Thymoma
| Thymoma | |
|---|---|
Adulthood | |
| Treatment | surgical removal, chemotherapy (in malignant cases). |
A thymoma is a
Signs and symptoms
A third of all people with a thymoma have symptoms caused by compression of the surrounding organs by an expansive mass. These problems may take the form of superior vena cava syndrome, dysphagia (difficulty swallowing), cough, or chest pain.[1]
One-third of patients have their tumors discovered because they have an associated
One-third to one-half of all persons with thymoma have no symptoms at all, and the mass is identified on a
Pathology
Thymoma originates from the epithelial cell population in the thymus, and several microscopic subtypes are now recognized.[1] There are three principal histological types of thymoma, depending on the appearance of the cells by microscopy:
- Type A if the epithelial cells have an oval or fusiform shape (less lymphocyte count);
- Type B if they have an epithelioid[clarification needed] shape (Type B has three subtypes: B1 (lymphocyte-rich), B2 (cortical) and B3 (epithelial).);[4]
- Type AB if the tumor contains a combination of both cell types.
Thymic cortical epithelial cells have abundant cytoplasm, vesicular nucleus with finely divided chromatin and small nucleoli and cytoplasmic filaments contact adjacent cells. Thymic medullary epithelial cells in contrast are spindle shaped with oval dense nucleus and scant cytoplasm thymoma if recapitulates cortical cell features more, is thought to be less benign.
Diagnosis

When a thymoma is suspected, a
The diagnosis is made via histologic examination by a pathologist, after obtaining a tissue sample of the mass. Final tumor classification and staging is accomplished pathologically after formal[clarification needed] surgical removal of the thymic tumor.
Selected laboratory tests can be used to look for associated problems or possible tumor spread. These include:
Staging
The Masaoka Staging System is used widely and is based on the anatomic extent of disease at the time of surgery:[6]
- I: Completely encapsulated
- IIA: Microscopic invasion through the capsule into surrounding fatty tissue
- IIB: Macroscopic invasion into capsule
- III: Macroscopic invasion into adjacent organs
- IVA: Pleural or pericardial implants
- IVB: Lymphogenous or hematogenous metastasis to distant (extrathoracic) sites
Treatment
Surgery is the mainstay of treatment for thymoma. If the tumor is apparently invasive and large, preoperative (neoadjuvant) chemotherapy and/or radiotherapy may be used to decrease the size and improve resectability, before surgery is attempted. When the tumor is an early stage (Masaoka I through IIB), no further therapy is necessary. Removal of the thymus in adults does not appear to induce
Prognosis
Prognosis is much worse for stage III or IV thymomas as compared with stage I and II tumors. Invasive thymomas uncommonly can also
Patients who have undergone thymectomy for thymoma should be warned of possible severe side effects after yellow fever vaccination. This is probably caused by inadequate T-cell response to live attenuated yellow fever vaccine. Deaths have been reported.[citation needed]
Epidemiology
The incidence of thymomas is around 0.13-0.26 per 100,000 people per year.[10] Males are affected slightly less frequently than females.[10] The typical age at diagnosis is in the 40s and 50s, though the age may range from six years to 83 years.[10]
Gallery
-
An encapsulated cystic thymoma.
-
A locally invasive circumscribed thymoma (mixed lymphocytic and epithelial, mixed polygonal and spindle).
-
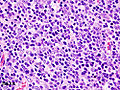
Histopathological image of thymoma type B1. Anterior mediastinal mass surgically resected. Hematoxylin & eosin stain.
-
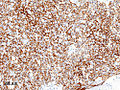
Histopathological image of thymoma type B1. Anterior mediastinal mass surgically resected. Cytokeratin CAM5.2 immunostain.
-
Histopathological image representing a noninvasive thymoma type B1, surgically resected. Hematoxylin & eosin.
-
Thymoma.FNA specimen. Field stain.
See also
- Mediastinal tumor
References
- ^ S2CID 12621667.
- ISBN 978-1-4160-2973-1.[page needed]
- PMID 26408958.
- PMID 11413764.
- PMID 22674945.
- PMID 7296496.
- ^ NCCN Thymoma, Guidelines (2016). "NCCN Thymoma Guidelines" (PDF). NCCN Guidelines.
- .
- PMID 10522726.
- ^ ISBN 978-92-832-4506-3.