Lenalidomide
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ˌlɛnəˈlɪdoʊmaɪd/ |
| Trade names | Revlimid, Linamide, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a608001 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | Undetermined |
| Protein binding | 30% |
| Metabolism | Undetermined |
| Elimination half-life | 3 hours |
| Excretion | Kidney (67% unchanged) |
| Identifiers | |
| |
JSmol) | |
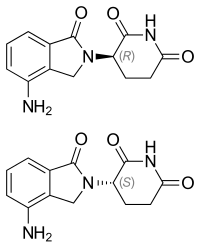
| Chirality | Racemic mixture |
| |
| |
| (verify) | |
Lenalidomide, sold under the brand name Revlimid among others, is a medication used to treat
Common side effects include diarrhea, itchiness, joint pain, fever, headache, and trouble sleeping.
Lenalidomide was approved for medical use in the United States in 2005.[6] It is on the World Health Organization's List of Essential Medicines.[8]
Medical uses
Multiple myeloma
Lenalidomide is used to treat multiple myeloma.[9] It is a more potent molecular analog of thalidomide, which inhibits tumor angiogenesis, tumor-secreted cytokines, and tumor proliferation through induction of apoptosis.[10][11][12]
Lenalidomide is effective at inducing a complete or "very good partial" response and improves
In 2006, lenalidomide received US Food and Drug Administration (FDA) approval for use in combination with dexamethasone in people with multiple myeloma who have received at least one prior therapy.[15] In 2017, the FDA approved lenalidomide as standalone maintenance therapy (without dexamethasone) for people with multiple myeloma following autologous stem cell transplant.[16]
In 2009, The
The use of lenalidomide combined with other drugs was evaluated. It was seen that the drug combinations of lenalidomide plus dexamethasone and continuous bortezomib plus lenalidomide plus dexamethasone probably result in an increase of the overall survival.[18]
Myelodysplastic syndromes
Lenalidomide was approved by the FDA in December 2005, for people with low- or intermediate-1-risk
Mantle cell lymphoma
Lenalidomide is approved by FDA as a
AL amyloidosis
Although not specifically approved by the FDA for use in treating AL amyloidosis, lenalidomide is sometimes used in the treatment of that condition, often in combination with dexamethasone.[23]
Adverse effects
In addition to
Lenalidomide may be associated with adverse effects as second primary
Teratogenicity
Lenalidomide is related to
Venous thromboembolism
Lenalidomide, like its parent compound thalidomide, may cause
Stevens-Johnson syndrome
This section needs to be updated. (April 2020) |
In March 2008, the US Food and Drug Administration (FDA) included lenalidomide on a list of twenty prescription drugs under investigation for potential safety problems. The drug was investigated for possibly increasing the risk of developing Stevens–Johnson syndrome, a life-threatening skin condition.[28]
FDA ongoing safety review
This section needs to be updated. (April 2020) |
In 2011, the FDA initiated an ongoing review of clinical trials that found an increased risk of developing cancers such as
Mechanism of action
Lenalidomide has been used to successfully treat both inflammatory disorders and cancers in the past ten years.[when?] There are multiple mechanisms of action, and they can be simplified by organizing them as mechanisms of action in vitro and in vivo.[31]
On a molecular level, lenalidomide has been shown to interact with the ubiquitin E3 ligase cereblon[32] and target this enzyme to degrade the Ikaros transcription factors IKZF1 and IKZF3.[33]
History
Lenalidomide was approved for medical use in the United States in 2005.[6]
Economics
Lenalidomide costs US$163,381 per year for the average person in the United States as of 2012.[needs update][29] Lenalidomide made almost $9.7bn for Celgene in 2018.[34]
In 2013, the UK National Institute for Health and Care Excellence (NICE) rejected lenalidomide for "use in the treatment of people with a specific type of the bone marrow disorder myelodysplastic syndrome (MDS)" in England and Scotland, arguing that Celgene "did not provide enough evidence to justify the £3,780 per month (US$5,746.73) price-tag of lenalidomide for use in the treatment of people with a specific type of the bone marrow disorder myelodysplastic syndrome (MDS)".[35]
In Australia, a 21-day course of 25 mg lenalidomide tablets costs Medicare A$2397, however the patient only pays $30 due to the Pharmaceutical Benefits Scheme.[36]
References
- ^ a b "Lenalidomide (Revlimid) Use During Pregnancy". Drugs.com. 13 March 2020. Archived from the original on 9 October 2020. Retrieved 13 August 2020.
- FDA. Retrieved 22 October 2023.
- ^ "LENALIDOMIDE VIATRIS (Alphapharm Pty Ltd)". Department of Health and Ages Care. Archived from the original on 13 November 2022. Retrieved 1 April 2023.
- ^ "Lenalidomide Sun/Lenalidomide Rbx/Lenalidomide Ran (Sun Pharma ANZ Pty Ltd)". Department of Health and Ages Care. Archived from the original on 18 March 2023. Retrieved 1 April 2023.
- ^ Anvisa (31 March 2023). "RDC Nº 784 - Listas de Substâncias Entorpecentes, Psicotrópicas, Precursoras e Outras sob Controle Especial" [Collegiate Board Resolution No. 784 - Lists of Narcotic, Psychotropic, Precursor, and Other Substances under Special Control] (in Brazilian Portuguese). Diário Oficial da União (published 4 April 2023). Archived from the original on 3 August 2023. Retrieved 15 August 2023.
- ^ a b c d e f g h i j k "Lenalidomide Monograph for Professionals". Drugs.com. Archived from the original on 4 March 2016. Retrieved 27 October 2019.
- ^ a b c d e "DailyMed - Revlimid- lenalidomide capsule". dailymed.nlm.nih.gov. Archived from the original on 16 February 2020. Retrieved 27 October 2019.
- hdl:10665/371090. WHO/MHP/HPS/EML/2023.02.
- S2CID 1228171.
- ^ S2CID 205547603.
- PMID 21426296.
- PMID 19674465.
- PMID 23691202.
- PMID 22323483.
- ^ "FDA approves lenalidomide oral capsules (Revlimid) for use in combination with dexamethasone in patients with multiple myeloma". U.S. Food and Drug Administration (FDA). 29 June 2006. Archived from the original on 25 November 2011. Retrieved 15 October 2015.
- ^ "Lenalidomide (Revlimid)". U.S. Food and Drug Administration (FDA). 22 February 2017. Archived from the original on 13 August 2020. Retrieved 13 August 2020.
- ^ "REVLIMID Receives Positive Final Appraisal Determination from National Institute for Health and Clinical Excellence (NICE) for Use in the National Health Service (NHS) in England and Wales". Reuters. 23 April 2009. Archived from the original on 24 June 2009.
- PMID 31765002.
- PMID 15703420.
- PMID 16085015.
- PMID 17021321.
- ^ "Revlimid Approved In Europe For Use In Myelodysplastic Syndromes". The MDS Beacon. Archived from the original on 21 September 2015. Retrieved 17 June 2013.
- ^ "Revlimid and Amyloidosis AL" (PDF). MyelomaUK. Archived from the original (PDF) on 27 September 2021. Retrieved 3 October 2020.
- PMID 17724360.
- ^ "Revlimid Summary of Product Characteristics. Annex I" (PDF). European Medicines Agency. 2012. p. 6. Archived (PDF) from the original on 1 March 2014. Retrieved 16 April 2014.
- ^ Ness S (13 March 2014). "New Specialty Drugs". Pharmacy Times. March 2014 Mental Health. 80 (3). Archived from the original on 21 September 2015. Retrieved 5 November 2015.
- PMID 17148721.
- ^ "Potential Signals of Serious Risks/New Safety Information Identified from the Adverse Event Reporting System (AERS) between January - March 2008". U.S. Food and Drug Administration. March 2008. Archived from the original on 19 April 2014. Retrieved 16 December 2019.
- ^ PMID 22571206.
- ^ "FDA Drug Safety Communication: Ongoing safety review of Revlimid (lenalidomide) and possible increased risk of developing new malignancies". U.S. Food and Drug Administration (FDA). April 2011. Archived from the original on 13 August 2020. Retrieved 13 August 2020.
- S2CID 43350339.
- PMID 21860026.
- PMID 24436409.
- ^ "Top 10 Best-Selling Cancer Drugs of 2018". Genetic Engineering and Biotechnology News. 22 April 2019. Archived from the original on 23 April 2019. Retrieved 25 April 2019.
- ^ "Revlimid faces NICE rejection for use in rare blood cancer Watchdog's draft guidance does not recommend Celgene's drug for NHS use in England and Wales". Pharma News. 11 July 2013. Archived from the original on 13 February 2016. Retrieved 5 November 2015.
- ^ Care AG, Pharmaceutical Benefits Scheme (PBS) |, Australian Government Department of Health and Aged Care, archived from the original on 31 March 2023, retrieved 31 March 2023
