Radiobiology
Radiobiology (also known as radiation biology, and uncommonly as actinobiology) is a field of clinical and basic
Health effects
In general, ionizing radiation is harmful and potentially lethal to living beings but can have health benefits in
Most adverse health effects of radiation exposure may be grouped in two general categories:
- deterministic effects (harmful tissue reactions) due in large part to the killing or malfunction of cells following high doses; and
- stochastic effects, i.e., cancer and heritable effects involving either cancer development in exposed individuals owing to mutation of somatic cells or heritable disease in their offspring owing to mutation of reproductive (germ) cells.[1]
Stochastic
Some effects of ionizing radiation on human health are
Its most common impact is the stochastic
Quantitative data on the effects of ionizing radiation on human health is relatively limited compared to other medical conditions because of the low number of cases to date, and because of the stochastic nature of some of the effects. Stochastic effects can only be measured through large epidemiological studies where enough data has been collected to remove confounding factors such as smoking habits and other lifestyle factors. The richest source of high-quality data comes from the study of Japanese
The added lifetime risk of developing cancer by a single abdominal CT of 8 mSv is estimated to be 0.05%, or 1 in 2,000.[4]
Deterministic
High radiation dose gives rise to deterministic effects which reliably occur above a threshold, and their severity increases with dose. Deterministic effects are not necessarily more or less serious than stochastic effects; either can ultimately lead to a temporary nuisance or a fatality. Examples of deterministic effects are:
- Acute radiation syndrome, by acute whole-body radiation
- Radiation burns, from radiation to a particular body surface
- Radiation-induced thyroiditis, a potential side effect from radiation treatment against hyperthyroidism
- Chronic radiation syndrome, from long-term radiation.
- Radiation-induced lung injury, from for example radiation therapy to the lungs
- Cataracts and infertility.[2]
The US National Academy of Sciences Biological Effects of Ionizing Radiation Committee "has concluded that there is no compelling evidence to indicate a dose threshold below which the risk of tumor induction is zero".[5]
| Phase | Symptom | Whole-body absorbed dose (Gy) | ||||
|---|---|---|---|---|---|---|
| 1–2 Gy | 2–6 Gy | 6–8 Gy | 8–30 Gy | > 30 Gy | ||
| Immediate | Nausea and vomiting | 5–50% | 50–100% | 75–100% | 90–100% | 100% |
| Time of onset | 2–6 h | 1–2 h | 10–60 min | < 10 min | Minutes | |
| Duration | < 24 h | 24–48 h | < 48 h | < 48 h | — (patients die in < 48 h) | |
| Diarrhea | None | None to mild (< 10%) | Heavy (> 10%) | Heavy (> 95%) | Heavy (100%) | |
| Time of onset | — | 3–8 h | 1–3 h | < 1 h | < 1 h | |
| Headache | Slight | Mild to moderate (50%) | Moderate (80%) | Severe (80–90%) | Severe (100%) | |
| Time of onset | — | 4–24 h | 3–4 h | 1–2 h | < 1 h | |
| Fever | None | Moderate increase (10–100%) | Moderate to severe (100%) | Severe (100%) | Severe (100%) | |
| Time of onset | — | 1–3 h | < 1 h | < 1 h | < 1 h | |
| CNS function | No impairment | Cognitive impairment 6–20 h | Cognitive impairment > 24 h | Rapid incapacitation | ||
Latent period |
28–31 days | 7–28 days | < 7 days | None | None | |
Illness |
Mild to moderate Fatigue
Weakness |
Moderate to severe | Severe Electrolyte disturbance
|
Nausea Vomiting Severe diarrhea High fever Electrolyte disturbance Shock |
— (patients die in < 48h) | |
| Mortality | Without care | 0–5% | 5–95% | 95–100% | 100% | 100% |
| With care | 0–5% | 5–50% | 50–100% | 99–100% | 100% | |
| Death | 6–8 weeks | 4–6 weeks | 2–4 weeks | 2 days – 2 weeks | 1–2 days | |
| Table source[6] | ||||||
By type of radiation
When alpha particle emitting isotopes are ingested, they are far more dangerous than their half-life or decay rate would suggest. This is due to the high
In pregnancy
The risk for developing radiation-induced cancer at some point in life is greater when exposing a fetus than an adult, both because the cells are more vulnerable when they are growing, and because there is much longer lifespan after the dose to develop cancer. If there is too much radiation exposure there could be harmful effects on the unborn child or reproductive organs.[7] Research shows that scanning more than once in nine months can harm the unborn child.[8]
Possible deterministic effects include of radiation exposure in pregnancy include miscarriage, structural birth defects, growth restriction and intellectual disability.[9] The deterministic effects have been studied at for example survivors of the atomic bombings of Hiroshima and Nagasaki and cases where radiation therapy has been necessary during pregnancy:
Gestational age |
Embryonic age |
Effects | Estimated threshold dose (mGy) |
|---|---|---|---|
| 2 to 4 weeks | 0 to 2 weeks | Miscarriage or none (all or nothing) | 50 - 100[9] |
| 4 to 10 weeks | 2 to 8 weeks | Structural birth defects | 200[9] |
| Growth restriction | 200 - 250[9] | ||
| 10 to 17 weeks | 8 to 15 weeks | Severe intellectual disability | 60 - 310[9] |
| 18 to 27 weeks | 16 to 25 weeks | Severe intellectual disability (lower risk) | 250 - 280[9] |
The intellectual deficit has been estimated to be about 25 IQ points per 1,000 mGy at 10 to 17 weeks of gestational age.[9]
These effects are sometimes relevant when deciding about medical imaging in pregnancy, since projectional radiography and CT scanning exposes the fetus to radiation.
Also, the risk for the mother of later acquiring radiation-induced breast cancer seems to be particularly high for radiation doses during pregnancy.[10]
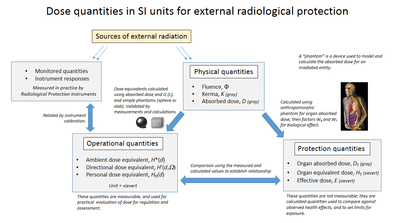
Measurement
The human body cannot sense ionizing radiation except in very high doses, but the effects of ionization can be used to characterize the radiation. Parameters of interest include disintegration rate, particle flux, particle type, beam energy, kerma, dose rate, and radiation dose.
The monitoring and calculation of doses to safeguard human health is called dosimetry and is undertaken within the science of health physics. Key measurement tools are the use of dosimeters to give the external effective dose uptake and the use of bio-assay for ingested dose. The article on the sievert summarises the recommendations of the ICRU and ICRP on the use of dose quantities and includes a guide to the effects of ionizing radiation as measured in sieverts, and gives examples of approximate figures of dose uptake in certain situations.
The committed dose is a measure of the stochastic health risk due to an intake of radioactive material into the human body. The ICRP states "For internal exposure, committed effective doses are generally determined from an assessment of the intakes of radionuclides from bioassay measurements or other quantities. The radiation dose is determined from the intake using recommended dose coefficients".[11]
Absorbed, equivalent and effective dose
The
To represent stochastic risk the
Organizations
The International Commission on Radiological Protection (ICRP) manages the International System of Radiological Protection, which sets recommended limits for dose uptake. Dose values may represent absorbed, equivalent, effective, or committed dose.
Other important organizations studying the topic include
- International Commission on Radiation Units and Measurements (ICRU)
- United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR)
- US National Council on Radiation Protection and Measurements (NCRP)
- UK UK Health Security Agency
- US National Academy of Sciences (NAS through the BEIR studies)
- French Institut de radioprotection et de sûreté nucléaire (IRSN)
- European Committee on Radiation Risk (ECRR) the stage of radiation depends on the stage the body parts are affected
Exposure pathways
External


External exposure is exposure which occurs when the radioactive source (or other radiation source) is outside (and remains outside) the organism which is exposed. Examples of external exposure include:
- A person who places a sealed radioactive source in his pocket
- A space traveller who is irradiated by cosmic rays
- A person who is treated for teletherapy or brachytherapy. While in brachytherapy the source is inside the person it is still considered external exposure because it does not result in a committed dose.
- A nuclear worker whose hands have been dirtied with radioactive dust. Assuming that his hands are cleaned before any radioactive material can be absorbed, inhaled or ingested, skin contamination is considered to be external exposure.
External exposure is relatively easy to estimate, and the irradiated organism does not become radioactive, except for a case where the radiation is an intense neutron beam which causes activation.
By type of medical imaging
| Target organs | Exam type | Effective dose in adults[14] | Equivalent time of background radiation[14] |
|---|---|---|---|
| CT of the head | Single series | 2 mSv | 8 months |
| With + without radiocontrast |
4 mSv | 16 months | |
| Chest | CT of the chest | 7 mSv | 2 years |
| CT of the chest, lung cancer screening protocol | 1.5 mSv | 6 months | |
| Chest X-ray | 0.1 mSv | 10 days | |
| Heart | Coronary CT angiography | 12 mSv | 4 years |
| Coronary CT calcium scan | 3 mSv | 1 year | |
| Abdominal | CT of abdomen and pelvis | 10 mSv | 3 years |
| CT of abdomen and pelvis, low dose protocol | 3 mSv[15] | 1 year | |
| CT of abdomen and pelvis, with + without radiocontrast |
20 mSv | 7 years | |
| CT Colonography | 6 mSv | 2 years | |
Intravenous pyelogram |
3 mSv | 1 year | |
| Upper gastrointestinal series | 6 mSv | 2 years | |
| Lower gastrointestinal series | 8 mSv | 3 years | |
| Spine | Spine X-ray | 1.5 mSv | 6 months |
| CT of the spine | 6 mSv | 2 years | |
| Extremities | X-ray of extremity | 0.001 mSv | 3 hours |
| Lower extremity CT angiography |
0.3 - 1.6 mSv[16] | 5 weeks - 6 months | |
| Dental X-ray | 0.005 mSv | 1 day | |
| DEXA (bone density) | 0.001 mSv | 3 hours | |
| PET-CT combination | 25 mSv | 8 years | |
| Mammography | 0.4 mSv | 7 weeks | |
Internal
Internal exposure occurs when the radioactive material enters the organism, and the radioactive atoms become incorporated into the organism. This can occur through inhalation, ingestion, or injection. Below are a series of examples of internal exposure.
- The exposure caused by potassium-40 present within a normal person.
- The exposure to the ingestion of a soluble radioactive substance, such as cows' milk.
- A person who is being treated for cancer by means of a fission products within a uranium dioxidematrix might never be able to truly become part of an organism, it is normal to consider such particles in the lungs and digestive tract as a form of internal contamination which results in internal exposure.
- cytotoxic) effect which is lethal (within a limited range of 5-9 micrometers or approximately one cell diameter). Clinical trials, with promising results, are currently carried out in Finland and Japan.
When radioactive compounds enter the human body, the effects are different from those resulting from exposure to an external radiation source. Especially in the case of alpha radiation, which normally does not penetrate the skin, the exposure can be much more damaging after ingestion or inhalation. The radiation exposure is normally expressed as a committed dose.
History
Although radiation was discovered in late 19th century, the dangers of radioactivity and of radiation were not immediately recognized. Acute effects of radiation were first observed in the use of
As a field of medical sciences, radiobiology originated from
The genetic effects of radiation, including the effects on cancer risk, were recognized much later. In 1927
More generally, the 1930s saw attempts to develop a general model for radiobiology. Notable here was Douglas Lea,[19][20] whose presentation also included an exhaustive review of some 400 supporting publications.[21][page needed][22]
Before the biological effects of radiation were known, many physicians and corporations had begun marketing radioactive substances as patent medicine and radioactive quackery. Examples were radium enema treatments, and radium-containing waters to be drunk as tonics. Marie Curie spoke out against this sort of treatment, warning that the effects of radiation on the human body were not well understood. Curie later died of aplastic anemia caused by radiation poisoning. Eben Byers, a famous American socialite, died of multiple cancers (but not acute radiation syndrome) in 1932 after consuming large quantities of radium over several years; his death drew public attention to dangers of radiation. By the 1930s, after a number of cases of bone necrosis and death in enthusiasts, radium-containing medical products had nearly vanished from the market.
In the United States, the experience of the so-called
The atomic bombings of Hiroshima and Nagasaki resulted in a large number of incidents of radiation poisoning, allowing for greater insight into its symptoms and dangers. Red Cross Hospital surgeon Dr. Terufumi Sasaki led intensive research into the Syndrome in the weeks and months following the Hiroshima bombings. Sasaki and his team were able to monitor the effects of radiation in patients of varying proximities to the blast itself, leading to the establishment of three recorded stages of the syndrome. Within 25–30 days of the explosion, the Red Cross surgeon noticed a sharp drop in white blood cell count and established this drop, along with symptoms of fever, as prognostic standards for Acute Radiation Syndrome.[25] Actress Midori Naka, who was present during the atomic bombing of Hiroshima, was the first incident of radiation poisoning to be extensively studied. Her death on August 24, 1945, was the first death ever to be officially certified as a result of radiation poisoning (or "atomic bomb disease").
The Atomic Bomb Casualty Commission and the Radiation Effects Research Foundation have been monitoring the health status of the survivors and their descendants since 1946. They have found that radiation exposure increases cancer risk, but also that the average lifespan of survivors was reduced by only a few months compared to those not exposed to radiation. No health effects of any sort have thus far been detected in children of the survivors.[26]
Areas of interest
The interactions between organisms and electromagnetic fields (EMF) and ionizing radiation can be studied in a number of ways:
- Radiation physics
- Radiation chemistry
- Molecular and cell biology
- Molecular genetics
- Cell death and apoptosis
- High and low-level electromagnetic radiation and health
- Specific absorption rates of organisms
- Radiation poisoning
- Radiation oncology (radiation therapy in cancer)
- Bioelectromagnetics
- Electric field and Magnetic field - their general nature.
- Electrophysiology - the scientific study of the electrical properties of biological cells and tissues.
- Biomagnetism - the magnetic properties of living systems (see, for example, the research of David Cohen using SQUID imaging) and Magnetobiology - the study of effect of magnets upon living systems. See also Electromagnetic radiation and health
- Bioelectromagnetism - the electromagnetic properties of living systems and Bioelectromagnetics- the study of the effect of electromagnetic fields on living systems.
- Electrotherapy
- Radiation therapy
- Radiogenomics
- Transcranial magnetic stimulation - a powerful electric current produces a transient, spatially focussed magnetic field that can penetrate the scalp and skull of a subject and induce electrical activity in the neurons on the surface of the brain.
- Magnetic resonance imaging - a very powerful magnetic field is used to obtain a 3D image of the density of water molecules of the brain, revealing different anatomical structures. A related technique, functional magnetic resonance imaging, reveals the pattern of blood flow in the brain and can show which parts of the brain are involved in a particular task.
- Embryogenesis, Ontogeny and Developmental biology- a discipline that has given rise to many scientific field theories.
- Bioenergetics - the study of energy exchange on the molecular level of living systems.
- Biological psychiatry, Neurology, Psychoneuroimmunology
Radiation sources for experimental radiobiology
Radiobiology experiments typically make use of a radiation source which could be:
- An .
- A , focused down to cellular or subcellular sizes.
- A UV lamp.
See also
- Biological effects of radiation on the epigenome
- Cell survival curve
- Health threat from cosmic rays
- NASA Space Radiation Laboratory
- Radioactivity in biology
- Radiology
- Radiophobia
- Radiosensitivity
References
- ^ ICRP 2007, p. 49, paragraph 55.
- ^ PMID 24275177.Note: first page available free at URL.
- ^ ICRP 2007, p. 55, Paragraph 83.
- ^ "Do CT scans cause cancer?". Harvard Health Publishing. Harvard University. March 2013. Retrieved 15 Jul 2020. Note: First paragraph provided free.
- ISBN 978-0-309-09156-5. Retrieved 11 Nov 2013.
- ^ "Radiation Exposure and Contamination - Injuries; Poisoning - Merck Manuals Professional Edition". Merck Manuals Professional Edition. Retrieved 6 Sep 2017.
- PMID 19047611.
- PMID 19047611.
- ^ American Congress of Obstetricians and Gynecologists. February 2016
- PMID 15642178.
- ^ ICRP 2007, p. 73, paragraph 144.
- ^ ICRP 2007, p. 24, glossary.
- ^ ICRP 2007, pp. 61–62, paragraphs 104 and 105.
- ^ RadiologyInfo.org by Radiological Society of North America. Retrieved 23 Oct 2017.
- PMID 27578040.
- PMID 24915439.
- PMID 11749482.
- ISBN 9781600212802. Page xxi.
- S2CID 250827449.
- ^ Lea, Douglas E. "Radiobiology in the 1940s". British Institute of Radiology. Retrieved 15 Jul 2020.
- ISBN 9781001281377.
- PMC 1932419.
- ^ Grady, Denise (6 October 1998). "A Glow in the Dark, and a Lesson in Scientific Peril". The New York Times. Retrieved 25 Nov 2009.
- OSTI 751062. Retrieved 24 May 2012.
- ISBN 978-0-88363-991-7.
- ^ "Long-term health effects of Hiroshima and Nagasaki atomic bombs not as dire as perceived". Science Daily. 11 August 2016. Retrieved 16 Oct 2021.
- S2CID 8711325. Archived from the original(PDF) on 16 Jul 2020.
Sources
- ICRP, 2007. The 2007 Recommendations of the International Commission on Radiological Protection. ICRP Publication 103. Ann. ICRP 37 (2-4).
Further reading
- Eric Hall, Radiobiology for the Radiologist. 2006. Lippincott
- G.Gordon Steel, "Basic Clinical Radiobiology". 2002. Hodder Arnold.
- The Institute for Radiation Biology at the Helmholtz-Center for Environmental Health [1]
