Benzodiazepine overdose
| Benzodiazepine overdose | |
|---|---|
| Other names | Benzodiazepine poisoning |
 | |
| US yearly overdose deaths involving benzodiazepines.[1] | |
| Specialty | Toxicology, emergency medicine |
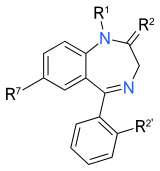
| Benzodiazepines |
|---|
 |
Benzodiazepine overdose (BZD OD) describes the ingestion of one of the drugs in the
Deaths from single-drug benzodiazepine overdoses occur infrequently,
Signs and symptoms
Following an acute overdose of a benzodiazepine the onset of symptoms is typically rapid with most developing symptoms within 4 hours.[12] Patients initially present with mild to moderate impairment of central nervous system function. Initial signs and symptoms include intoxication, somnolence, diplopia, impaired balance, impaired motor function, anterograde amnesia, ataxia, and slurred speech. Most patients with pure benzodiazepine overdose will usually only exhibit these mild CNS symptoms.[12][13] Paradoxical reactions such as anxiety, delirium, combativeness, hallucinations, and aggression can also occur following benzodiazepine overdose.[14] Gastrointestinal symptoms such as nausea and vomiting have also been occasionally reported.[13]
Cases of severe overdose have been reported and symptoms displayed might include prolonged deep coma or deep cyclic coma,
The symptoms of an
Toxicity

Comparability
The various benzodiazepines differ in their toxicity since they produce varying levels of sedation in overdose. A 1993 British study of deaths during the 1980s found flurazepam and temazepam more frequently involved in drug-related deaths, causing more deaths per million prescriptions than other benzodiazepines. Flurazepam, now rarely prescribed in the United Kingdom and Australia, had the highest fatal toxicity index of any benzodiazepine (15.0), followed by temazepam (11.9), versus benzodiazepines overall (5.9), taken with or without alcohol.[36] An Australian (1995) study found oxazepam less toxic and less sedative, and temazepam more toxic and more sedative, than most benzodiazepines in overdose.[11] An Australian study (2004) of overdose admissions between 1987 and 2002 found alprazolam, which happens to be the most prescribed benzodiazepine in Australia and the United States, to be more toxic than diazepam and the other three benzodiazepines which it was compared to (alprazolam, diazepam, oxazepam, chlordiazepoxide, and clonazepam). They also cited a review of the Annual Reports of the American Association of Poison Control Centers National Data Collection System, which showed alprazolam was involved in 34 fatal deliberate self-poisonings over 10 years (1992–2001), compared with 30 fatal deliberate self-poisonings involving diazepam.[37] In a New Zealand study (2003) of 200 deaths, Zopiclone, a benzodiazepine receptor agonist, had similar, although less overdose potential compared to temazepam, which is the most toxic benzodiazepine.[38]
Pathophysiology
Benzodiazepines bind to a specific benzodiazepine receptor, thereby enhancing the effect of the neurotransmitter
Diagnosis
The diagnosis of benzodiazepine overdose may be difficult, but is usually made based on the clinical presentation of the patient along with a history of overdose.
Treatment

Medical observation and supportive care are the mainstay of treatment of benzodiazepine overdose.
Supportive measures
Supportive measures include observation of
Flumazenil
Flumazenil is very effective at reversing the
Epidemiology
In a Swedish (2003) study benzodiazepines were implicated in 39% of
In a Swedish retrospective study of deaths of 1987, in 159 of 1587 autopsy cases benzodiazepines were found. In 44 of these cases the cause of death was
In Australia, a study of 16 deaths associated with toxic concentrations of benzodiazepines during the period of 5 years leading up to July 1994 found preexisting natural disease as a feature of 11 cases; 14 cases were suicides. Cases where other drugs, including ethanol, had contributed to the death were excluded. In the remaining five cases, death was caused solely by benzodiazepines. Nitrazepam and temazepam were the most prevalent drugs detected, followed by oxazepam and flunitrazepam.[57] A review of self poisonings of 12 months 1976 - 1977 in Auckland, New Zealand, found benzodiazepines implicated in 40% of the cases.[58] A 1993 British study found flurazepam and temazepam to have the highest number of deaths per million prescriptions among medications commonly prescribed in the 1980s. Flurazepam, now rarely prescribed in the United Kingdom and Australia, had the highest fatal toxicity index of any benzodiazepine (15.0) followed by Temazepam (11.9), versus 5.9 for benzodiazepines overall, taken with or without alcohol.[36]
Etizolam overdose deaths are rising - for instance, the National Records of Scotland report on drug-related deaths, implicated 548 deaths from 'street' Etizolam in 2018, almost double the number from 2017 (299) and only six years from the first recorded death (in 2012). The 548 deaths were 45% of all drug-related deaths in Scotland in 2018.[59]
References
- ^ a b Overdose Death Rates. By National Institute on Drug Abuse (NIDA).
- ^ S2CID 39966201.
- ISBN 978-0-7817-2845-4.
- ^ S2CID 12787102.
- PMID 26890165.
- ^ Commissioner, Office of the. "Press Announcements - FDA requires strong warnings for opioid analgesics, prescription opioid cough products, and benzodiazepine labeling related to serious risks and death from combined use". www.fda.gov. Retrieved 2017-06-03.
- S2CID 2802139.
- ^ PMID 17306436.
- PMID 10641912.
- S2CID 46001278.
- ^ PMID 7866122.
- ^ PMID 9656979.
- ^ S2CID 27619795.
- PMID 6742700.
- ^ S2CID 45680683.
- ^ PMID 862377.
- PMID 6101526.
- ^ S2CID 7512857.
- PMID 16879940.
- S2CID 37777007.[permanent dead link]
- ^ Wishart, David (2006). "Triazolam". DrugBank. Retrieved 2006-03-23.
- S2CID 796286.
- ^ National Treatment Agency for Substance Misuse (2007). "Drug misuse and dependence - UK guidelines on clinical management" (PDF). United Kingdom: Department of Health. Archived from the original (PDF) on 2012-10-11. Retrieved 2009-11-30.
- PMID 1354907.
- S2CID 10102942.
- S2CID 20125264.
- PMID 28476551.
- PMID 15847621.
- PMID 7663317.
- S2CID 25222287.
- PMID 9153780.
- PMID 8988593.
- PMID 3147739.
- S2CID 11306468.
- S2CID 32066967.
- ^ S2CID 46001278.
- PMID 15206998.
- S2CID 45870330.
- PMID 2461282.
- PMID 6140613.
- PMID 589310.
- S2CID 43105029.
- PMID 40432.
- PMID 2882522.
- ^ ISBN 978-0-7817-2845-4.
- ISBN 978-93-5270-674-7.
Forced diuresis is unlikely to have any benefit in a case of BZD overdose due to high-lipid solubility along with high volume of distribution. Similarly, there is no role of hemodialysis
- ^ S2CID 1055503.
- ^ ISBN 978-0-07-147914-1.
- PMID 1611650.
- PMID 2510872.
- PMID 2569340.
- PMID 7629986.
- ^ ISBN 978-0-07-147914-1.
- PMID 16439763.
- S2CID 24102880.
- PMID 8231567.
- PMID 8947361.
- PMID 31581.
- ^ "Drug-related deaths in Scotland, 2018" (PDF). National Records of Scotland.
