission tomography (PET) is one type of biomarker which is capable of identify patient with elevated levels of tau at patient with Alzheimers disease. PET is a great tool which can supplement information such as various regions having higher neuropathologic burden than others. But it needs to be eligible, and more positive outcome than negative, such as exposure to radioactivity.[5]
Biofluid
The analysis of cerebrospinal fluid (CSF) represents a potential avenue for the development of biomarkers in tauopathies. Substantial data on CSF biomarkers is available for Alzheimer's disease (AD), focusing on measures related to total and phosphorylated forms of tau and amyloid-beta (Aβ) protein. Elevated CSF tau and decreased Aβ levels constitute the characteristic CSF signature of AD, allowing differentiation from controls.[6] This signature may also assist in distinguishing atypical forms of AD pathology associated with clinical frontotemporal dementia (FTD) from those with underlying frontotemporal lobar degeneration (FTLD)-Tau pathology[7]
Alzheimer's Disease
Alzheimer's Disease (AD) is clinically characterized by a progressive decline in memory and cognitive functions, leading to severe dementia. Microscopically, AD is identified by the presence of two types of insoluble fibrous materials: (1) extracellular amyloid (Aß) protein forming senile plaques and (2) intracellular neurofibrillary lesions (NFL) composed of abnormally and hyperphosphorylated tau protein. While AD is not strictly considered a prototypical tauopathy, as tau pathology coexists with Aß protein deposition, the 'amyloid cascade hypothesis' posits that Aß accumulation is the primary factor driving AD pathogenesis.[8][9] Nevertheless, AD neurofibrillary lesions were the first to undergo ultrastructural and biochemical analysis, thus laying the foundation for in-depth studies on tau protein deposition in various tauopathies [10]
Neuropathologic Phenotypes
Pick Disease (PiD)
Pick disease (PiD) is a part of a diverse spectrum of disorders clinically marked by dysfunction in the frontal and temporal lobes, collectively referred to as frontotemporal lobar degeneration (FTLD). The primary histological characteristics include profound neuronal loss, enlarged neurons, and distinctive spherical argyrophilic inclusions known as Pick bodies (PBs). These PBs primarily consist of hyperphosphorylated tau protein, with tau protein presenting as two major bands at 60 and 64 kDa and a variable, minor band at 69 kDa. Filamentous tau deposits in nerve cells are predominantly composed of 3R tau isoforms.[11]
Progressive Supranuclear Palsy (PSP)
Progressive Supranuclear Palsy (PSP) is a type of tauopathy, but the cause is not yet discovered. For PSP unusual phosphorylation for tauprotein causes vital protein filaments in the nerve cells to destruct, a phenomenon called "neurofibrillary" degeneration. Typical symptoms of PSP would be abnormal speech, balance impairment and overcognitive and memory impairment. As CBD, PSP is also classified as a 4R tauopathy, and because of that PSP will often be selected for trials regarding anti-tau therapeutics.[12][13]
Corticobasal Degeneration (CBD)
Corticobasal degeneration (CBD) is an increasingly acknowledged neurodegenerative disorder characterized by both motor and cognitive dysfunction. In affected regions, histological examination reveals pronounced neuronal loss accompanied by spongiosis and gliosis, cortical ballooned cells, and notable intracytoplasmic filamentous tau pathology in both glial and neuronal cells. Biochemically, the distinctive tau profile in CBD cases manifests as a prominent tau doublet at 64 and 68 kDa, which is variably identified. These bands predominantly consist of hyperphosphorylated 4R tau isoforms, leading to the classification of CBD as a 4R tauopathy.[14]
Tau Therapeutics
Currently, there are no specific treatments for tauopathies. Up till now, attempts have been made to target neurotransmitter disturbances to relieve disease symptoms. For AD a specific treatment is difficult because the pathological changes both early compared to the symptoms showing.[15] Even though there is no current treatment for tauopathies, there are treatments that can relieve symptoms. Speech therapy can be beneficial for aphasia symptoms, symptoms such as depression and apathy frequently engaged with pharmaceuticals. For physical challenges, physical therapy has proven helpful in extending motor function for patients.[16]
Other diseases
- Primary age-related tauopathy (PART) dementia, with NFTs similar to AD, but without amyloid plaques.[17][18]
- Chronic traumatic encephalopathy (CTE)[19][20]
- Progressive supranuclear palsy (PSP)[21]
- Corticobasal degeneration (CBD)[22]
- Frontotemporal dementia and parkinsonism linked to chromosome 17 (FTDP-17)[23]
- Vacuolar tauopathy[24]
- Lytico-bodig disease (Parkinson-dementia complex of Guam)[25]
- gangliocytoma[26]
- Meningioangiomatosis[27]
- Subacute sclerosing panencephalitis (SSPE)[28]
- As well as lipofuscinosis[29]
See also
- Proteopathy
References
- .
- PMID 28558799.
- .
- .
- PMC 9895127.
- PMC 2696350.
- .
- .
- .
- .
- .
- PMC 7462164.
- ^ "Progressive Supranuclear Palsy - Symptoms, Causes, Treatment | NORD". rarediseases.org.
- .
- PMC 7709159.
- PMC 5476494.
- PMID 22802095.
- S2CID 5655388.
- PMID 26667418.
- S2CID 32662671.
- S2CID 1417930.
- .
- PMID 12142353.
- PMID 33004675.
- S2CID 2821768.
- S2CID 36482221.
- S2CID 663552.
- S2CID 36105401.
- S2CID 25649751.
