Hidradenitis suppurativa
| Hidradenitis suppurativa | |
|---|---|
| Other names | Acne inversa, apocrine acne, Verneuil's disease, Velpeau's disease immunosuppressive medication[2] |
| Frequency | 1–4% of people, when mild cases are included[2][3] |
| Deaths | Rare[1] |


Hidradenitis suppurativa (HS), sometimes known as acne inversa or Verneuil's disease, is a long-term
The exact cause is usually unclear, but believed to involve a combination of
No cure is known,
If mild cases of HS are included, then the estimate of its frequency is from 1–4% of the population.[2][3] Women are three times more likely to be diagnosed with it than men.[2] Onset is typically in young adulthood and may become less common after 50 years old.[2] It was first described between 1833 and 1839 by French anatomist Alfred Velpeau.[1][12]
Terminology
Although hidradenitis suppurativa is often referred to as acne inversa, it is not a form of acne, and lacks the core defining features of acne such as the presence of closed
Causes
The exact cause of hidradenitis suppurativa remains unknown,[11][14] and there has, in the recent past, been notable disagreement among experts in this regard.[15] The condition, however, likely stems from both genetic and environmental causes.[3] Specifically, an immune-mediated pathology has been proposed,[11] although environmental factors have not been ruled out.[3]
Lesions will occur in any body areas with hair follicles,[15] and/or sweat glands,[16] although areas such as the axilla, groin, and perineal region are more commonly involved. This theory includes most of these potential indicators:[17]
- Post-pubescent individuals[18]
- Blocked hair follicles or blocked apocrine sweat glands
- Excessive sweating
- Androgen dysfunction
- Genetic disorders that alter cell structure
The historical understanding of the disease suggests dysfunctional apocrine glands[19] or dysfunctional hair follicles,[20] possibly triggered by a blocked gland, which creates inflammation, pain, and a swollen lesion.
Triggering factors
Several triggering factors should be taken into consideration:
- skin maceration.
- Tight clothing,[21] and clothing made of heavy, nonbreathable materials[23]
- Hot and especially humid climates.[29]
- Stress[27]
Predisposing factors
- autosomal dominant inheritance pattern has been proposed.[30]
- hormones.[31] Women often have outbreaks before their menstrual period and after pregnancy; HS severity usually decreases during pregnancy and after menopause.
Some cases have been found to result from mutations in the
Diagnosis
Early diagnosis is essential in avoiding tissue damage. However HS is often misdiagnosed or diagnosed late due to healthcare professionals not being aware of the condition or people not consulting with a physician.[34][35] Globally, the diagnosis is delayed more than 7 years in average after symptoms appear. This is much longer than with other skin conditions.[36]
Stages


Hidradenitis suppurativa presents itself in three stages.[19][38] Due to the large spectrum of clinical severity and the severe impact on quality of life, a reliable method for evaluating HS severity is needed.[citation needed]
Hurley's staging system
Hurley's staging system was the first classification system proposed, and is still in use for the classification of patients with skin diseases (i.e.,
| Stage | Characteristics |
|---|---|
| I | Solitary or multiple isolated abscess formation without scarring or sinus tracts (A few minor sites with rare inflammation; may be mistaken for acne .)
|
| II | Recurrent abscesses, single or multiple widely separated lesions, with sinus tract formation (Frequent inflammation restricts movement and may require minor surgery such as incision and drainage .)
|
| III | Diffuse or broad involvement across a regional area with multiple interconnected sinus tracts and abscesses (Inflammation of sites to the size of golf balls, or sometimes baseballs; scarring develops, including subcutaneous tracts of infection – see fistula. Obviously, patients at this stage may be unable to function.) |
Sartorius staging system
The Sartorius staging system is more sophisticated than Hurley's. Sartorius et al. suggested that the Hurley system is not sophisticated enough to assess treatment effects in clinical trials during research. This classification allows for better dynamic monitoring of the disease severity in individual patients. The elements of this staging system are:[40]
- Anatomicregions involved (axilla, groin gluteal, or other region or inframammary region left or right)
- Number and types of fistulasor sinuses, scars, points for lesions of all regions involved)
- The distance between lesions, in particular the longest distance between two relevant lesions (i.e., nodules and fistulas in each region or size if only one lesion present)
- The presence of normal skin in between lesions (i.e., if all lesions are clearly separated by normal skin)
Points are accumulated in each of the above categories, and added to give both a regional and total score. In addition, the authors recommend adding a visual analog scale for pain or using the dermatology life quality index (DLQI, or the 'skindex') when assessing HS.[41]
Treatment
Treatment depends upon presentation and severity of the disease. Due to the poorly studied nature of the disease, the effectiveness of drugs and therapies were unclear.[42] Clear and sensitive communication from health care professionals, social and psychological interventions can help managing the emotional impact of the condition and aid necessary lifestyle changes.[34][35] In May 2023, the European Commission (EC) approved Cosentyx (secukinumab) for active moderate to severe hidradenitis suppurativa in adults.[43]
Other possible treatments include the following:
Cryotherapy
Cryotherapy has demonstrated efficacy against the disease, with 88% of persistent lesions resolving in a clinical trial of 23 patients.[44]
Lifestyle
Warm baths may be tried in those with mild disease.[4] Weight loss and the cessation of smoking are also recommended.[2]
Medication
- Antibiotics: taken by mouth, these are used for their anti-inflammatory properties rather than to treat infection. Most effective is a combination of rifampicin and clindamycin given concurrently for 2–3 months. Popular antibiotics also include tetracycline and minocycline.[45] Topical clindamycin has been shown to have an effect in double-blind placebo controlled studies.[46] In a retrospective review and telephone survey, intravenous ertapenem therapy showed clinical improvement with 80.3% of subjects reporting medium to high satisfaction and 90.8% would recommend ertapenem to other patients.[47]
- Corticosteroid injections, also known as intralesional steroids, can be particularly useful for localized disease, if the drug can be prevented from escaping via the sinuses.
- TNF-alpha) drugs such as infliximab, and etanercept[51] This use of these drugs is not currently Food and Drug Administration(FDA) approved and is somewhat controversial, so may not be covered by insurance.
- TNF inhibitor: Studies have supported that various TNF inhibitors have a positive effect on HS lesions.[52] Specifically adalimumab at weekly intervals is useful.[53] Adalimumab is the only medication approved by the FDA for the treatment of HS as of 2021.
- Topical acne vulgaris. Individuals affected by HS who responded to isotretinoin treatment tended to have milder cases of the condition.[54]
- Zinc and Nicotinamide, at doses of 90 mg and 30 mg respectively, have shown efficacy against mild to moderate hidradenitis suppurativa in a controlled retrospective clinical trial.[55]
Surgery
When the process becomes chronic, wide surgical excision is the procedure of choice.
Wounds in the affected area do not heal by
Laser hair removal
The 1064-
Prognosis

Potential complications
- axillae due to fibrosis and scarring occur. Severe lymphedemamay develop in the lower limbs.
- Local and systemic , etc.), are seen, which may even progress to sepsis.
- higher risk for diabetes mellitus[61]
- Interstitial keratitis
- Anal, rectal, or urethral fistulae[62]
- Normochromic or hypochromic anemia[63]
- People with HS may be at increased risk for autoimmune disorders including ankylosing spondylitis, rheumatoid arthritis, and psoriatic arthritis.[64]
- tumorsare usually highly aggressive.
- Tumors of the oral cavity, and liver cancer[66]
- Hypoproteinemia and amyloidosis, which can lead to kidney failure and death[67]
- Seronegative and usually asymmetric polyarthralgia syndrome[68]
Impact on mental health
HS is a painful and socially isolating condition which leads to a negative impact on mental health as well. 21% of people with HS have depression and 12% have anxiety.[69] People with HS also have a higher risk of attempting suicide.[70]
Epidemiology
Prevalence
Estimates of the prevalence of HS vary worldwide and there is no accepted generalization. In the USA, the prevalence is estimated to be 0.1% while in Europe it is thought to be 1% or more.[70]
Gender
In North America and Europe, women are three times more likely to have HS. However, in South Korea, men are twice as likely to have HS.[70]
Age
HS is the most prevalent in people in their 40s and 50s.[70]
History
- From 1833 to 1839, in a series of three publications, Velpeau identified and described a disease now known as hidradenitis suppurativa.[71]
- In 1854, Verneuil described hidradenitis suppurativa as hidrosadénite Phlegmoneuse. This is how HS obtained its alternate name "Verneuil's disease".[72]
- In 1922, Schiefferdecker hypothesized a pathogenic link between "acne inversa" and human sweat glands.[73]
- In 1956, Pillsbury et al.[74] coined the term follicular occlusion triad for the common association of hidradenitis suppurativa, acne conglobata and dissecting cellulitis of the scalp. Modern clinical research still employs Pillsbury's terminology for these conditions' descriptions.[75]
- In 1975, Plewig and Kligman, following Pillsbury's research path, modified the "acne triad", replacing it with the "acne tetrad: acne triad, plus pilonidal sinus".[76]Plewig and Kligman's research follows in Pillsbury's footsteps, offering explanations of the symptoms associated with hidradenitis suppurativa.
- In 1989, Plewig and Steger's research led them to rename hidradenitis suppurativa, calling it "acne inversa" – which is not still used today in medical terminology, although some individuals still use this outdated term.[77]
A surgeon from Paris, Velpeau described an unusual inflammatory process with formation of superficial
| Author | Year | Findings |
|---|---|---|
| Velpeau | 1839 | First description of the hidradenitis suppurativa |
| Verneuil | 1854 | "Hidrosadénite phlegmoneuse" |
| Pillsbury | 1956 | Acne triad (hidradenitis suppurativa, perifolliculitis capitis abscendens et suffodiens, acne congoblata) |
| Plewig & Kligman | 1975 | Acne tetrad (acne triad + pilonidal sinus) |
| Plewig & Steger | 1989 | Acne inversa |
Other names
Hidradenitis suppurativa has been referred to by multiple names in the literature, as well as in various cultures. Some of these are also used to describe different diseases, or specific instances of this disease.[38]
- Acne conglobata – not really a synonym – this is a similar process, but in classic acne areas of chest and back
- Acne inversa – a proposed new term[78][79] which has not gained widespread favor.[80]
- Apocrine acne – an outdated term based on the disproven[citation needed] concept that apocrine glands are primarily involved, though many do have apocrine gland infection
- Apocrinitis – another outdated term based on the same thesis
- Fox-den disease – a term not used in medical literature, based on the deep fox den–like sinuses
- Hidradenitis supportiva – a misspelling
- Pyodermia fistulans significa – now considered archaic
- Verneuil's disease – recognizing the surgeon whose name is most often associated with the disorder as a result of his 1854–1865 studies[81]
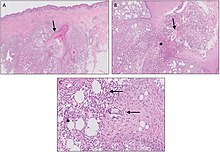
Histology
| Author | Year | Major Features |
|---|---|---|
| Plewig & Steger[77] | 1989 | Initial eccrine sweat glands secondarily involved.
|
| Yu & Cook[82] | 1990 | hair follicles are also inflamed.
|
| Boer & Weltevreden[83] | 1996 | Primary inflammation of the follicular infundibulum. Apocrine sweat glands are secondarily involved. |
Society and culture
Experiences of people with HS
HS can have a strong negative impact on people's lives, as well as physical and mental health. People with HS often feel stigmatised and embarrassed by their condition. Many try to hide the symptoms which can lead to impaired relationships and social isolation. A multidisciplinary approach by healthcare professionals, social support networks and psychological interventions can contribute to a better quality of life.[34][35] Compared to other skin diseases, HS has one of the highest Dermatology Life Quality Index (DLQI) scores.[84]
References
- ^ a b c d e f g h i "Hidradenitis Suppurativa". NORD (National Organization for Rare Disorders). 2012. Archived from the original on 19 February 2017. Retrieved 26 October 2017.
- ^ PMID 22236226.
- ^ a b c d e f g h i j k l m n "Hidradenitis suppurativa". Genetics Home Reference. December 2013. Archived from the original on 5 September 2017. Retrieved 27 October 2017.
- ^ a b c d e f "Hidradenitis suppurativa". rarediseases.info.nih.gov. 2017. Archived from the original on 28 July 2017. Retrieved 27 October 2017.
- ^ "Intergluteal contour deformity in hidradenitis suppurativa". Retrieved 18 May 2021.
- S2CID 169036038. Retrieved 18 May 2021.
- S2CID 201672889. Retrieved 18 May 2021.
- S2CID 25491238. Retrieved 18 May 2021.
- ^ "Psychosocial impact of hidradenitis suppurativa: a qualitative study". Retrieved 18 May 2021.
- ^ See section "Genetic Changes"[3]
- ^ a b c Pathophysiology of hidradenitis suppurativa (Seminal paper, SCMS Journal); NIH, National Library of Medicine, NCBI; 2017 Jun, 36(2):47–54.
- ISBN 978-3-540-33101-8. Archivedfrom the original on 28 October 2017.
- PMID 24767187.
- ^ See section "Genetic Changes"[3]
- ^ a b Medline Plus (2012). "Hidradenitis suppurativa". U.S. National Library of Medicine. Archived from the original on 16 September 2012. Retrieved 19 September 2012.
- ^ Hopkins Medicine Staff (2024). "Inflamed/Infected Sweat Glands (Hidradenitis)". Johns Hopkins Medicine. Retrieved 27 March 2024.
- ^ a b Schawartz's principles of surgery, 8th edition, self assessment and board review, chapter 15, the skin and subcutaneous tissue, question 16
- ^ Mayo Clinic Staff (2012). "Definition". Mayo Clinic. Archived from the original on 10 September 2012. Retrieved 19 September 2012.
- ^ a b DermNet acne/hidradenitis-suppurativa
- ^ "HSF – What is Hidradenitis Suppurativa? What is HS?". Archived from the original on 6 July 2007. Retrieved 8 July 2007.
- ^ PMID 12890458.
- ^ a b Jemec GBE. Body weight in hidradenitis suppurativa. In: Marks R, Plewig G, editors. Acne and Related disorders. London: Martin Dunitz; 1989. pp. 375–6.
- S2CID 25343489.
- S2CID 46448517.
- PMID 2492847.
- S2CID 207889793.
- ^ PMID 34440863.
- PMID 7829746.
- ^ Hidradenitis Suppurativa at eMedicine
- S2CID 35601570.
- S2CID 34410437.
- ^ Reference GH. "hidradenitis suppurativa". Genetics Home Reference. Archived from the original on 5 September 2017. Retrieved 5 September 2017.
- S2CID 231576248.
- ^ S2CID 246548949.
- ^ S2CID 235242411.
- S2CID 41589200.
- PMID 29713318.
- ^ a b "HS-USA :: What is Hidradenitis Suppurativa?". Archived from the original on 17 June 2013. Retrieved 20 July 2013.
- ^ Hurley HJ. Axillary hyperhidrosis, apocrine bromhidrosis, hidradenitis suppurativa, and familial benign pemphigus: surgical approach. In: Roenigk RK, Roenigk HH, editors. Dermatologic surgery. Marcel Dekker, New York, 1989, pp. 729–739.
- S2CID 46142606.
- PMID 17097366.
- PMID 26801356.
- ^ Sharma R (1 June 2023). "Novartis Cosentyx gets European Commission nod for use in adults with hidradenitis suppurativa". medicaldialogues.in. Retrieved 1 June 2023.
- PMID 37144039.
- PMID 24021361.
- S2CID 46661288.
- ^ {{Nosrati A, Ch'en PY, Torpey ME, Shokrian N, Ball G, Benesh G, Andriano TM, Zhu TR, Heibel HD, Hosgood HD, Campton KL, Cohen SR. Efficacy and Durability of Intravenous Ertapenem Therapy for Recalcitrant Hidradenitis Suppurativa. JAMA Dermatol. 2024 Feb 14:e236201. doi: 10.1001/jamadermatol.2023.6201. Epub ahead of print. PMID 38353987; PMCID: PMC10867774.}}
- ^ S2CID 149443722.
- ^ S2CID 204331143.
- PMID 31712062.
- S2CID 23743987.
- PMID 19997689.
- PMID 28355440.
- PMID 24765227.
- PMID 32339699.
- S2CID 21974148.
- from the original on 6 March 2014. Retrieved 4 March 2014.
- PMID 20855672.
- PMID 16488526.
- S2CID 33438993.
- PMID 37047569.
- ^ Hurley HJJ. Apocrine glands. New York: McGraw Hill; 1979.
- PMID 5667225.
- PMID 31968066.
- PMID 1952719.
- PMID 11405761.
- PMID 5953172.
- PMID 6241861.
- S2CID 214716227.
- ^ S2CID 221475227.
- ^ Velpeau A. Aissele. In: Bechet Jeune Z: Dictionnaire de médecine, on Repertoire Générale des Sciences Medicals sous le Rapport Theorique et Pratique. 1839.
- ^ Verneuil AS (1854). "Etudes sur les tumeurs de la peau et quelques maladies de glandes sudoripares" [Studies on skin tumors; some diseases of the sweat glands]. Archives of General Medicine (in French). 94: 693–705.
- ^ Schiefferdecker B (1922). Die Hautdrüsen der Menschen und der Säugetiere, ihre histologische und rassenanatomische Bedeutung sowie die muscularis sexualis [The skin glands of humans and mammals, their histological and anatomical racial meaning and muscularis sexualis]. Stuttgart: Schweizerbart E.[page needed]
- ^ Pillsbury DM, Shelley WB, Kligmann AM (1956). "Bacterial infections of the skin". In Pillsbury DM (ed.). Dermatoloy (1st ed.). Philadelphia. pp. 482–9.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ Triads in Dermatology; Prachi G Agrawal, Uday S Khopkar, [...], and Sunil N Mishra; Indian J Dermatol. 2013 Sep–Oct; 58(5): 346–351
- ISBN 978-3-642-96246-2.
- ^ a b Plewig G, Steger M (1989). "Acne inversa (alias acne triad, acne tetrad or hidradenitis suppurativa)". In Marks R, Plewig G (eds.). Acne and Related Disorders. London: Martin Dunitz. pp. 345–57.
- S2CID 34144101.
- S2CID 43108078.
- PMID 17459292.
- ^ Verneuil AS (1854). "Etudes sur les tumor de la peau". Arch Gen Med (in French). 94: 693.
- S2CID 8857181.
- PMID 8977671.
- S2CID 247006893.
External links
- Hidradenitis suppurativa at American Academy of Dermatology Association
- Hidradenitis suppurativa at British Association of Dermatologists
- Hidradenitis Suppurativa Foundation
