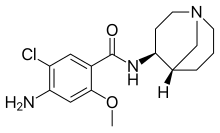
Renzapride
 | |
| Clinical data | |
|---|---|
| ATC code |
|
| Identifiers | |
| |
JSmol) | |
| |
| |
| | |
Renzapride is a
Renzapride was being developed by Alizyme plc of the United Kingdom. In May 2016, EndoLogic LLC, a US-based pharmaceutical and medical device company, acquired the US and worldwide patent rights to Renzapride.
Endologic confirmed the cardiac safety of renzapride through a “Thorough QTc” study [3] and sold the rights to Atlantic Healthcare plc in 2019,[4] a specialist pharmaceutical company.
Atlantic Healthcare is focusing on the development of renzapride for the management of gastrointestinal (GI) motility in a number of rare diseases, including systemic scleroderma and cystic fibrosis, both of which are associated with chronic GI motility problems and for which there are no approved therapies.
Clinical trials
In nine diabetic patients with autonomic neuropathy, renzapride reduced the mean lag phase of gastric emptying by 20–26 min at all doses (P < 0.01) [5]
In Phase 2a studies on subjects with constipation Renzapride was shown to accelerate colonic transit (p=0.016 vs placebo P=0.009) (Ref: ATL 1251/001/CL) as well as increase daily stool frequency (p<0.005) (Ref: ATL 1251/025/CL)
Renzapride has been assessed in Phase II clinical trials with a total of 578 patients with constipation-predominant irritable bowel syndrome (IBS-C). As compared with placebo, the treatment groups reported better relief of their overall symptoms, namely abdominal pain and discomfort, increase in the number of pain free days, improved stool frequency, consistency and ease of passage of bowel movements. There were no significant differences in the reported Serious Adverse Events between treatment and placebo groups.[2][6][7]
In the largest of these Phase II trials, 510 subjects with IBS-C received either 1, 2 or 4 mg QD renzapride, or placebo QD for 12 weeks. The Weekly responder rate based on subject's assessment of whether they had relief from abdominal pain and/or discomfort associated with IBS during weeks 5-12 was 56% (renzapride 4 mg) vs 49% (placebo). For females the treatment effect was larger, 61% (renzapride 4 mg) vs 49% (placebo). Statistically significant effects in favour of renzapride were observed for improvements in stool consistency and increased bowel movements.[7]
In the Phase III clinical trial in IBS-C, 1798 female patients received either 2 or 4 mg Renzapride, or placebo once daily, for 12 weeks. The mean number of months with relief of overall symptoms was 0.6, 0.55 and 0.44 for renzapride 2 mg twice a day, renzapride 4 mg once a day and placebo, respectively, with both renzapride doses being statistically superior to placebo (p=0.004 and p=0.027, respectively). On responder analysis, the proportion of responders was 33.2%, 29.8%, and 24.3% for renzapride 2 mg twice a day, renzapride 4 mg once a day and placebo, respectively.[8]
The 8.9% delta between renzapride 2 mg twice daily and placebo compares favourably with other FDA approved therapies (Ford [9]).
References
- ^ PMID 18095752.
- ^ PMID 15476153.
- ^ "FDA accepts cardiac safety trial for gastroparesis drug". Healio. 21 May 2018.
- ^ Quested T (26 June 2019). "Atlantic Healthcare pounces on big bucks US opportunity". Business Weekly.
- S2CID 20428833.
- S2CID 25481560.
- ^ S2CID 38167889.
- PMID 20163375.
- S2CID 28565520.
