Hepatoblastoma
| Hepatoblastoma | |
|---|---|
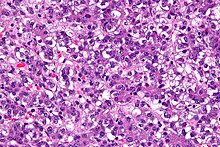 | |
| Micrograph of a hepatoblastoma. H&E stain. | |
| Specialty | Oncology |
Hepatoblastoma is a malignant
Signs and symptoms
Patients are usually asymptomatic at diagnosis.[3] As a result, disease is often advanced at diagnosis.
Pathophysiology


Hepatoblastomas originate from immature liver precursor cells, are typically unifocal, affect the right lobe of the
Individuals with
Recently, other components of the Wnt signaling pathway have also demonstrated a likely role in constitutive activation of this pathway in the causation of hepatoblastoma.[8][9] Accumulating evidence suggests that hepatoblastoma is derived from a pluripotent stem cell.[10]
Syndromes with an increased incidence of hepatoblastoma include Beckwith–Wiedemann syndrome, trisomy 18, trisomy 21, Acardi syndrome, Li–Fraumeni syndrome, Goldenhar syndrome, von Gierke disease, and familial adenomatous polyposis.[11]
Diagnosis
The most common method of testing for hepatoblastoma is a blood test checking the alpha-fetoprotein level. Alpha-fetoprotein (AFP) is used as a biomarker to help determine the presence of liver cancer in children. At birth, infants have relatively high levels of AFP, which fall to normal adult levels by the second year of life. The normal level for AFP in children has been reported as lower than 50 nanograms per milliliter (ng/ml) and 10 ng/ml in adults. An AFP level greater than 500 ng/ml is a significant indicator of hepatoblastoma. AFP is also used as an indicator of treatment success. If treatments are successful in removing the cancer, the AFP level is expected to return to normal.[12]
Treatment
Surgical
References
- ^ "Archived copy". Archived from the original on 2019-05-31. Retrieved 2010-09-15.
{{cite web}}: CS1 maint: archived copy as title (link)[full citation needed] - PMID 18166449.
- ^ Willert, Jennifer. "Pediatric Hepatoblastoma Clinical Presentation: History, Physical, Causes". emedicine.medscape.com.
- OCLC 953861627.
- PMID 16126064.
- S2CID 34824663.
- PMID 10850429.
- ^ PMID 16012954.
- PMID 15958610.
- PMID 12228907.
- ^ Zimmerman A, Saxena R. Hepatoblastoma. In: WHO Classification of Tumours of the Digestive System, 4th, Bosman FT, Carneiro F, Hruban RH, Theise ND (Eds), IARC, Lyon 2010. p.229.
- PMID 12065588.
- S2CID 11332782.
- S2CID 20741138.
- ^ Pediatric Hepatoblastoma at eMedicine
- S2CID 74339.
- PMID 12065556. Archived from the originalon 2013-04-15.
External links
- humpath #2775 (Pathology images)
