Sexual differentiation in humans

Sexual differentiation in humans is the process of development of
The development of sexual differences begins with the
Disorders of sexual development (DSD), encompassing conditions characterized by the appearance of undeveloped genitals that may be ambiguous, or look like those typical for the opposite sex, sometimes known as intersex, can be a result of genetic and hormonal factors.[4]
Sex determination
Most
Chromosomal sex is determined at the time of
Six weeks elapse after fertilization before the first signs of sex differentiation can be observed in human embryos.
Reproductive system
This article needs additional citations for verification. (October 2021) |
![Figure One: The mesonephric System Pathway [7]](http://upload.wikimedia.org/wikipedia/commons/thumb/c/c7/SRY_Gene_Pathway.jpg/500px-SRY_Gene_Pathway.jpg)
Differentiation between the sexes of the sex organs occurs throughout embryological, fetal and later life. In both males and females, the sex organs consist of two structures: the internal genitalia and the external genitalia. In males, the gonads are the
As the zygote divides, it first becomes the embryo (which means 'growing within'), typically between zero and eight weeks, then from the eighth week until birth, it is considered the fetus (which means 'unborn offspring'). The internal genitalia are all the accessory glands and ducts that connect the gonads to the outside environment. The external genitalia consist of all the external reproductive structures. The sex of an early embryo cannot be determined because the reproductive structures do not differentiate until the seventh week. Prior to this, the child is considered bipotential because it cannot be identified as male or female.
Internal genital differentiation
The internal genitalia consist of two accessory ducts: mesonephric ducts (Woffian duct) and paramesonephric ducts (Müllerian ducts). The mesonephric system is the precursor to the male genitalia and the paramesonephric to the female reproductive system.[8] As development proceeds, one of the pairs of ducts develops while the other regresses. This depends on the presence or absence of the sex determining region of the Y chromosome, also known as the SRY gene.[5] In the presence of a functional SRY gene, the bipotential gonads develop into testes. Gonads are histologically distinguishable by 6–8 weeks of gestation.
Subsequent development of one set and degeneration of the other depends on the presence or absence of two testicular hormones: testosterone and anti-Müllerian hormone (AMH). Disruption of typical development may result in the development of both, or neither, duct system, which may produce morphologically intersex individuals.
Males: The SRY gene when transcribed and processed produces SRY protein that binds to DNA and directs the development of the gonad into testes. Male development can only occur when the fetal testis secretes key hormones at a critical period in early gestation. The testes begin to secrete three hormones that influence the male internal and external genitalia: they secrete anti-Müllerian hormone (AMH),
Females: Without testosterone and AMH, the mesonephric ducts degenerate and disappear. The paramesonephric ducts develop into the
External genital differentiation
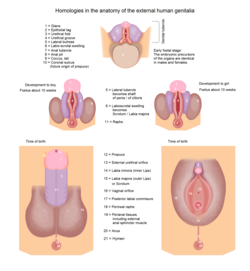
By 7 weeks, a fetus has a
A sufficient amount of any androgen can cause external
Further sex differentiation of the external genitalia occurs at puberty, when androgen levels again become disparate. Male levels of testosterone directly induce growth of the penis, and indirectly (via DHT) the prostate.
Secondary sexual characteristics
This section needs expansion. You can help by adding to it. (January 2020) |
Breast development
Visible differentiation occurs at puberty, when estradiol and other hormones cause breasts to develop in typical females.
Psychological and behavioral differentiation
Human adults and children show many psychological and behavioral sex differences. Some (e.g. dress) are learned and cultural. Others are demonstrable across cultures and have both biological and learned determinants. For example, some studies claim girls are, on average, more verbally fluent than boys, but boys are, on average, better at spatial calculation.[14] It seems likely that this is due to males generally having a greater area allocated to the space-specialized parietal cortex, while females generally have relatively more brain area allocated to the verbal-associative-specialized temporal cortex.[15]
Disorders of sex development
Disorders of sex determination (DSD) are classified into a multitude of categories.[16] These categories consists of different types of female disorders along with categories specifically for male DSDs. There are also sex chromosomal DSDs such as, the later mentioned, Klinefelter and Turner syndrome[16]
The following are some of the conditions associated with atypical determination and differentiation process:[17]
- A zygote with only X chromosome (XO) results in Turner syndrome and will develop with female characteristics.[5]
- Congenital adrenal hyperplasia –Inability of adrenal to produce sufficient cortisol, leading to increased production of testosterone resulting in severe masculinization of 46 XX females. The condition also occurs in XY males, as they suffer from the effects of low cortisol and salt-wasting, not virilization.
- Persistent Müllerian duct syndrome – A rare type of pseudohermaphroditism that occurs in 46 XY males, caused by either a mutation in the Müllerian inhibiting substance (MIS) gene, on 19p13, or its type II receptor, 12q13. Results in a retention of Müllerian ducts (persistence of rudimentary uterus and fallopian tubes in otherwise normally virilized males), unilateral or bilateral undescended testes, and sometimes causes infertility.
- XY differences of sex development – Atypical androgen production or inadequate androgen response, which can cause incomplete masculinization in XY males. Varies from mild failure of masculinization with undescended testes to complete sex reversal and female phenotype (Androgen insensitivity syndrome)
- SRYgenes.
- A androgeniceffects farther from the site of testosterone production, where the concentrations of testosterone are too low to have any potency.
- Klinefelter syndrome (47,XXY)- A chromosomal disorder that results in an extra X chromosome in males. This leads to hormonal problems later on. However, this disorder while in some cases easily identified, sometimes is not extreme and can not be determined until after puberty if at all.[18]
Timeline
| Fetal age (weeks) |
Crown-rump length (mm) |
Sex differentiating events |
|---|---|---|
| 1 | blastocyst | X-inactivation, if more than one X chromosome present[20] |
| 4 | 2–3 | Development of Wolffian ducts
|
| 5 | 7 | Migration of primordial germ cells in the undifferentiated gonad |
| 6 | 10–15 | Development of Müllerian ducts
|
| 7 | 13–20 | Male: Differentiation of seminiferous tubules
|
| 8 | 30 | Male: Regression of Müllerian ducts |
| 8 | 32–35 | Male: Appearance of Leydig cells. First synthesis of testosterone
|
| 9 | 43 | Male: Total regression of Müllerian ducts. Female: Loss of sensitivity of Müllerian ducts in the female fetus |
| 9 | 43 | Female: First meiotic prophase in oogonia |
| 10 | 43–45 | Male: Beginning of masculinization of external genitalia |
| 10 | 50 | Female: Beginning of regression of Wolffian ducts |
| 12 | 70 | Male: Fetal inguinal ring
|
| 12–14 | 70–90 | Male: Penile urethra is completed |
| 14 | 90 | Male: Appearance of first spermatogonia |
| 16 | 100 | Female: Appearance of first ovarian follicles
|
| 17 | 120 | Male: Numerous Leydig cells. Peak of testosterone secretion |
| 20 | 150 | Male: Regression of Leydig cells. Diminished testosterone secretion |
| 24 | 200 | Female: First multilayered ovarian follicles. Canalisation of the vagina |
| 28 | 230 | Female: Cessation of oogonia multiplication |
| 28 | 230 | Male: Descent of testis |
See also
References
- ^ PMID 11459768.
- ^ Sizonenko, P. C. (n.d.). "Human sexual differentiation". Reproductive health – via Geneva Foundation for Medical Education and Research.
- S2CID 25732504.
- PMID 16160410.
- ^ .
- ISBN 978-0-07-147693-5.
- ^ Silverthorn, Dee, U.. (2010). Reproduction and Development. In: Human Physiology: an integrated approach. 5th ed. san francisco: Pearson education. pp. 828–831.
- ^ "Learning Objectives". Albany.edu. Archived from the original on 3 May 2001. Retrieved 2 October 2017.
- ^ ISBN 978-0-07-147693-5 – via Internet Archive.
- ISBN 978-0-4650-4792-5.
- ^ Wilson, Danielle; Bordoni, Bruno (2025). "Embryology, Mullerian Ducts (Paramesonephric Ducts)". StatPearls. StatPearls Publishing.
- ^ Hughes, Ieuan A. . (June 12, 2011).[full citation needed]
- PMID 4399057.
- ]
- ]
- ^ PMID 29503125.
- PMID 14736929.
- ^ "Klinefelter syndrome: MedlinePlus Genetics". medlineplus.gov. Retrieved 17 April 2025.
- ^ PC Sizonenko in Pediatric Endocrinology, edited by J. Bertrand, R. Rappaport, and PC Sizonenko, (Baltimore: Williams & Wilkins, 1993), pp. 88–99
- PMID 37399516.
Further reading
- De Felici, M. (2010). "Germ stem cells in the mammalian adult ovary: Considerations by a fan of the primordial germ cells". Molecular Human Reproduction. 16 (9): 632–636. PMID 20086005.
- Sharman, GB; Hughes, RL; Cooper, DW (1989). "The Chromosomal Basis of Sex-Differentiation in Marsupials". Australian Journal of Zoology. 37 (3): 451. .
- Watson, CM; Margan, SH; Johnston, PG (1998). "Sex-chromosome elimination in the bandicoot Isoodon macrourus using Y-linked markers". Cytogenetics and Cell Genetics. 81 (1): 54–59. S2CID 20042866.

