Meconium aspiration syndrome
| Meconium aspiration syndrome | |
|---|---|
| Other names | Neonatal aspiration of meconium |
 | |
| X-ray showing the extent of lung epithelial damage in response to meconium seen in neonates with meconium aspiration syndrome. | |
| Specialty | Neonatology |
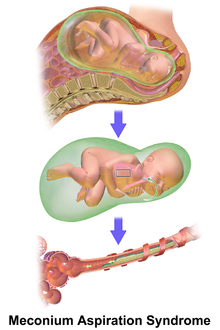
Meconium aspiration syndrome (MAS) also known as neonatal aspiration of meconium is a medical condition affecting newborn infants. It describes the spectrum of disorders and pathophysiology of newborns born in meconium-stained amniotic fluid (MSAF) and have meconium within their lungs. Therefore, MAS has a wide range of severity depending on what conditions and complications develop after parturition. Furthermore, the pathophysiology of MAS is multifactorial and extremely complex which is why it is the leading cause of morbidity and mortality in term infants.[1][2]
The word meconium is derived from the Greek word mēkōnion meaning juice from the opium poppy as the sedative effects it had on the foetus were observed by Aristotle.[3]
Meconium is a sticky dark-green substance which contains gastrointestinal secretions, amniotic fluid, bile acids, bile, blood, mucus, cholesterol, pancreatic secretions, lanugo, vernix caseosa and cellular debris.[1] Meconium accumulates in the foetal gastrointestinal tract throughout the third trimester of pregnancy and it is the first intestinal discharge released within the first 48 hours after birth.[4] Notably, since meconium and the whole content of the gastrointestinal tract is located 'extracorporeally,' its constituents are hidden and normally not recognised by the foetal immune system.[5]
For the meconium within the amniotic fluid to successfully cause MAS, it has to enter the respiratory system during the period when the fluid-filled lungs transition into an air-filled organ capable of gas exchange.[1]
Causes
The main theories of meconium passage into amniotic fluid are caused by fetal maturity or from foetal stress as a result of
Meconium passage as a result of foetal distress
There may be an important association between foetal distress and
Foetal hypoxic stress during parturition can stimulate colonic activity, by enhancing intestinal
The association between foetal distress and meconium passage is not a definite cause-effect relationship as over 3⁄4 of infants with MSAF are vigorous at birth and do not have any distress or hypoxia.[2] Additionally, foetal distress occurs frequently without the passage of meconium as well.[3]
Meconium passage as a result of foetal maturity
Although meconium is present in the gastrointestinal tract early in development, MSAF rarely occurs before 34 weeks gestation.[3]
Pathophysiology
As MAS describes a spectrum of disorders of newborns born through MSAF, without any congenital respiratory disorders or other underlying pathology, there are numerous hypothesised mechanisms and causes for the onset of this syndrome. Long-term consequences may arise from these disorders, for example, infants that develop MAS have higher rates of developing neurodevelopmental defects due to poor respiration.[9]
Airway obstruction
In the first 15 minutes of meconium aspiration, there is obstruction of larger airways which causes increased lung resistance, decreased lung compliance, acute hypoxemia, hypercapnia, atelectasis and respiratory acidosis. After 60 minutes of exposure, the meconium travels further down into the smaller airways. Once within the terminal bronchioles and alveoli, the meconium triggers inflammation, pulmonary edema, vasoconstriction, bronchoconstriction, collapse of airways and inactivation of surfactant.[10][11]
Foetal hypoxia
The lung areas which do not or only partially participate in
Infection
Microorganisms, most commonly
Pulmonary inflammation
Meconium has a complex chemical composition, so it is difficult to identify a single agent responsible for the several diseases that arise. As meconium is stored inside the
Meconium is a source of pro-inflammatory
Meconium contains high amounts of
Surfactant inactivation
The extent of surfactant inhibition depends on both the concentration of surfactant and meconium. If the surfactant concentration is low, even very highly diluted meconium can inhibit surfactant function whereas, in high surfactant concentrations, the effects of meconium are limited. Meconium may impact surfactant mechanisms by preventing surfactant from spreading over the alveolar surface, decreasing the concentration of surfactant proteins (SP-A and SP-B), and by changing the viscosity and structure of surfactant.[10] Several morphological changes occur after meconium exposure, the most notable being the detachment of airway epithelium from stroma and the shedding of epithelial cells into the airway. These indicate a direct detrimental effect on lung alveolar cells because of the introduction of meconium into the lungs.[1]
Persistent Pulmonary Hypertension
Apoptosis
Apoptosis is an important mechanism in the clearance of injured cells and in tissue repair, however too much apoptosis may cause harm, such as acute lung injury. Meconium induces apoptosis and DNA cleavage of lung airway epithelial cells, this is detected by the presence of fragmented DNA within the airways and in alveolar epithelial nuclei. Meconium induces an inflammatory reaction within the lungs as there is an increase of autophagocytic cells and levels of caspase 3 after exposure. After 8 hours of meconium exposure, in rabbit foetuses, the total amount of apoptotic cells is 54%.[15] Therefore, the majority of meconium-induced lung damage may be due to the apoptosis of lung epithelium.[1]
Diagnosis
Respiratory distress in an infant born through the darkly coloured MSAF as well as meconium obstructing the airways is usually sufficient enough to diagnose MAS. Additionally, newborns with MAS can have other types of respiratory distress such as tachypnea and hypercapnia. Sometimes it is hard to diagnose MAS as it can be confused with other diseases that also cause respiratory distress, such as pneumonia. Additionally, X-rays and lung ultrasounds can be quick, easy and cheap imaging techniques to diagnose lung diseases like MAS.[16]
Prevention
In general, the incidence of MAS has been significantly reduced over the past two decades as the number of post-term deliveries has minimized.[17]
Prevention during pregnancy
Prevention during pregnancy may include amnioinfusion and antibiotics but the effectiveness of these treatments are questionable.[2]
Prevention during parturition
As previously mentioned,
Treatment
Most infants born through MSAF do not require any treatments (other than routine postnatal care) as they show no signs of respiratory distress, as only approximately 5% of infants born through MSAF develop MAS.[1] However, infants which do develop MAS need to be admitted to a neonatal unit where they will be closely observed and provided any treatments needed. Observations include monitoring heart rate, respiratory rate, oxygen saturation and blood glucose (to detect worsening respiratory acidosis or the development of hypoglycemia).[18] In general, treatment of MAS is more supportive in nature.
Assisted ventilation techniques
To clear the airways of meconium, tracheal suctioning can be used however, the efficacy of this method is in question and it can cause harm.[19]
In cases of MAS, there is a need for supplemental oxygen for at least 12 hours in order to maintain oxygen saturation of haemoglobin at 92% or more. The severity of respiratory distress can vary significantly between newborns with MAS, as some require minimal or no supplemental oxygen requirement and, in severe cases, mechanical ventilation may be needed.
Ventilation of infants with MAS can be challenging and, as MAS can affect each individual differently, ventilation administration may need to be customised. Some newborns with MAS can have homogenous lung changes and others can have inconsistent and patchy changes to their lungs. It is common for sedation and muscle relaxants to be used to optimise ventilation and minimise the risk of pneumothorax associated with dyssynchronous breathing.[18]
Inhaled nitric oxide
Inhaled
Antiinflammatories
As inflammation is such a huge issue in MAS, treatment has consisted of anti-inflammatories.
Glucocorticoids
Glucocorticoids have a strong anti-inflammatory activity and works to reduce the migration and activation of neutrophils, eosinophils, mononuclear cells, and other cells. They reduce the migration of neutrophils into the lungs ergo, decreasing their adherence to the endothelium. Thus, there is a reduction in the action of mediators released from these cells and therefore, a reduced inflammatory response.[22][11]
Glucocorticoids also possess a genomic mechanism of action in which, once bound to a glucocorticoid receptor, the activated complex moves into the nucleus and inhibits transcription of mRNA. Ultimately, effecting whether various proteins get produced or not. Inhibiting the transcription of nuclear factor (NF-κB) and protein activator (AP-1) attenuates the expression of pro-inflammatory cytokines (IL-1, IL-6, IL-8 and TNF etc.), enzymes (PLA2, COX-2, iNOs etc.) and other biologically active substances.[23][22][11] The anti-inflammatory effect of glucocorticoids is also demonstrated by enhancing the activity of lipocortines which inhibit the activity of PLA2 and therefore, decrease the production of arachidonic acid and mediators of lipoxygenase and cyclooxygenase pathways.[22]
Inhibitors of phosphodiesterase
Inhibitors of cyclooxygenase
Antibiotics
Meconium is typically sterile however, it can contain various cultures of bacteria so appropriate antibiotics may need to be prescribed.[17]
Surfactant treatment
Previous treatments
Originally, it was believed that MAS developed as a result of the meconium being a physical blockage of the airways. Thus, to prevent newborns, who were born through MSAF, from developing MAS, suctioning of the
Historically, amnioinfusion has been used when MSAF was present, which involves a transcervical infusion of fluid during labour. The idea was to dilute the thick meconium to reduce its potential pathophysiology and reduce cases of MAS, since MAS is more prevalent in cases of thick meconium.[2] However, there are associated risks, such as umbilical cord prolapse and prolongation of labour. The UK National Institute of Health and Clinical Excellence (NICE) Guidelines recommend against the use of amnioinfusion in women with MSAF.[18]
Prevalence
1 in every 7 pregnancies have MSAF and, of these cases, approximately 5% of these infants develop MAS.[1] MSAF is observed 23-52% in pregnancies at 42 weeks therefore, the frequency of MAS increases as the length of gestation increases, such that the prevalence is greatest in post-term pregnancies. Conversely, preterm births are not frequently associated with MSAF (only approximately 5% in total contain MSAF). The rate of MAS declines in populations where labour is induced in women that have pregnancies exceeding 41 weeks.[4] There are many suspected pre-disposing factors that are thought to increase the risk of MAS. For example, the risk of MSAF is higher in African American, African and Pacific Islander mothers, compared to mothers from other ethnic groups.[27][6]
Future research
Research is being focused on developing both a successful method for preventing MAS as well as an effective treatment. For example, investigations are being made in the efficiency of
See also
References
- ^ PMID 19833459.
- ^ PMID 28411000.
- ^ .
- ^ .
- ^ PMID 25721501.
- ^ PMID 22164183.
- ^ PMID 19057607.
- PMID 19836908.
- PMID 19057618.
- ^ S2CID 20533996.
- ^ S2CID 41008280.
- PMID 24028637.
- S2CID 46969843.
- .
- PMID 15698862.
- PMID 25220126.
- ^ S2CID 4723566.
- ^ .
- ^ PMID 21277716.
- S2CID 29268118.
- PMID 19057615.
- ^ PMID 21465122.
- ^ S2CID 24458998.
- S2CID 38587541.
- PMID 22067375.
- PMID 984149.
- PMID 10879341.
