Interferon
| Interferon type I (α/β/δ...) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| CDD | cd00095 | ||||||||
| |||||||||
| Interferon type II (γ) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| |||||||||
| Interferon type III (λ) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Identifiers | |||||||||
| Symbol | IL28A | ||||||||
| Pfam | PF15177 | ||||||||
| InterPro | IPR029177 | ||||||||
| CATH | 3og6A00 | ||||||||
| |||||||||
Interferons (IFNs, to heighten their anti-viral defenses.
IFNs belong to the large class of
More than twenty distinct IFN genes and proteins have been identified in animals, including humans. They are typically divided among three classes: Type I IFN, Type II IFN, and Type III IFN. IFNs belonging to all three classes are important for fighting
Types of interferon
Based on the type of receptor through which they signal, human interferons have been classified into three major types.
- macrophages can also produce large amounts of type I interferons when stimulated by viral molecular patterns. The production of type I IFN-α is inhibited by another cytokine known as Interleukin-10. Once released, type I interferons bind to the IFN-α/β receptor on target cells, which leads to expression of proteins that will prevent the virus from producing and replicating its RNA and DNA.[7] Overall, IFN-α can be used to treat hepatitis B and C infections, while IFN-β can be used to treat multiple sclerosis.[3]
- IFNGR2 chains.[3]
In general, type I and II interferons are responsible for regulating and activating the immune response.
Function
All interferons share several common effects: they are antiviral agents and they modulate functions of the immune system. Administration of Type I IFN has been shown experimentally to inhibit tumor growth in animals, but the beneficial action in human tumors has not been widely documented. A virus-infected cell releases viral particles that can infect nearby cells. However, the infected cell can protect neighboring cells against a potential infection of the virus by releasing interferons. In response to interferon, cells produce large amounts of an
Another function of interferons is to up-regulate
Interferons can also suppress angiogenesis by down regulation of angiogenic stimuli deriving from tumor cells. They also suppress the proliferation of endothelial cells. Such suppression causes a decrease in tumor angiogenesis, a decrease in its vascularization and subsequent growth inhibition. Interferons, such as interferon gamma, directly activate other immune cells, such as macrophages and natural killer cells.[17][18][19]
Induction of interferons
Production of interferons occurs mainly in response to microbes, such as viruses and bacteria, and their products. Binding of molecules uniquely found in microbes—viral
Downstream signaling
By interacting with their specific receptors, IFNs activate signal transducer and activator of transcription (STAT) complexes; STATs are a family of transcription factors that regulate the expression of certain immune system genes. Some STATs are activated by both type I and type II IFNs. However each IFN type can also activate unique STATs.[22]
STAT activation initiates the most well-defined cell signaling pathway for all IFNs, the classical
In addition to the JAK-STAT pathway, IFNs can activate several other signaling cascades. For instance, both type I and type II IFNs activate a member of the CRK family of
Interferons can disrupt signaling by other stimuli. For example, interferon alpha induces RIG-G, which disrupts the CSN5-containing COP9 signalosome (CSN), a highly conserved multiprotein complex implicated in protein deneddylation, deubiquitination, and phosphorylation.[24] RIG-G has shown the capacity to inhibit NF-κB and STAT3 signaling in lung cancer cells, which demonstrates the potential of type I IFNs.[citation needed]
Viral resistance to interferons
Many viruses have evolved mechanisms to resist interferon activity.
Ten percent of patients with life-threatening COVID-19 have autoantibodies against type I interferon.[40]
Delayed IFN-I response contributes to the pathogenic inflammation (cytokine storm) seen in later stages of COVID-19 disease.[41] Application of IFN-I prior to (or in the very early stages of) viral infection can be protective,[37] as can treatment with pegylated IFN-λIII,[42] which should be validated in randomized clinical trials.[41]
Interferon therapy
Diseases
Interferon therapy is used (in combination with chemotherapy and radiation) as a treatment for some cancers.
Both
Unconfirmed results suggested that interferon eye drops may be an effective treatment for people who have
When used in systemic therapy, IFNs are mostly administered by an intramuscular injection. The injection of IFNs in the muscle or under the skin is generally well tolerated. The most frequent
Drug formulations
This section needs additional citations for verification. (November 2021) |
| Generic name | Brand name |
|---|---|
| Interferon alfa | Multiferon |
Interferon alpha 2a |
Roferon A |
Interferon alpha 2b |
Intron A/Reliferon/Uniferon |
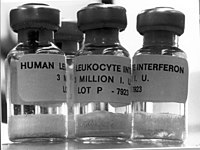
| Human leukocyte Interferon-alpha (HuIFN-alpha-Le) | Multiferon |
Interferon beta 1a , liquid form |
Rebif |
Interferon beta 1a , lyophilized |
Avonex |
Interferon beta 1a , biogeneric (Iran) |
Cinnovex |
Interferon beta 1b |
Betaseron / Betaferon |
Interferon gamma 1b |
Actimmune |
| PEGylated interferon alpha 2a | Pegasys |
| PEGylated interferon alpha 2a (Egypt) | Reiferon Retard |
| PEGylated interferon alpha 2b | PegIntron |
| Ropeginterferon alfa-2b | Besremi |
| PEGylated interferon alpha 2b plus ribavirin (Canada) | Pegetron |
Several different types of interferons are approved for use in humans. One was first approved for medical use in 1986.
There are also interferon-inducing drugs, notably
History
Interferons were first described in 1957 by Alick Isaacs and Jean Lindenmann at the National Institute for Medical Research in London;[65][66][67] the discovery was a result of their studies of viral interference. Viral interference refers to the inhibition of virus growth caused by previous exposure of cells to an active or a heat-inactivated virus. Isaacs and Lindenmann were working with a system that involved the inhibition of the growth of live influenza virus in chicken embryo chorioallantoic membranes by heat-inactivated influenza virus. Their experiments revealed that this interference was mediated by a protein released by cells in the heat-inactivated influenza virus-treated membranes. They published their results in 1957 naming the antiviral factor they had discovered interferon.[66] The findings of Isaacs and Lindenmann have been widely confirmed and corroborated in the literature.[68]
Furthermore, others may have made observations on interferons before the 1957 publication of Isaacs and Lindenmann. For example, during research to produce a more efficient
Interferon was first synthesized manually at
Cantell's and Tan's methods of making large amounts of natural interferon were critical for chemical characterisation, clinical trials and the preparation of small amounts of interferon messenger RNA to clone the human alpha and beta interferon genes. The superinduced human beta interferon messenger RNA was prepared by Tan's lab for Cetus. to clone the human beta interferon gene in bacteria and the recombinant interferon was developed as 'betaseron' and approved for the treatment of MS. Superinduction of the human beta interferon gene was also used by Israeli scientists to manufacture human beta interferon.
Human interferons
Teleost fish interferons
References
- ^ "Interferon | Definition of Interferon by Lexico". Archived from the original on 2020-12-22. Retrieved 2019-10-17.
- S2CID 4523675.
- ^ S2CID 165986.
- PMID 34834923.
- PMID 17502368.
- ^ PMID 15771572.
- PMID 22323926.
- PMID 12946237.
- PMID 20392288.
- ^ Vilcek, Novel interferons, Nature Immunol. 4, 8-9. 2003
- PMID 24751921.
- PMID 28986419.
- S2CID 27209861.
- S2CID 1714991.
- ^ PMID 12872134.
- PMID 16436515.
- ^ PMID 11900986.
- ^ S2CID 20374688.
- ^ PMID 18049472.
- S2CID 28803811.
- PMID 17683972.
- ^ S2CID 1472195.
- PMID 18996892.
- PMID 23415865.
- PMID 20459142.
- ^ PMID 15308723.
- ^ PMID 11544356.
- ^ PMID 11070021.
- PMID 489592.
- PMID 1501278.
- PMID 1350676.
- S2CID 8293109.
- PMID 10390359.
- PMID 11152499.
- PMID 10733410.
- S2CID 72191620.
- ^ PMID 32726355.
- PMID 34571706.
- PMID 32935333.
- ^ PMID 34746804.
- ^ PMID 32464097.
- PMID 36780676.
- PMID 11687131.
- PMID 19707422.
- ^ S2CID 9160289.
- PMID 18236459.
- PMID 15208528.
- PMID 11134916.
- ^ "Genotypes of hepatitis C". Hepatitis C Trust. 2023. Retrieved 8 February 2023.
- PMID 22423262.
- PMID 21449783.
- PMID 21449784.
- PMID 23607594.
- PMID 18985803.
- PMID 19759533.
- S2CID 1707096.
- ^ PMID 25879115.
- PMID 17319959.
- ISBN 978-1437727029. Archivedfrom the original on 2019-12-29. Retrieved 2017-09-01.
- PMID 19034963.
- PMID 14768714.
- PMID 11990646.
- PMID 4670490.
- PMID 29133569.
- ^ Kolata, Gina (2015-01-22). "Jean Lindenmann, Who Made Interferon His Life's Work, Is Dead at 90". The New York Times. Archived from the original on 2019-12-27. Retrieved 2015-02-12.
- ^ S2CID 202574492.
- ^ PMID 17502369.
- ISBN 978-3-7091-3432-0.
- PMID 14364998.
- PMID 16590396.
- PMID 4346649.
- S2CID 4287343.
- S2CID 4315307.
- PMID 678325.
- PMID 670186.
- ^ PMID 468807.
- PMID 7352260.
- PMID 6157401.
- PMID 7352259.
- PMID 6164058.
- PMID 6159625.
- S2CID 29500779.
- S2CID 4275528.
- S2CID 4310807.
- ^ US patent 6207146, Tan YH, Hong WJ, "Gene expression in mammalian cells.", issued 2001
- ISBN 978-981-02-3148-4.
- PMID 5272327.
- ^ US patent 3773924, Ho M, Armstrong JA, Ke YH, Tan YH, "Interferon Production", issued 1973
- S2CID 84918367.
- S2CID 3455413.
- PMID 27827855.
Further reading
- Taylor, Milton W. (2014). "Interferons". Viruses and Man: A History of Interactions. pp. 101–119. PMC 7123835.
External links
 Media related to Interferons at Wikimedia Commons
Media related to Interferons at Wikimedia Commons
