Desmoplastic small-round-cell tumor
| Desmoplastic small-round-cell tumor | |
|---|---|
| Other names | DSRCT[1] |
 | |
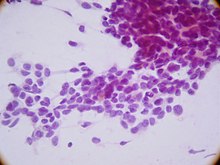
| Micrograph of a desmoplastic small round cell tumor, showing the characteristic desmoplastic stroma and angulated nests of small round cells. H&E stain. | |
| Specialty | Oncology |
| Prognosis | Five-year survival rate 15%[2] |
| Frequency | ~200 cases reported[2][3] |
Desmoplastic small-round-cell tumor (DSRCT) is an aggressive and rare
. It is characterized by the EWS-WT1 fusion protein.The
Signs and symptoms

There are few early warning signs that a patient has a DSRCT. Patients are often young and healthy as the tumors grow and spread uninhibited within the abdominal cavity. These are rare tumors and symptoms are often misdiagnosed by physicians. The abdominal masses can grow to enormous size before being noticed by the patient. The tumors can be felt as hard, round masses by palpating the abdomen.[citation needed]
First symptoms of the disease often include abdominal distention, abdominal mass, abdominal or back pain, gastrointestinal obstruction, lack of appetite, ascites, anemia, and cachexia.[citation needed]
Other reported symptoms include unknown lumps, thyroid conditions, hormonal conditions, blood clotting, kidney and urological problems, testicle, breast, uterine, vaginal, and ovarian masses.[citation needed]
Genetics
There are no known risk factors that have been identified specific to the disease. The tumor appears to arise from the primitive cells of childhood, and is considered a childhood cancer.[citation needed]
Research has indicated that there is a chimeric relationship between DSRCT and Wilms' tumor and Ewing sarcoma. Together with neuroblastoma and non-Hodgkin's lymphoma, they form the small-cell tumors.[citation needed]
DSRCT is associated with a unique
The EWS/WT1 translocation product targets
Pathology
The entity was first described by pathologists William L. Gerald and
On immunohistochemistry, these cells have trilinear coexpression including the epithelial marker cytokeratin, the mesenchymal markers desmin and vimentin, and the neuronal marker neuron-specific enolase. Thus, although initially thought to be of mesothelial origin due to sites of presentation, it is now hypothesized to arise from a progenitor cell with multiphenotypic differentiation.[citation needed]
Diagnosis
Differential diagnosis
Because this is a rare tumor, not many family physicians or oncologists are familiar with this disease. DSRCT in young patients can be mistaken for other abdominal tumors including rhabdomyosarcoma, neuroblastoma, and mesenteric carcinoid. In older patients DSRCT can resemble lymphoma, peritoneal mesothelioma, and peritoneal carcinomatosis. In males DSRCT may be mistaken for germ cell or testicular cancer while in females DSRCT can be mistaken for ovarian cancer. DSRCT shares characteristics with other small-round blue cell cancers including Ewing's sarcoma, acute leukemia, small cell mesothelioma, neuroblastoma, primitive neuroectodermal tumor, rhabdomyosarcoma, and Wilms' tumor.[citation needed]
Treatment
DSRCT is frequently
There is no standard protocol for the disease;
Prognosis
The prognosis for DSRCT remains poor.[14] Prognosis depends upon the stage of the cancer. Because the disease can be misdiagnosed or remain undetected, tumors frequently grow large within the abdomen and metastasize or seed to other parts of the body.
There is no known organ or area of origin. DSRCT can metastasize through lymph nodes or the blood stream. Sites of metastasis include the spleen, diaphragm, liver, large and small intestine, lungs, central nervous system, bones, uterus, bladder, genitals, abdominal cavity, and the brain.
A multi-modality approach of high-dose chemotherapy, aggressive surgical resection,[15] radiation, and stem cell rescue improves survival for some patients. Reports have indicated that patients will initially respond to first line chemotherapy and treatment but that relapse is common.
Some patients in remission or with inoperable tumor seem to benefit from long term low dose chemotherapy, turning DSRCT into a chronic disease.
Research
The examples and perspective in this section may not represent a worldwide view of the subject. (July 2016) |
The Stehlin Foundation[16] currently offers DSRCT patients the opportunity to send samples of their tumors free of charge for testing. Research scientists are growing the samples on nude mice and testing various chemical agents to find which are most effective against the individual's tumor.
Patients with advanced DSRCT may qualify to participate in
The Cory Monzingo Foundation is a 501(c)(3) organization that supports the research for treatments and a cure for DSRCT. The Cory Monzingo Foundation provides funding to MD Anderson Cancer Center and may also provide funding to other nonprofit cancer research organizations.
In 2002, Nishio and al,[17] established a novel human tumor cell line derived from the pleural effusion of a patient with a typical intra-abdominal DSRCT, called JN-DSRCT-1[18] that can now be used in research.
St. Jude Children’s Research Hospital has, in 2018, make available resources from the Childhood Solid Tumor Network, that upon request gives access to patient-derived orthotopic xenografts.[19]
Alternative names
This disease is also known as:
There is no connection to peritoneal mesothelioma which is another disease sometimes described as desmoplastic.
See also
- Desmoplasia
- Kate Granger (1981–2016), an English physician, whose diagnosis with DSRCT led to her campaigning for better patient care, and fund-raising for cancer research.
References
- ^ RESERVED, INSERM US14-- ALL RIGHTS. "Orphanet: Desmoplastic small round cell tumor". www.orpha.net. Retrieved 17 November 2019.
{{cite web}}: CS1 maint: numeric names: authors list (link) - ^ a b "Desmoplastic Small Round Cell Tumor". St. Jude Children's Research Hospital. Retrieved March 22, 2023.
- ^ "Desmoplastic Small Round Cell Tumors (DSRCT)". National Cancer Institute. Retrieved March 22, 2023.
- ^ Lee YS, Hsiao CH: Desmoplastic small round cell tumor: a clinicopathologic, immunohistochemical and molecular study of four patients. J Formos Med Assoc 2007; 106: 854–860.
- PMID 18081791.
- PMID 18703217.
- PMID 34203801.
- PMID 15826834.
- PMID 17964965.
- PMID 34340159.
- PMID 18523561.

- PMID 2473463.
- ^ Talarico F, Iusco D, Negri L, Belinelli D: Combined resection and multi-agent adjuvant chemotherapy for intra-abdominal desmoplastic small round cell tumour: case report and review of the literature. G Chir 2007; 28: 367–370.
- PMID 15868593.
- PMID 17915050.
- ^ "Official website for Stehlin Foundation". Archived from the original on 2021-04-12. Retrieved 2006-10-08.
- PMID 12218078.
- ^ "Jn-Dsrct-1".
- ^ "St Jude Children's Research Hospital".
