Ulcerative colitis
| Ulcerative colitis | |
|---|---|
| Frequency | 2–299 per 100,000[5] |
| Deaths | 47,400 together with Crohn's (2015)[6] |
Ulcerative colitis (UC) is one of the two types of
The cause of UC is unknown.
Dietary changes, such as maintaining a high-calorie diet or
Signs and symptoms
| Crohn's disease | Ulcerative colitis | |
|---|---|---|
| Defecation | Often porridge-like,[10] sometimes steatorrhea |
Often mucus-like and with blood[10] |
| Tenesmus | Less common[10] | More common[10] |
| Fever | Common[10] | Indicates severe disease[10] |
| Fistulae | Common[11] | Seldom |
| Weight loss | Often | More seldom |
Gastrointestinal
People with ulcerative colitis usually present with diarrhea mixed with blood,[12] of gradual onset that persists for an extended period of time (weeks). It is estimated that 90% of people experience rectal bleeding (of varying severity), 90% experience watery or loose stools with increased stool frequency (diarrhea), and 75-90% of people experience bowel urgency.[13] Additional symptoms may include fecal incontinence, mucous rectal discharge, and nocturnal defecations.[12] With proctitis (inflammation of the rectum), people with UC may experience urgency or rectal tenesmus, which is the urgent desire to evacuate the bowels but with the passage of little stool.[12] Tenesmus may be misinterpreted as constipation, due to the urge to defecate despite small volume of stool passage. Bloody diarrhea and abdominal pain may be more prominent features in severe disease.[12] The severity of abdominal pain with UC varies from mild discomfort to very painful bowel movements and abdominal cramping.[14] High frequency of bowel movements, weight loss, nausea, fatigue, and fever are also common during disease flares. Chronic bleeding from the GI tract, chronic inflammation, and iron deficiency often leads to anemia, which can affect quality of life.[15]
The clinical presentation of ulcerative colitis depends on the extent of the disease process.[16] Up to 15% of individuals may have severe disease upon initial onset of symptoms.[12] A substantial proportion (up to 45%) of people with a history of UC without any ongoing symptoms (clinical remission) have objective evidence of ongoing inflammation.[17] Ulcerative colitis is associated with a generalized inflammatory process that can affect many parts of the body. Sometimes, these associated extra-intestinal symptoms are the initial signs of the disease.[18]
Extent of involvement


In contrast to Crohn's disease, which can affect areas of the gastrointestinal tract outside of the colon, ulcerative colitis is usually confined to the colon. Inflammation in ulcerative colitis is usually continuous, typically involving the rectum, with involvement extending proximally (to sigmoid colon, ascending colon, etc.).[19] In contrast, inflammation with Crohn's disease is often patchy, with so-called "skip lesions" (intermittent regions of inflamed bowel).[20]
The disease is classified by the extent of involvement, depending on how far the disease extends:[14] proctitis (rectal inflammation), left sided colitis (inflammation extending to descending colon), and extensive colitis (inflammation proximal to the descending colon).[19] Proctosigmoiditis describes inflammation of the rectum and sigmoid colon. Pancolitis describes involvement of the entire colon, extending from the rectum to the cecum. While usually associated with Crohn's disease, ileitis (inflammation of the ileum) also occurs in UC. About 17% of individuals with UC have ileitis.[21] Ileitis more commonly occurs in the setting of pancolitis (occurring in 20% of cases of pancolitis),[12] and tends to correlate with the activity of colitis. This so-called "backwash ileitis" can occur in 10–20% of people with pancolitis and is believed to be of little clinical significance.[22]
Severity of disease
In addition to the extent of involvement, UC is also characterized by severity of disease.[19] Severity of disease is defined by symptoms, objective markers of inflammation (endoscopic findings, blood tests), disease course, and the impact of the disease on day-to-day life.[19] Most patients are categorized through endoscopy and fecal calprotectin levels. Indicators of low risk for future complications in mild and moderate UC include the following parameters: exhibiting less than 6 stools daily and lack of fever/weight loss. Other indicators include lack of extraintestinal symptoms, low levels of the inflammatory markers C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR), and fecal calprotectin, and later age of diagnosis (over 40 years).[23] Mild disease correlates with fewer than four stools daily; in addition, mild urgency and rectal bleeding may occur intermittently.[19] Mild disease lacks systemic signs of toxicity (e.g. fever, chills, weight changes) and exhibits normal levels of the serum inflammatory markers ESR and CRP.[23]
Moderate to severe disease correlates with more than six stools daily, frequent bloody stools and urgency.[19] Moderate abdominal pain, low-grade fever, 38 to 39 °C (100 to 102 °F), and anemia may develop.[19] ESR and CRP are usually elevated.[19]
The Mayo Score, which incorporates a combination of clinical symptoms (stool frequency and amount of rectal bleeding) with endoscopic findings and a physicians assessment of severity, is often used clinically to classify UC as mild, moderate or severe.[13]
Acute-Severe Ulcerative Colitis (ASUC) is a severe form which presents acutely and with severe symptoms. This fulminant type is associated with severe symptoms (usually diarrhea, rectal bleeding and abdominal pain) and is usually associated with systemic symptoms including fever.
Ulcerative colitis may improve and enter remission.[19]
Extraintestinal manifestations and complications
| Crohn's disease |
Ulcerative colitis | ||
|---|---|---|---|
| Nutrient deficiency | Higher risk | ||
Colon cancer risk |
Slight | Considerable | |
| Prevalence of extraintestinal complications[25][26][27] | |||
Iritis/uveitis |
Females | 2.2% | 3.2% |
| Males | 1.3% | 0.9% | |
| Primary sclerosing cholangitis |
Females | 0.3% | 1% |
| Males | 0.4% | 3% | |
| Ankylosing spondylitis |
Females | 0.7% | 0.8% |
| Males | 2.7% | 1.5% | |
| Pyoderma gangrenosum |
Females | 1.2% | 0.8% |
| Males | 1.3% | 0.7% | |
| Erythema nodosum | Females | 1.9% | 2% |
| Males | 0.6% | 0.7% | |

UC is characterized by immune dysregulation and systemic inflammation, which may result in
UC may affect the mouth. About 8% of individuals with UC develop oral manifestations.[31] The two most common oral manifestations are aphthous stomatitis and angular cheilitis.[31] Aphthous stomatitis is characterized by ulcers in the mouth, which are benign, noncontagious and often recurrent. Angular chelitis is characterized by redness at the corners of the mouth, which may include painful sores or breaks in the skin.[31] Very rarely, benign pustules may occur in the mouth (pyostomatitis vegetans).[31]
UC may affect the eyes manifesting in scleritis, iritis, and conjunctivitis. Patients may be asymptomatic or experience redness, burning, or itching in eyes. Inflammation may occur in the interior portion of the eye, leading to
UC may cause several joint manifestations, including a type of rheumatologic disease known as
Ulcerative colitis may affect the skin. The most common type of skin manifestation, erythema nodosum, presents in up to 3% of UC patients. It develops as raised, tender red nodules usually appearing on the outer areas of the arms or legs, especially in the anterior tibial area (shins).[34] The nodules have diameters that measure approximately 1–5 cm. Erythema nodosum is due to inflammation of the underlying subcutaneous tissue (panniculitis), and biopsy will display focal panniculitis (although is often unnecessary in diagnosis). In contrast to joint-related manifestations, erythema nodosum often occurs alongside intestinal disease. Thus, treatment of UC can often lead to resolution of skin nodules.[35]
Another skin condition associated with UC is pyoderma gangrenosum, which presents as deep skin ulcerations. Pyoderma gangrenosum is seen in about 1% of patients with UC and its formation is usually independent of bowel inflammation.[13] Pyoderma gangrenosum is characterized by painful lesions or nodules that become ulcers which progressively grow. The ulcers are often filled with sterile pus-like material. In some cases, pyoderma gangrenosum may require injection with corticosteroids.[28] Treatment may also involve inhibitors of tumor necrosis factor (TNF), a cytokine that promotes cell survival.[35]
Other associations determined between the skin and ulcerative colitis include a skin condition known as
Ulcerative colitis may affect the circulatory and endocrine system. UC increases the risk of blood clots in both arteries and veins;
Osteoporosis may occur related to systemic inflammation or prolonged steroid use in the treatment of UC, which increases the risk of bone fractures.[18] Clubbing, a deformity of the ends of the fingers, may occur.[18] Amyloidosis may occur, especially with severe and poorly controlled disease, which usually presents with protein in the urine (proteinuria) and nephritic syndrome.[18]
Primary sclerosing cholangitis
Ulcerative colitis (UC) has a significant association with primary sclerosing cholangitis (PSC), a progressive inflammatory disorder of small and large bile ducts. Up to 70-90% of people with primary sclerosing cholangitis have ulcerative colitis.[34] As many as 5% of people with UC may progress to develop primary sclerosing cholangitis.[28][40] PSC is more common in men, and often begins between 30 and 40 years of age.[28] It can present asymptomatically or exhibit symptoms of itchiness (pruritis) and fatigue. Other symptoms include systemic signs such as fever and night sweats. Such symptoms are often associated with a bacterial episodic version of PSC. Upon physical exam, one may discern enlarged liver contours (hepatomegaly) or enlarged spleen (splenomegaly) as well as areas of excoriation. Yellow coloring of the skin, or jaundice, may also be present due to excess of bile byproduct buildup (bilirubin) from the biliary tract.
In diagnosis, lab results often reveal a pattern indicative of biliary disease (cholestatic pattern). This is often displayed by markedly elevated alkaline phosphatase levels and milder or no elevation in liver enzyme levels. Results of endoscopic retrograde cholangiography (ERC) may show bile ducts with thicker walls, areas of dilation or narrowing. However, some patients with UC and PSC have inflammation that has significantly affected only ramified intrahepatic bile ducts of smaller diameter, also known as "small ducts", which are not visualized by ERC.[41]: 604, 609
In some cases, primary sclerosing cholangitis occurs several years before the bowel symptoms of ulcerative colitis develop.[34] PSC does not parallel the onset, extent, duration, or activity of the colonic inflammation in ulcerative colitis.[34] In addition, colectomy does not have an impact on the course of primary sclerosing cholangitis in individuals with UC.[34] PSC is associated with an increased risk of colorectal cancer and cholangiocarcinoma (bile duct cancer).[34][28] PSC is a progressive condition, and may result in cirrhosis of the liver.[28] No specific therapy has been proven to affect the long-term course of PSC.[28]
Causes
| Crohn's disease | Ulcerative colitis | |
|---|---|---|
| Smoking | Higher risk for smokers | Lower risk for smokers[19] |
| Age | Usual onset between 15 and 30 years[42] |
Peak incidence between 15 and 25 years |
Ulcerative colitis is an
Genetic factors
A genetic component to the cause of UC can be hypothesized based on aggregation of UC in families, variation of prevalence between different ethnicities,
Twelve regions of the
Multiple autoimmune disorders are associated with ulcerative colitis, including
Environmental factors
Many hypotheses have been raised for environmental factors contributing to the pathogenesis of ulcerative colitis, including diet, breastfeeding and medications. Breastfeeding may have a protective effect in the development of ulcerative colitis.[53][54] One study of isotretinoin found a small increase in the rate of UC.[55]
As the colon is exposed to many dietary substances which may encourage
As a result of a class-action lawsuit and community settlement with DuPont, three epidemiologists conducted studies on the population surrounding a chemical plant that was exposed to PFOA at levels greater than in the general population. The studies concluded that there was an association between PFOA exposure and six health outcomes, one of which being ulcerative colitis.[64]
Alternative theories
Levels of
Infection by
Pathophysiology
| Crohn's disease | Ulcerative colitis | |
|---|---|---|
| Cytokine response | Associated with Th17[67] |
Vaguely associated with Th2
|
An increased amount of colonic sulfate-reducing bacteria has been observed in some people with ulcerative colitis, resulting in higher concentrations of the toxic gas hydrogen sulfide. Human colonic mucosa is maintained by the colonic epithelial barrier and immune cells in the lamina propria (see intestinal mucosal barrier). The short-chain fatty acid n-butyrate gets oxidized through the beta oxidation pathway into carbon dioxide and ketone bodies. It has been shown that n-butyrate helps supply nutrients to this epithelial barrier. Studies have proposed that hydrogen sulfide plays a role in impairing this beta-oxidation pathway by interrupting the short chain acetyl-CoA dehydrogenase, an enzyme within the pathway. Furthermore, it has been suggested that the protective effect of smoking in ulcerative colitis is due to the hydrogen cyanide from cigarette smoke reacting with hydrogen sulfide to produce the non-toxic isothiocyanate, thereby inhibiting sulfides from interrupting the pathway.[68] An unrelated study suggested that the sulfur contained in red meats and alcohol may lead to an increased risk of relapse for people in remission.[65]
Other proposed mechanisms driving the pathophysiology of ulcerative colitis involve an abnormal immune response to the normal
Diagnosis
The initial diagnostic workup for ulcerative colitis consists of a complete history and physical examination, assessment of signs and symptoms, laboratory tests and endoscopy.[69] Severe UC can exhibit high erythrocyte sedimentation rate (ESR), decreased albumin (a protein produced by the liver), and various changes in electrolytes. As discussed previously, UC patients often also display elevated alkaline phosphatase. Inflammation in the intestine may also cause higher levels of fecal calprotectin or lactoferrin.[70]
Specific testing may include the following:[19][71]
- A thrombocytosis, a high plateletcount, is occasionally seen
- hypomagnesemiaand kidney injury.
- Liver function tests are performed to screen for bile duct involvement: primary sclerosing cholangitis.
- Imaging such as x-ray or CT scan to evaluate for possible perforation or toxic megacolon
- Stool culture and Clostridioides difficile stool assay to rule out infectious colitis[69]
- Inflammatory markers, such as erythrocyte sedimentation rate or C-reactive protein
- Lower endoscopy to evaluate the rectum and distal large intestine (sigmoidoscopy) or entire colon and end of the small intestine (colonoscopy) for ulcers and inflammation
Although ulcerative colitis is a disease of unknown causation, inquiry should be made as to unusual factors believed to trigger the disease.[19]
The simple clinical colitis activity index was created in 1998 and is used to assess the severity of symptoms.[72]
Endoscopic

The best test for diagnosis of ulcerative colitis remains
Ulcerative colitis is usually continuous from the rectum, with the rectum almost universally being involved. Perianal disease is rare. The degree of involvement endoscopically ranges from proctitis (rectal inflammation) to left sided colitis (extending to descending colon), to extensive colitis (extending proximal to descending colon).[14]
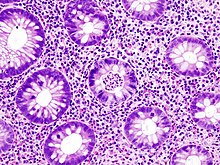
Histologic

Laboratory tests
Blood and stool tests serve primarily to assess disease severity, level of inflammation and rule out causes of infectious colitis. All individuals with suspected ulcerative colitis should have stool testing to rule out infection.[12]
A complete blood count may demonstrate anemia, leukocytosis, or thrombocytosis.[12] Anemia may be caused by inflammation or bleeding. Chronic blood loss may lead to iron deficiency as a cause for anemia, particularly microcytic anemia (small red blood cells), which can be evaluated with a serum ferritin, iron, total iron-binding capacity and transferrin saturation. Anemia may be due to a complication of treatment from azathioprine, which can cause low blood counts,[75] or sulfasalazine, which can result in folate deficiency. Thiopurine metabolites (from azathioprine) and a folate level can help.[76]
UC may cause high levels of inflammation throughout the body, which may be quantified with serum inflammatory markers, such as CRP and ESR. However, elevated inflammatory markers are not specific for UC and elevations are commonly seen in other conditions, including infection. In addition, inflammatory markers are not uniformly elevated in people with ulcerative colitis. Twenty five percent of individuals with confirmed inflammation on endoscopic evaluation have a normal CRP level.[19] Serum albumin may also be low related to inflammation, in addition to loss of protein in the GI tract associated with bleeding and colitis. Low serum levels of vitamin D are associated with UC, although the significance of this finding is unclear.[77]
Specific antibody markers may be elevated in ulcerative colitis. Specifically,
Several stool tests may help quantify the extent of inflammation present in the colon and rectum.
Imaging
Overall, imaging tests, such as x-ray or CT scan, may be helpful in assessing for complications of ulcerative colitis, such as perforation or toxic megacolon. Bowel ultrasound (US) is a cost-effective, well-tolerated, non-invasive and readily available tool for the management of patients with inflammatory bowel disease (IBD), including UC, in clinical practice.[79] Some studies demonstrated that bowel ultrasound is an accurate tool for assessing disease activity in people with ulcerative colitis.[80][81] Imaging is otherwise of limited use in diagnosing ulcerative colitis.[12][28] Magnetic resonance imaging (MRI) is necessary to diagnose underlying PSC.[28]
Abdominal xray is often the test of choice and may display nonspecific findings in cases of mild or moderate ulcerative colitis. In circumstances of severe UC, radiographic findings may include thickening of the mucosa, often termed "thumbprinting", which indicates swelling due to fluid displacement (edema). Other findings may include colonic dilation and stool buildup evidencing constipation.[70]
Similar to xray, in mild ulcerative colitis, double contrast barium enema often shows nonspecific findings. Conversely, barium enema may display small buildups of barium in microulcerations. Severe UC can be characterized by various polyps, colonic shortening, loss of haustrae (the small bulging pouches in the colon),and narrowing of the colon. It is important to note that barium enema should not be conducted in patients exhibiting very severe symptoms as this may slow or stop stool passage through the colon causing ileus and toxic megacolon.[70]
Other methods of imaging include computed tomography (CT) and magnetic resonance imaging (MRI). Both may depict colonic wall thickening but have decreased ability to find early signs of wall changes when compared to barium enema. In cases of severe ulcerative colitis, however, they often exhibit equivalent ability to detect colonic changes.[70]
Doppler ultrasound is the last means of imaging that may be used. Similar to the imaging methods mentioned earlier, this may show some thickened bowel wall layers. In severe cases, this may show thickening in all bowel wall layers (transmural thickness).[70]
Differential diagnosis
Several conditions may present in a similar manner as ulcerative colitis and should be excluded. Such conditions include: Crohn's disease, infectious colitis,
The most common disease that mimics the symptoms of ulcerative colitis is Crohn's disease, as both are inflammatory bowel diseases that can affect the colon with similar symptoms. It is important to differentiate these diseases since their courses and treatments may differ. In some cases, however, it may not be possible to tell the difference, in which case the disease is classified as indeterminate colitis.[83] Crohn's disease can be distinguished from ulcerative colitis in several ways. Characteristics that indicate Crohn's include evidence of disease around the anus (perianal disease). This includes anal fissures and abscesses as well as fistulas, which are abnormal connections between various bodily structures.[84]
Infectious colitis is another condition that may present in similar manner to ulcerative colitis. Endoscopic findings are also oftentimes similar. One can discern whether a patient has infectious colitis by employing tissue cultures and stool studies. Biopsy of the colon is another beneficial test but is more invasive.
Other forms of colitis that may present similarly include radiation and diversion colitis. Radiation colitis occurs after irradiation and often affects the rectum or sigmoid colon, similar to ulcerative colitis. Upon histology radiation colitis may indicate eosinophilic infiltrates, abnormal epithelial cells, or fibrosis. Diversion colitis, on the other hand, occurs after portions of bowel loops have been removed. Histology in this condition often shows increased growth of lymphoid tissue.
In patients who have undergone transplantation, graft versus host disease may also be a differential diagnosis. This response to transplantation often causes prolonged diarrhea if the colon is affected. Typical symptoms also include rash. Involvement of the upper gastrointestinal tract may lead to difficulty swallowing or ulceration. Upon histology, graft versus host disease may present with crypt cell necrosis and breakdown products within the crypts themselves.[85]
| Crohn's disease | Ulcerative colitis | |
|---|---|---|
Terminal ileum involvement |
Commonly | Seldom |
| Colon involvement | Usually | Always |
| Rectum involvement | Seldom | Usually (95%)[19] |
| Involvement around the anus |
Common[86] | Seldom |
| Bile duct involvement | No increase in rate of primary sclerosing cholangitis | Higher rate[87] |
| Distribution of disease | Patchy areas of inflammation (skip lesions) | Continuous area of inflammation[19] |
| Endoscopy | Deep geographic and serpiginous (snake-like) ulcers
|
Continuous ulcer |
| Depth of inflammation | May be transmural, deep into tissues[86][46] | Shallow, mucosal |
| Stenosis | Common | Seldom |
| Granulomas on biopsy | May have non- | Non-peri- intestinal crypt granulomas not seen[90]
|
Management
Standard treatment for ulcerative colitis depends on the extent of involvement and disease severity. The goal is to induce remission initially with medications, followed by the administration of maintenance medications to prevent a relapse. The concept of induction of remission and maintenance of remission is very important. The medications used to induce and maintain a remission somewhat overlap, but the treatments are different. Physicians first direct treatment to inducing remission, which involves relief of symptoms and mucosal healing of the colon's lining, and then longer-term treatment to maintain remission and prevent complications.[91]
For acute stages of the disease, a low fiber diet may be recommended.[92][93][94]
Medication
The first-line maintenance medication for ulcerative colitis in remission is
A formulation of
Aminosalicylates
Sulfasalazine has been a major agent in the therapy of mild to moderate ulcerative colitis for over 50 years. In 1977, it was shown that 5-aminosalicylic acid (5-ASA, mesalazine/mesalamine) was the therapeutically active component in sulfasalazine.[109] Many 5-ASA drugs have been developed with the aim of delivering the active compound to the large intestine to maintain therapeutic efficacy but with reduction of the side effects associated with the sulfapyridine moiety in sulfasalazine. Oral 5-ASA drugs are particularly effective in inducing and in maintaining remission in mild to moderate ulcerative colitis.[110][111] Rectal suppository, foam or liquid enema formulations of 5-ASA are used for colitis affecting the rectum, sigmoid or descending colon, and have been shown to be effective especially when combined with oral treatment.[112]
Biologics
Biologic treatments such as the TNF inhibitors infliximab, adalimumab, and golimumab are commonly used to treat people with UC who are no longer responding to corticosteroids. Tofacitinib and vedolizumab can also produce good clinical remission and response rates in UC.[8] Biologics may be used early in treatment (step down approach), or after other treatments have failed to induce remission (step up approach); the strategy should be individualized.[113]
Unlike aminosalicylates, biologics can cause serious side effects such as an increased risk of developing extra-intestinal cancers,[114] heart failure; and weakening of the immune system, resulting in a decreased ability of the immune system to clear infections and reactivation of latent infections such as tuberculosis. For this reason, people on these treatments are closely monitored and are often tested for hepatitis and tuberculosis annually.[115][116]
Etrasimod, a once-daily oral sphingosine 1-phosphate (S1P) receptor modulator that selectively activates S1P receptor subtypes 1, 4, and 5 with no detectable activity on S1P 2 or 3, is in development for treatment of immune-mediated diseases, including ulcerative colitis, and was shown in 2 randomized trials to be effective and well tolerated as induction and maintenance therapy in patients with moderately to severely active ulcerative colitis.[117]
Nicotine
Unlike
Iron supplementation
The gradual loss of blood from the gastrointestinal tract, as well as chronic inflammation, often leads to anemia, and professional guidelines suggest routinely monitoring for anemia with blood tests repeated every three months in active disease and annually in quiescent disease.
Anticholinergics
Anticholinergic drugs, more specifically muscarinic antagonists, are sometimes used to treat abdominal cramps in connection with ulcerative colitis through their calming effect on colonic peristalsis (reducing both amplitude and frequency) and intestinal tone.[130][131] Some medical authorities suggest over-the-counter anticholinergic drugs as potential helpful treatments for abdominal cramping in mild ulcerative colitis.[132] However, their use is contraindicated especially in moderate to severe disease states because of the potential for anticholinergic treatment to induce toxic megacolon in patients with colonic inflammation.[133] Toxic megacolon is a state in which the colon is abnormally distended, and may in severe or untreated cases lead to colonic perforation, sepsis, and death.[134]
Immunosuppressant therapies, infection risks and vaccinations
Many patients affected by ulcerative colitis need immunosuppressant therapies, which may be associated with a higher risk of contracting opportunistic infectious diseases.[135] Many of these potentially harmful diseases, such as Hepatitis B, Influenza, chickenpox, herpes zoster virus, pneumococcal pneumonia, or human papilloma virus, can be prevented by vaccines. Each drug used in the treatment of IBD should be classified according to the degree of immunosuppression induced in the patient. Several guidelines suggest investigating patients' vaccination status before starting any treatment and performing vaccinations against vaccine preventable diseases when required.[136][137] Compared to the rest of the population, patients affected by IBD are known to be at higher risk of contracting some vaccine-preventable diseases.[138] Patients treated with Janus kinase inhibitor showed higher risk of Shingles.[139] Nevertheless, despite the increased risk of infections, vaccination rates in IBD patients are known to be suboptimal and may also be lower than vaccination rates in the general population.[140][141]
Surgery
Crohn's disease |
Ulcerative colitis
| |
|---|---|---|
| Mesalazine | Less useful[142] | More useful[142] |
| Antibiotics | Effective in long-term[143] | Generally not useful[144] |
| Surgery | Often returns following removal of affected part |
Usually cured by removal of colon |
Unlike in Crohn's disease, the gastrointestinal aspects of ulcerative colitis can generally be cured by surgical removal of the large intestine, though extraintestinal symptoms may persist. This procedure is necessary in the event of: exsanguinating hemorrhage, frank perforation, or documented or strongly suspected carcinoma. Surgery is also indicated for people with severe colitis or toxic megacolon. People with symptoms that are disabling and do not respond to drugs may wish to consider whether surgery would improve the quality of life.[14]
The removal of the entire large intestine, known as a
Another surgical option for ulcerative colitis that is affecting most of the large bowel is called the
While the ileal pouch procedure removes the need for an ostomy bag, it does not restore normal bowel function. In the months following the final operation, patients typically experience 8–15 bowel movements a day. Over time this number decreases, with many patients reporting 4–6 bowel movements after one year post-op. While many patients have success with this procedure, there are a number of known complications. Pouchitis, inflammation of the ileal pouch resulting in symptoms similar to ulcerative colitis, is relatively common. Pouchitis can be acute, remitting, or chronic however treatment using antibiotics, steroids, or biologics can be highly effective. Other complications include fistulas, abscesses, and pouch failure. Depending on the severity of the condition, pouch revision surgery may need to be performed. In some cased the pouch may need to be de-functioned or removed and an ileostomy recreated.[146][147]
The risk of cancer arising from an ileal pouch anal anastomosis is low.[148] However, annual surveillance with pouchoscopy may be considered in individuals with risk factors for dysplasia, such as a history of dysplasia or colorectal cancer, a history of PSC, refractory pouchitis, and severely inflamed atrophic pouch mucosa.[148]
Bacterial recolonization
In a number of randomized clinical trials,
A
It is unclear whether probiotics help to prevent future relapse in people with stable disease activity, either as a monotherapy or combination therapy.[151]
Fecal microbiota transplant involves the infusion of human probiotics through fecal enemas. Ulcerative colitis typically requires a more prolonged bacteriotherapy treatment than Clostridioides difficile infection does to be successful, possibly due to the time needed to heal the ulcerated epithelium. The response of ulcerative colitis is potentially very favorable with one study reporting 67.7% of people experiencing complete remission.[152] Other studies found a benefit from using fecal microbiota transplantation.[153][154][155]
Alternative medicine
A variety of alternative medicine therapies have been used for ulcerative colitis, with inconsistent results. Curcumin (turmeric) therapy, in conjunction with taking the medications mesalamine or sulfasalazine, may be effective and safe for maintaining remission in people with quiescent ulcerative colitis.[156][157] The effect of curcumin therapy alone on quiescent ulcerative colitis is unknown.[157]
Treatments using cannabis or cannabis oil are uncertain. So far, studies have not determined its effectiveness and safety.[158]
Abdominal pain management
Many interventions have been considered to manage abdominal pain in people with ulcerative colitis, including FODMAPs diet, relaxation training, yoga, kefir diet and stellate ganglion block treatment. It is unclear whether any of these are safe or effective at improving pain or reducing anxiety and depression.[159]
Nutrition
Diet can play a role in symptoms of patients with ulcerative colitis.[160]
The most avoided foods by patients are spicy foods, dairy products, alcohol, fruits and vegetables and carbonated beverages; these foods are mainly avoided during remission and to prevent relapse. In some cases, especially in the flares period, the dietary restrictions of these patients can be very severe and can lead to a compromised nutritional state. Some patients tend to eliminate gluten spontaneously, despite not having a definite diagnosis of Coeliac disease, because they believe that gluten can exacerbate gastrointestinal symptoms.[161]
Mental health
Many studies found that patients with IBD reported a higher frequency of depressive and anxiety disorders than the general population, and most studies confirm that women with IBD are more likely than men to develop affective disorders and show that up to 65% of them may have
Prognosis
Poor prognostic factors include: age < 40 years upon diagnosis, extensive colitis, severe colitis on endoscopy, prior hospitalization, elevated CRP and low serum albumin.[19]
Progression or remission
People with ulcerative colitis usually have an intermittent course, with periods of disease inactivity alternating with "flares" of disease. People with proctitis or left-sided colitis usually have a more benign course: only 15% progress proximally with their disease, and up to 20% can have sustained remission in the absence of any therapy. A subset of people experience a course of disease progress rapidly. In these cases, there is usually a failure to respond to medication and surgery often is performed within the first few years of disease onset.[164][165] People with more extensive disease are less likely to sustain remission, but the rate of remission is independent of the severity of the disease.[166] Several risk factors are associated with eventual need for colectomy, including: prior hospitalization for UC, extensive colitis, need for systemic steroids, young age at diagnosis, low serum albumin, elevated inflammatory markers (CRP & ESR), and severe inflammation seen during colonoscopy.[97][19] Surgical removal of the large intestine is necessary in some cases.[19]
Colorectal cancer
The risk of
Mortality
People with ulcerative colitis are at similar
Epidemiology
Together with Crohn's disease, about 11.2 million people were affected as of 2015[update].[172] Each year it newly occurs in 1 to 20 per 100,000 people, and 5 to 500 per 100,000 individuals are affected.[7][9] The disease is more common in North America and Europe than other regions.[9] Often it begins in people aged 15 to 30 years, or among those over 60.[1] Males and females appear to be affected in equal proportions.[7] It has also become more common since the 1950s.[7][9] Together, ulcerative colitis and Crohn's disease affect about a million people in the United States.[173] With appropriate treatment the risk of death appears the same as that of the general population.[3] The first description of ulcerative colitis occurred around the 1850s.[9]
Each year, ulcerative colitis newly occurs in 1 to 20 per 100,000 people (incidence), and there are a total of 5–500 per 100,000 individuals with the disease (prevalence).[7][9] In 2015, a worldwide total of 47,400 people died due to inflammatory bowel disease (UC and Crohn's disease).[6] The peak onset is between 30 and 40 years of age,[12] with a second peak of onset occurring in the 6th decade of life.[174] Ulcerative colitis is equally common among men and women.[12][7] With appropriate treatment the risk of death appears similar to that of the general population.[3] UC has become more common since the 1950s.[7][9]
The geographic distribution of UC and Crohn's disease is similar worldwide,[175] with the highest number of new cases a year of UC found in Canada, New Zealand and the United Kingdom.[176] The disease is more common in North America and Europe than other regions.[9] In general, higher rates are seen in northern locations compared to southern locations in Europe[177] and the United States.[178] UC is more common in western Europe compared with eastern Europe.[179] Worldwide, the prevalence of UC varies from 2 to 299 per 100,000 people.[5] Together, ulcerative colitis and Crohn's disease affect about a million people in the United States.[173]
As with Crohn's disease, the rates of UC are greater among
United States
As of 2004[update], the number of new cases of UC in the United States was between 2.2 and 14.3 per 100,000 per year.[182] The number of people affected in the United States in 2004 was between 37 and 246 per 100,000.[182]
Canada
In Canada, between 1998 and 2000, the number of new cases per year was 12.9 per 100,000 population or 4,500 new cases. The number of people affected was estimated to be 211 per 100,000 or 104,000.[183]
United Kingdom
In the United Kingdom 10 per 100,000 people newly develop the condition a year while the number of people affected is 243 per 100,000. Approximately 146,000 people in the United Kingdom have been diagnosed with UC.[184]
History
The term ulcerative colitis was first used by Samuel Wilks in 1859. The term entered general medical vocabulary afterwards in 1888 with William Hale-White publishing a report of various cases of "ulcerative colitis".[185]
UC was the first subtype of IBD to be identified.[185]
Research
Gram positive bacteria present in the lumen could be associated with extending the time of relapse for ulcerative colitis.[190]
A series of drugs in development looks to disrupt the inflammation process by selectively targeting an ion channel in the inflammation signaling cascade known as KCa3.1.[191] In a preclinical study in rats and mice, inhibition of KCa3.1 disrupted the production of Th1 cytokines IL-2 and TNF-α and decreased colon inflammation as effectively as sulfasalazine.[191]
Neutrophil extracellular traps[192] and the resulting degradation of the extracellular matrix[193] have been reported in the colon mucosa in ulcerative colitis patients in clinical remission, indicating the involvement of the innate immune system in the etiology.[192]
Fexofenadine, an antihistamine drug used in treatment of allergies, has shown promise in a combination therapy in some studies.[194][195] Opportunely, low gastrointestinal absorption (or high absorbed drug gastrointestinal secretion) of fexofenadine results in higher concentration at the site of inflammation. Thus, the drug may locally decrease histamine secretion by involved gastrointestinal mast cells and alleviate the inflammation.[195]
There is evidence that etrolizumab is effective for ulcerative colitis, with phase 3 trials underway as of 2016.[8][196][197][198] Etrolizumab is a humanized monoclonal antibody that targets the β7 subunit of integrins α4β7 and αEβ7, ultimately blocking migration and retention of leukocytes in the intestinal mucosa.[197] As of early 2022, Roche halted clinical trials for the use of etrolizumab in the treatment of ulcerative colitis.[199]
A type of leukocyte apheresis, known as granulocyte and monocyte adsorptive apheresis, still requires large-scale trials to determine whether or not it is effective.[200] Results from small trials have been tentatively positive.[201]
Notable cases
References
- ^ a b c d e f g h i j k l m n o p q r s t u v w x "Ulcerative Colitis". NIDDK. September 2014. Retrieved 3 August 2016.
- ^ "Ulcerative Colitis". Autoimmune Registry Inc. Retrieved 15 June 2022.
- ^ PMID 27158539.
- ISBN 9781437727722.
- ^ PMID 22001864.
- ^ PMID 27733281.
- ^ S2CID 14778938.
- ^ PMID 26600980.
- ^ PMID 22047562.
- ^ a b c d e f internetmedicin.se > Inflammatorisk tarmsjukdom, kronisk, IBD By Robert Löfberg. Retrieved Oct 2010 Translate.
- S2CID 31219115.)
{{cite journal}}: CS1 maint: DOI inactive as of January 2024 (link - ^ PMID 27914657.
- ^ S2CID 261696018.
- ^ PMID 28158501.
- PMID 26301120.
- PMID 8596552.
- PMID 23446338.
- ^ S2CID 1796160.
- ^ S2CID 73473272.
- S2CID 20223406.
- S2CID 42108108.
- ^ ISBN 978-0-07-159991-7
- ^ a b "UpToDate". www.uptodate.com. Retrieved 8 November 2022.
- ^ "UpToDate". www.uptodate.com. Retrieved 9 November 2022.
- PMID 957999.
- PMID 11316157.
- PMID 26614685.
- ^ PMID 31272578.
- PMID 18019875.
- PMID 26154136.
- ^ PMID 27433081.
- ^ PMID 28932076.
- PMID 30521217.
- ^ PMID 21180592.
- ^ S2CID 6905740.
- PMID 31290938.
- ^ S2CID 214946656.
- ^ PMID 24462530.
- PMID 29618721.
- PMID 2013375.
- PMID 9200295.
- ^ Nachimuthu S. "Crohn's disease". eMedicineHealth. Archived from the original on 9 December 2019. Retrieved 8 December 2019.
- PMID 20389289.
- ^ S2CID 218907577.
- PMID 3396969.
- ^ S2CID 35264387.
- PMID 10814724.
- S2CID 44102071.
- PMID 30422277.
- PMID 22504032.
- PMID 32552882.
- PMID 1771936.
- PMID 28892171.
- PMID 9698126.
- S2CID 918753.
- PMID 6673083.
- S2CID 11295804.
- PMID 15361498.
- PMID 22055893.
- PMID 15361484.
- S2CID 20919357.
- S2CID 30373968.
- S2CID 22547709.
- PMID 24284021.
- ^ S2CID 25496705.
- PMID 29308085.
- PMID 17570211.
- S2CID 3141574.
- ^ PMID 26025078.
- ^ PMID 17983810.
- ^ Ulcerative colitis at eMedicine
- PMID 9771402.
- ^ PMID 31562236.
- PMID 30837789.
- ^ "Azathioprine Product Information" (PDF). Access FDA. Food and Drug Administration.
- PMID 25518052.
- PMID 26348447.
- S2CID 26111716.
- S2CID 3344377.
- PMID 33349199.
- PMID 30085066.
- PMID 27467600.
- S2CID 40346031.
- S2CID 11446833.
- PMID 11596.
- ^ S2CID 31219115.)
{{cite journal}}: CS1 maint: DOI inactive as of January 2024 (link - S2CID 260320940.
- S2CID 36907992.
- S2CID 29476514.
- PMID 24942757.
- PMID 27226344.
- ^ "Should You Try a Low-Residue Diet?". WebMD. 25 October 2016. Retrieved 29 April 2017.
- ^ Manual of Clinical Nutrition Management (PDF). Compass Group. 2013.
- ^ Roncoroni L, Gori R, Elli L, et al. Nutrition in Patients with Inflammatory Bowel Diseases: A Narrative Review. Nutrients. 2022;14(4):751. Published 2022 Feb 10. doi:10.3390/nu14040751
- ^ PMID 22390554.
- ^ PMID 34635919.
- ^ PMID 31945371.
- PMID 12492172.
- PMID 30576644.
- ^ "FDA approves Uceris as ulcerative colitis treatment". Healio Gastroenterology. 15 January 2013.
- ^ "UCERIS (budesonide) extended release tablets label" (PDF). FDA.
- ^ "FDA approves new treatment for moderately to severely active ulcerative colitis". U.S. Food and Drug Administration (FDA) (Press release). 30 May 2018. Retrieved 31 May 2018.
- PMID 25162749.
- S2CID 74798482.
- S2CID 1294555.
- PMID 8196726.
- PMID 30726894.
- ^ "U.S. FDA Approves Pfizer's Velsipity for Adults with Moderately to Severely Active Ulcerative Colitis (UC)" (Press release). Pfizer. 13 October 2023. Retrieved 13 October 2023 – via Business Wire.
- S2CID 44785199.
- PMID 32786164.
- PMID 32856298.
- PMID 23152224.
- S2CID 195763151.
- PMID 27239106.
- S2CID 195771593.
- S2CID 21673794.
- S2CID 257286271.
- S2CID 5775169.
- PMID 18069751.
- PMID 22398093.
- PMID 15157822.
- PMID 10583016.
- S2CID 25745900.
- S2CID 24122049.
- PMID 8876866.
- PMID 10958212.
- ^ PMID 21561874.
- PMID 17985376.
- S2CID 8269837.
- PMID 14229762.
- S2CID 83791469.
- S2CID 219029672.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - S2CID 204891274.
- PMID 32547151.
- ^ Toruner, M.; Loftus, E.V.; Harmsen, W.S.; Zinsmeister, A.R.; Orenstein, R.; Sandborn, W.J.; Colombel, J.; Egan, L.J. Risk factors for opportunistic infections in patients with inflammatory bowel disease. Gastroenterology 2008, 134, 929–936
- ^ Farraye, F.A.; Melmed, G.Y.; Lichtenstein, G.R.; Kane, S.V. ACG Clinical Guideline: Preventive Care in Inflammatory Bowel Disease. Am. J. Gastroenterol. 2017, 112, 241–258.
- ^ Kucharzik, T.; Ellul, P.; Greuter, T.; Rahier, J.F.; Verstockt, B.; Abreu, C.; Albuquerque, A.; Allocca, M.; Esteve, M.; Farraye, F.A.; et al. ECCO Guidelines on the Prevention, Diagnosis, and Management of Infections in Inflammatory Bowel Disease. J. Crohn’s Colitis 2021, 15, 879–913.
- ^ Ananthakrishnan, A.N.; McGinley, E.L. Infection-related hospitalizations are associated with increased mortality in patients with inflammatory bowel diseases. J. Crohn’s Colitis 2013, 7, 107–112.
- ^ Winthrop, K.L.; Melmed, G.Y.; Vermeire, S.; Long, M.D.; Chan, G.; Pedersen, R.D.; Lawendy, N.; Thorpe, A.J.; Nduaka, C.I.; Su, C. Herpes Zoster Infection in Patients with Ulcerative Colitis Receiving Tofacitinib. Inflamm. Bowel Dis. 2018, 24, 2258–2265
- ^ Malhi, G.; Rumman, A.; Thanabalan, R.; Croitoru, K.; Silverberg, M.S.; Steinhart, A.H.; Nguyen, G.C. Vaccination in inflammatory bowel disease patients: Attitudes, knowledge, and uptake. J. Crohn’s Colitis 2015, 9, 439–444.
- ^ Costantino, A.; Michelon, M.; Noviello, D.; Macaluso, F.S.; Leone, S.; Bonaccorso, N.; Costantino, C.; Vecchi, M.; Caprioli, F., on behalf of AMICI Scientific Board. Attitudes towards Vaccinations in a National Italian Cohort of Patients with Inflammatory Bowel Disease. Vaccines 2023, 11, 1591.
- ^ ISBN 0-7817-7153-6.
- PMID 20067425.
- PMID 19444096.
- ^ "Living with a stoma". IBD Relief.
- ^ "Colectomy Not a Final Cure for Ulcerative Colitis, Data Show". www.mdedge.com. Retrieved 15 December 2019.
- PMID 27247537.
- ^ S2CID 201114672.
- PMID 21437015.
- ^ PMID 32128795.
- PMID 32128794.
- PMID 24257037.
- PMID 28906291.
- PMID 27295210.
- PMID 30644982.
- PMID 17101300.
- ^ PMID 23076948.
- PMID 30406638.
- PMID 34291816.
- ^ De Souza, H.; Fiocchi, C.; Iliopoulos, D. The IBD interactome: An integrated view of aetiology, pathogenesis and therapy. Nat. Rev. Gastroenterol. Hepatol. 2017, 14, 739–749
- license.
- ^ Fracas E, Costantino A, Vecchi M, Buoli M. Depressive and Anxiety Disorders in Patients with Inflammatory Bowel Diseases: Are There Any Gender Differences? International Journal of Environmental Research and Public Health. 2023; 20(13):6255. https://doi.org/10.3390/ijerph20136255
- ^ Barberio B, Zamani M, Black CJ, Savarino EV, Ford AC. Prevalence of symptoms of anxiety and depression in patients with inflammatory bowel disease: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2021 May;6(5):359-370. doi: 10.1016/S2468-1253(21)00014-5
- PMID 29659758.
- PMID 28526076.
- ISBN 9781416061892.
- S2CID 10801391.
- PMID 16564852.
- ^ S2CID 2086542.
- PMID 25071340.
- PMID 21731826.
- PMID 27733282.
- ^ ISBN 978-1455733941.
- PMID 11000558.
- PMID 12167685.
- PMID 3004417.
- PMID 9014768.
- PMID 1983816.
- S2CID 25069828.
- PMID 11248156.
- ^ PMID 3821808.
- ^ a b "Epidemiology of the IBD". Centers for Disease Control and Prevention (CDC). Archived from the original on 23 February 2017. Retrieved 23 February 2017.
- S2CID 40543366.
- ^ "Ulcerative colitis: management". National Institute for Health and Care Excellence. 3 May 2019.
- ^ PMID 24094598.
- ^ PMID 15825065.
- ^ S2CID 34563008.
- PMID 7541009.
- S2CID 31495688.
- PMID 25525379.
- ^ PMID 22891655.
- ^ PMID 25993694.
- PMID 30702115.
- S2CID 2605447.
- ^ PMID 23070081.
- S2CID 7369482.
- ^ PMID 26630451.
- S2CID 24706213.
- ^ Taylor N (3 February 2022). "Roche lets go of etro, dumping phase 3 Crohn's prospect 18 months after posting weak colitis data". Fierce Biotech. Retrieved 12 December 2023.
- S2CID 36724094.
- PMID 20817610.
Further reading
- Rubin DT, Ananthakrishnan AN, Siegel CA, Sauer BG, Long MD (March 2019). "ACG Clinical Guideline: Ulcerative Colitis in Adults". The American Journal of Gastroenterology. 114 (3): 384–413. S2CID 73473272.

- Torpy JM, Lynm C, Golub RM (January 2012). "JAMA patient page. Ulcerative colitis". JAMA. 307 (1): 104. PMID 22215172.
External links
- MedlinePlus ulcerative colitis page
 Media related to Ulcerative colitis at Wikimedia Commons
Media related to Ulcerative colitis at Wikimedia Commons
