IPEX syndrome
| IPEX syndrome | |
|---|---|
| Other names | Autoimmune enteropathy type 1[1] |
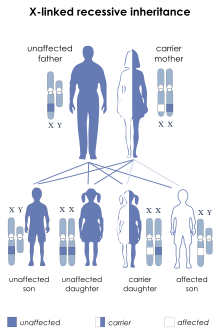 | |
| IPEX syndrome is inherited via X-linked recessive | |
| Specialty | Immunology |
| Symptoms | Lymphadenopathy[2] |
| Causes | FOXP3 gene mutation[1] |
| Diagnostic method | Family history, Genetic test[1] |
| Treatment | TPN(nutritional purpose), Cyclosporin A and FK506, Bone marrow transplant[3][4] |
Immunodysregulation polyendocrinopathy enteropathy X-linked syndrome (IPEX syndrome) is a rare
IPEX is caused by mutations in the gene FOXP3, which encodes transcription factor forkhead box P3 (
IPEX onset usually happens in
Presentation
Classical triad
The classical triad describes the most common symptoms of IPEX: intractable
Other symptoms include: thyroid disease, kidney dysfunction, blood disorders, frequent infections, autoimmune hemolytic anemia, and food allergies, among others.[10]
Endocrinopathy
The most common
Thyroid disorders are also common.[14]
Enteropathy
The most common enteropathy associated with IPEX is intractable diarrhea. Vomiting and gastritis are also common. Other manifestations include Celiac disease, ulcerative colitis, and ileus.[14]

Skin manifestations
The most common form of skin involvement is
Early life
IPEX patients are usually born with normal weight and length at term. Nevertheless, the first symptoms may present in the first days of life,[15] and some reported cases labeled newborns with intrauterine growth restriction and evidence of meconium in the amniotic fluid.[16]
Genetics

FOXP3 gene
IPEX syndrome is inherited in males in an
FOXP3 mutations
A large variety of
FOXP3 pathways
FOXP3 can function as both a
Diagnosis
Early detection of the disease is crucial because IPEX has a high mortality level if left untreated.[20] IPEX is usually diagnosed based on the following criteria:[1][4]
- Clinical triad
- Family history
- IgE, eosinophilia, autoimmune anemia and decreased number of FOXP3 Treg cells.
- Genetic testing: single-gene testing and multigene panel.
Treatment

Individuals with IPEX will usually need supportive care in a hospital. Most common is nutritional treatment for enteropathy and insulin therapy for T1D. IPEX treatment tends to focus on managing symptoms, reducing autoimmunity, and/or treating secondary conditions. Usually, treatment will involve immunosuppression.[11]
Drugs used include:
- Cyclosporin A
- Tacrolimus
- Sirolimus
- Rituximab
Currently, the standard treatment for IPEX is a bone marrow transplant. If donor-recipient chimerism is achieved, individuals with IPEX can achieve complete remission.[11]
Research
In 1982, Powel et al. published a case report of a family with 19 males who were affected by an X-linked syndrome with symptoms including polyendocrinopathy and diarrhea. The most common symptoms in this family were severe enteropathy, T1D, and dermatitis. Only 2 of the 19 affected males in the family survived past 3 years old. These individuals lived to 10 and 30 years old.[21] Powel's study is now widely considered the first documentation of IPEX.[citation needed]
Scurfy mouse
Scurfy is a type of model mouse used for immunology research. Scurfy mice have had 2 base pairs inserted within the FOXP3 gene. This leads to a frameshift mutation in FOXP3 gene and the expressed protein is truncated, causing functional deficiency of Treg cells. Then, autoreactive CD4+T cells and inflammatory cells cause tissue damage.[22] Scurfy mice have an enlarged spleen and lymph nodes, squinted red eyes, and scaly or "ruffled" skin. The mice also have immunity problems and tend to die approximately 3 weeks after birth.[18] From 2000 - 2001, multiple studies confirmed that IPEX is the human equivalent of scurfy mice and that the FOXP3 gene is responsible.[10]
See also
References
- ^ a b c d e "Orphanet: Immune dysregulation polyendocrinopathy enteropathy X linked syndrome". www.orpha.net. Retrieved 2017-04-18.
- ^ a b "Immunodysregulation, polyendocrinopathy and enteropathy X-linked | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Archived from the original on 2019-01-09. Retrieved 2017-04-16.
- ISBN 9781603274784.
- ^ PMID 20301297.update 2011
- ^ "Embase". www.embase.com. Retrieved 2023-04-04.
- ^ a b "IPEX syndrome". Genetics Home Reference. Retrieved 2017-04-16.
- ^ a b "FOXP3 gene". Genetics Home Reference. Retrieved 2017-04-16.
- ^ S2CID 211231953.
- S2CID 11149833.
- ^ S2CID 11149833.
- ^ PMID 33668198.
- S2CID 214768010.
- ^ CDC (2022-03-11). "What Is Type 1 Diabetes?". Centers for Disease Control and Prevention. Retrieved 2023-04-16.
- ^ S2CID 214768010.
- PMID 23060872.
- PMID 25546394.
- ^ PMID 26918796.
- ^ PMID 26918796.
- ^ S2CID 20395564.
- ^ S2CID 208377306, retrieved 2021-01-29
- PMID 7040622.
- PMID 31068947.
Further reading
- Bacchetta R, Barzaghi F, Roncarolo MG (April 2018). "From IPEX syndrome to FOXP3 mutation: a lesson on immune dysregulation". Annals of the New York Academy of Sciences. 1417 (1): 5–22. PMID 26918796.
- Barzaghi F, Passerini L, Bacchetta R (1 January 2012). "Immune dysregulation, polyendocrinopathy, enteropathy, x-linked syndrome: a paradigm of immunodeficiency with autoimmunity". Frontiers in Immunology. 3: 211. PMID 23060872.
- Elzouki AY, Harfi HA, Nazer H, Stapleton FB, Oh W, Whitley RJ (2012-01-10). Textbook of Clinical Pediatrics. Springer Science & Business Media. ISBN 9783642022029.
